The goals of tomographic imaging in evaluation of cardiac masses are the following:
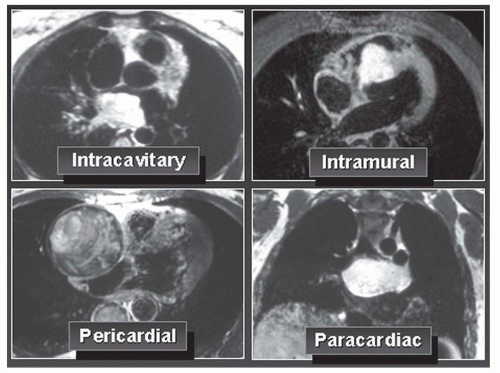
Identify an intracardiac or extracardiac mass.
Demonstrate the extent and invasiveness of the mass (staging of tumor).
Distinguish between benign and malignant tumor if possible.
Distinguish between primary and secondary tumor.
Distinguish between tumor and thrombus.
The term mass is used rather than tumor in this chapter because the most frequent mass within a cardiac chamber is thrombus rather than tumor. Primary tumors are rare. Secondary tumors, either metastatic or representing direct extension of primary tumors of another organ, are about 40 times more frequent than primary cardiac tumors.
Computed tomography (CT) and magnetic resonance imaging (MRI) can help determine the presence and extent of cardiac and paracardiac tumors. These modalities, especially MRI, can also sometimes characterize the mass. Although CT may be adequate for the evaluation of cardiac and paracardiac mass, MRI is usually employed for this purpose. Consequently, this chapter focuses on the findings on MRI.
Because of a wide field of view that encompasses the cardiovascular structures, mediastinum, and adjacent lung simultaneously, CT and MRI can display the intracardiac and extracardiac extent of tumors. In addition, the ability to image in multiple planes makes MRI especially suited for the demarcation of the spatial relationship of a mass to the various cardiac and mediastinal structures. Multiplanar images or reconstructions overcome the volume-averaging problem at the diaphragmatic interface encountered with a solely transaxial imaging plane. These features permit a clear delineation of the possible infiltration of a mass lesion into cardiac and adjacent mediastinal structures. MRI allows the assessment of functional parameters such as ventricular wall thickening, ejection fraction, or flow velocity in adjacent vessels. Therefore, the impact of a tumor on cardiac function can be evaluated.
In clinical practice, MRI and CT are most often used to verify or exclude a possible mass suggested initially by echocardiography. Echocardiography clearly depicts cardiac morphology and provides an assessment of functional parameters. The effectiveness of transthoracic echocardiography is limited by the acoustic window, however, which varies considerably with patient habitus. Image quality of echocardiography may be severely decreased by obesity or chronic obstructive pulmonary disease. Transesophageal echocardiography overcomes this problem but adds invasiveness. The soft tissue contrast achieved with echocardiography remains limited in comparison with that obtained with MRI and CT. Usually, pericardial involvement and infiltration of the myocardium can be better visualized with MRI and CT.
Tissue characterization based on specific T1 and T2 relaxation times is possible to a limited degree. Nevertheless, definitive differentiation between benign and malignant tumors is sometimes not possible. Most cardiac tumors have low to intermediate signal intensity on T1-weighted images and high signal intensity on T2-weighted images. However, the combination of imaging characteristics of a cardiac mass, such as location, signal intensity on T1- and T2-weighted images, possible hyperenhancement after the administration of paramagnetic contrast agents, and possible suppression of signal with the application of a fat-saturation technique, may render a specific tissue diagnosis highly probable in some cases.
BENIGN PRIMARY CARDIAC TUMORS
About 80% of primary cardiac tumors are benign (
Table 35-1). Although these tumors do not metastasize or invade locally, they may lead to significant morbidity and mortality by causing arrhythmias, valvular obstruction, or embolism. An intramyocardial location can interfere with normal conduction pathways and produce arrhythmias, obstruct coronary blood flow, or diminish compliance or contractility through replacement of myocardium. Both benign and malignant tumors have characteristic sites of origin (
Table 35-2).
