Case presentation
An 8-year-old female is brought into the Emergency Department by private vehicle after being run over by a car. The child was in her driveway when her father, who was backing the family van out of the garage, struck and ran over her. She is accompanied by both of her parents. The mother corroborates the father’s history. There is no reported loss of consciousness and the parents are sure that the child did not strike her head. There is no complaint of neck pain, chest pain, or difficulty breathing. She does complain of abdominal and lower back pain, but this has improved since the accident. Due to the history and her symptoms, the child is brought immediately to the trauma resuscitation bay.
Her physical examination reveals an afebrile child with a heart rate of 170 beats per minute, respiratory rate of 32 breaths per minute, a blood pressure of 87/56 mm Hg, and a room air oxygen saturation of 97%. Her Glasgow Coma Scale (GCS) score is 15. She is complaining of diffuse hip pain and bilateral lower leg pain. There are no signs of head, neck, chest, or abdominal trauma. A cervical collar is placed, given her other injuries. Her abdominal examination shows diffuse tenderness and bilateral lower quadrant guarding. She has multiple abrasions to the suprapubic area, bilateral lower abdominal quadrants, and the bilateral upper thighs. There is blood at the meatus. The vaginal area shows no other signs of trauma.
Imaging considerations
Imaging is indicated if there is suspicion, either by history or physical examination, of an intraabdominal injury (including bladder injury), significant microscopic hematuria, or gross hematuria. The amount of microscopic hematuria that is considered significant, prompting a clinician to obtain imaging, is a matter of debate and there is no universally accepted standard. Some authors have suggested that imaging is not indicated in patients with microscopic hematuria of less than 25 red blood cells per high-powered field.
Plain radiography
This imaging modality is readily available and is utilized as a first-line modality for suspected pediatric pelvic injuries. The standard view is anteroposterior (AP). Plain radiography can be used to diagnose pelvic fractures but may not demonstrate certain fractures well, such as those of the posterior pelvic ring, , and is less sensitive than computed tomography (CT). The detection of pelvic fractures on plain radiography may prompt the clinician to investigate for the presence of a bladder injury. Some authors recommend proceeding to CT if pelvic fractures are present. Other recommendations are to avoid routine pelvic radiography in low-risk pediatric patients: those who lack lower extremity injury, lack an abnormal physical examination of the pelvis and hip, lack abdominal pain, lack hematuria, have a GCS score of 13 or higher, are hemodynamically stable and have no need for abdominal/pelvis CT. , If a patient is to undergo CT of the abdomen/pelvis, plain radiography of the pelvis can be deferred.
Traditionally, plain radiographic or fluoroscopic cystography has been used to evaluate for the presence of a bladder injury. This study is performed by instilling iodinated contrast into the bladder and obtaining imaging to assess for contrast extravasation; postvoid imaging is important to avoid missing bladder injury and extravasation not evident on initial imaging. However, the density of contrast utilized for conventional (plain film or fluoroscopic) cystography will preclude performance of a CT of the abdomen and pelvis after the cystogram.
Computed tomography
CT is the imaging modality of choice for blunt or penetrating abdominal or genitourinary trauma. Standard CT imaging, though, is not adequate to diagnose bladder rupture. CT cystography, with retrograde filling of the bladder with very dilute iodinated contrast, is indicated for this purpose and is the preferred method over conventional cystography in patients undergoing CT imaging of the abdomen and pelvis for other injuries.
Authors have recommended CT cystography if certain injuries or findings are present: gross hematuria, pelvic free fluid on intravenous (IV) contrast–enhanced abdominal/pelvic CT, specific pelvic fractures (pubic symphysis diastasis, sacroiliac diastasis, and sacral, iliac, pubic rami fractures), and microscopic hematuria with pelvic fractures. , ,
Whichever method is utilized to perform cystography, the bladder should be fully distended. Instructions on how to perform a CT cystogram, and suggested bladder volumes for a cystogram, are presented later.
Magnetic resonance imaging (MRI)
MRI is not generally indicated in the acute evaluation of pediatric pelvic and genitourinary injuries. If there is severe allergy to IV contrast material, this modality can be considered in the trauma patient, but pediatric literature is lacking.
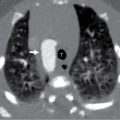
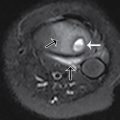
Imaging findings
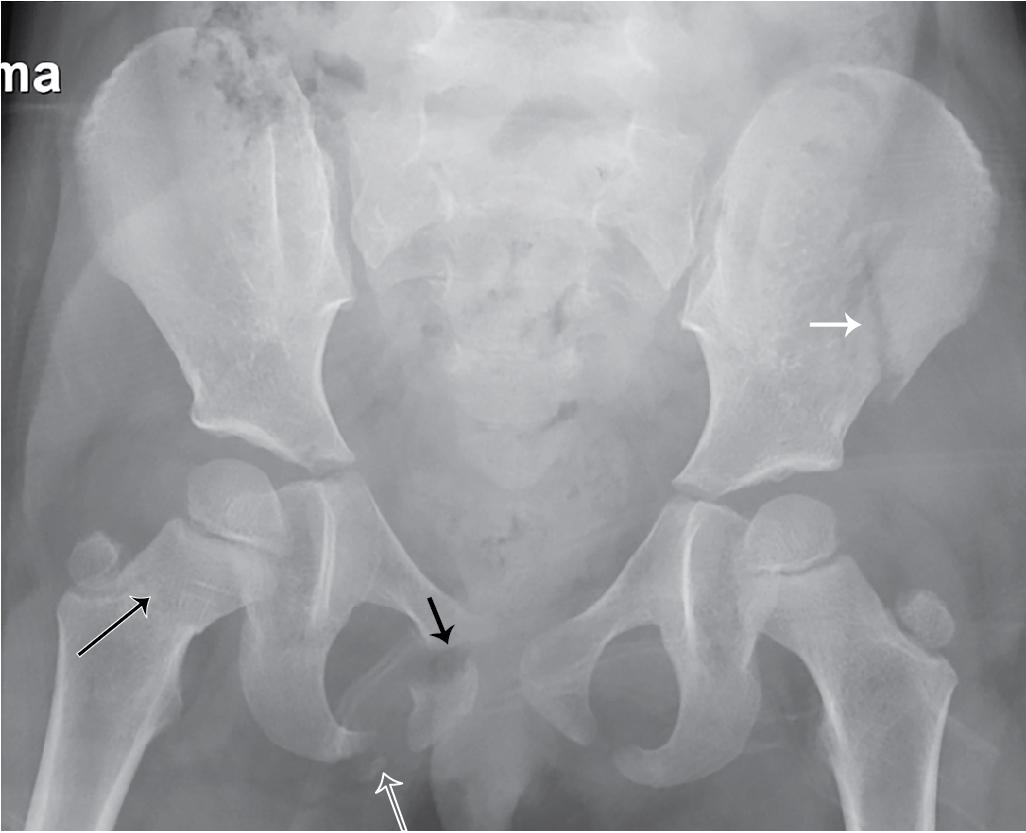
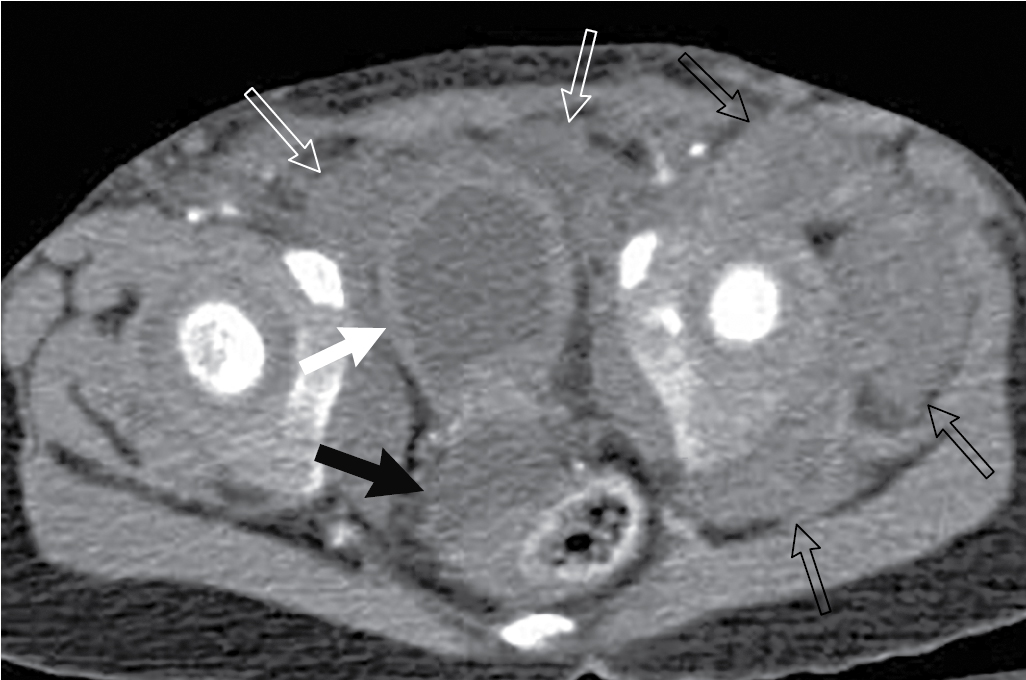
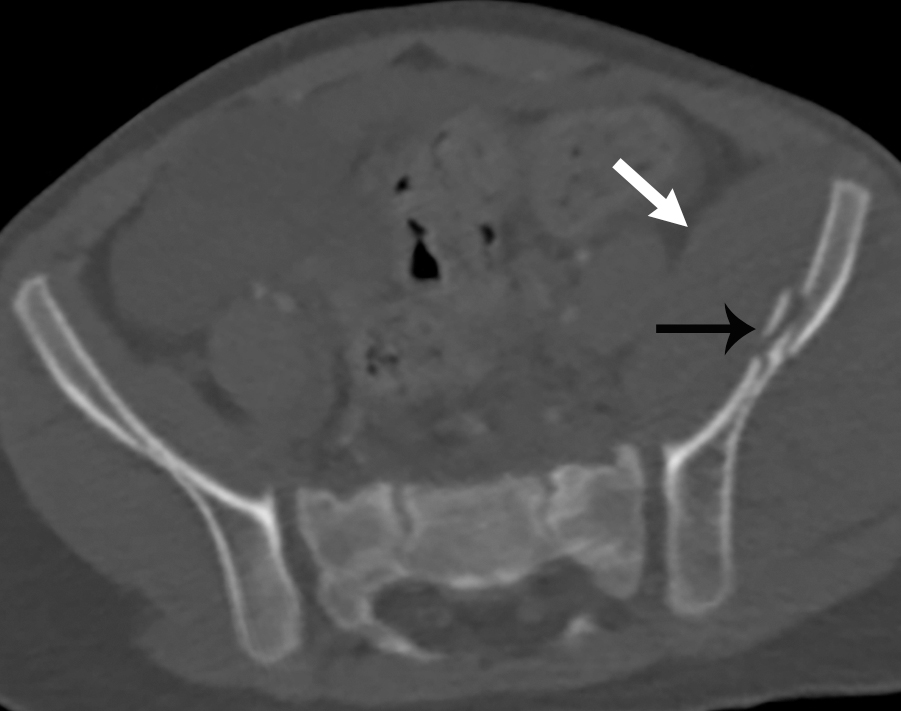
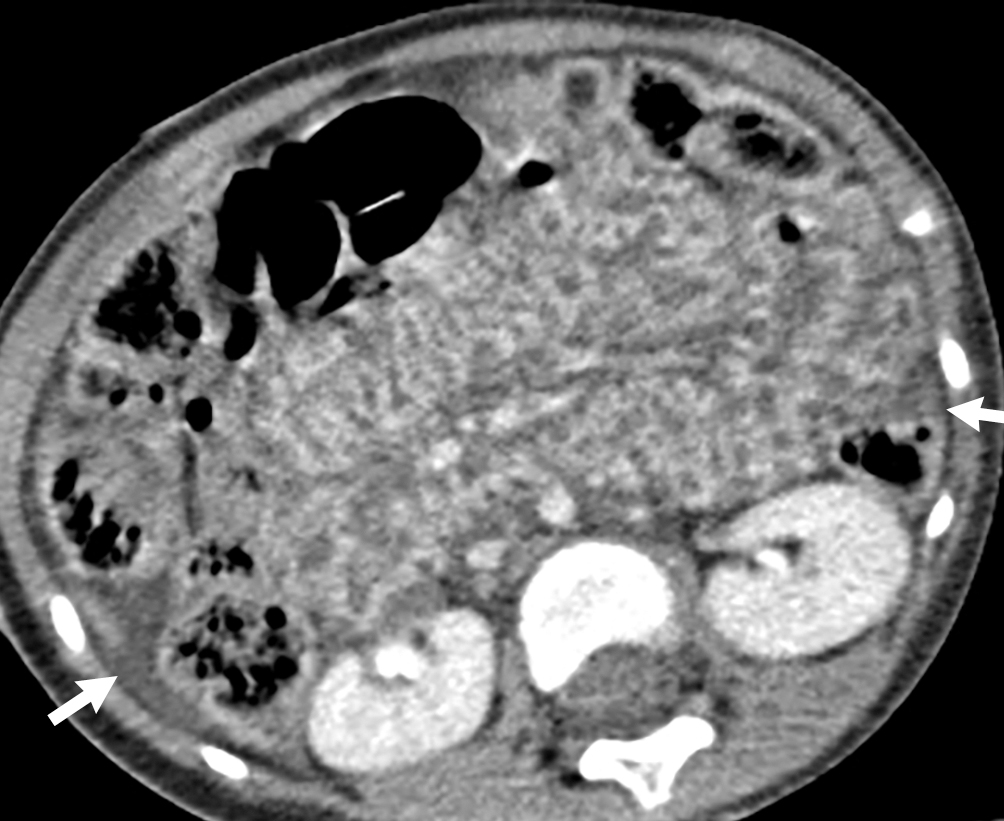
The child had an AP x-ray of the pelvis done. This image revealed multiple fractures, including fractures of the left iliac wing, the right symphysis pubis with diastasis of the symphysis pubis, fracture of the right inferior pubic ramus, and a right femoral neck fracture ( Fig. 43.1 ). These findings, plus the presence of gross hematuria, prompted CT imaging with IV contrast and CT cystography. This study demonstrated a rupture at the dome of the urinary bladder, best appreciated on the delayed images. The contrast leaks out into the peritoneal space. The bladder wall is markedly irregular and thickened ( Figs. 43.2–43.6 ).