Myxoma
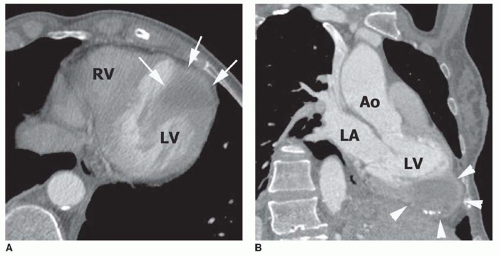
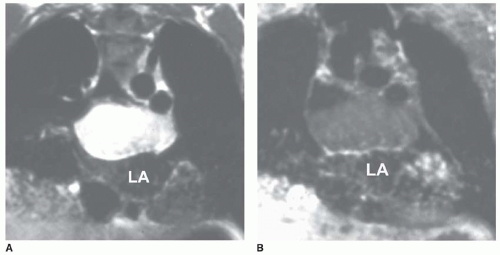
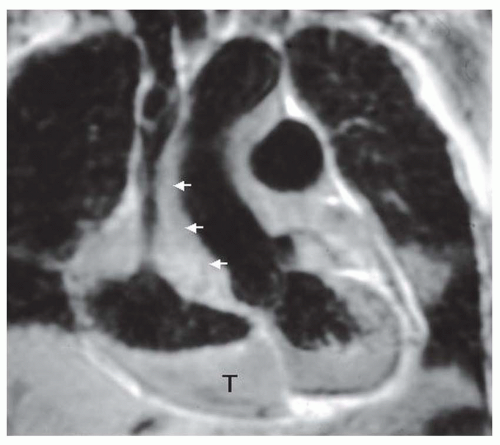
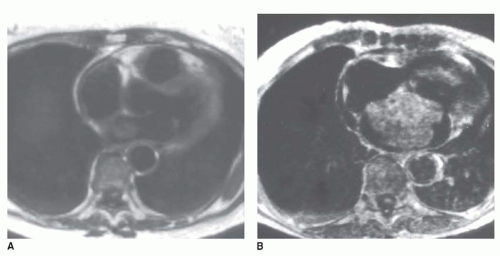
Myxoma is the most common benign cardiac tumor. It is located in the left atrium in 75% of cases and in the right atrium in 20% of cases. Multiple atrial myxomas may occur rarely, especially in Carney’s syndrome. This tumor is usually spherical, but the shape may vary during the cardiac cycle because of its gelatinous consistency. Left atrial myxomas are typically attached by a narrow pedicle to the area of the fossa ovalis (
Fig. 35-9, A). Infrequently, myxomas have a wide base of attachment to the atrial septum (see
Fig. 35-9, B). However, a wide mural attachment is more frequently encountered with malignant tumors. The extent of attachment may be difficult to assess for large tumors, which fill nearly the entire cavity so that they are compressed against the septum (
Fig. 35-9, B). As a result, the tumor appears to have broad contact with the atrial septum on static MR images. Myxomas can grow through a patent foramen ovale and extend into both atria, a condition that has been described
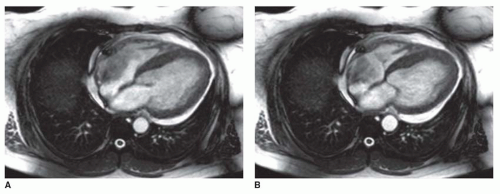
as a “dumbbell” appearance. Cine MRI permits an evaluation of tumor motion and may help to identify the site and length of attachment of the tumor to the wall or walls of the cardiac chambers. With this technique, myxomas have been shown to prolapse through the funnel of the atrioventricular valve (
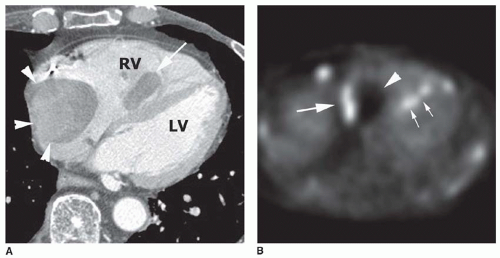
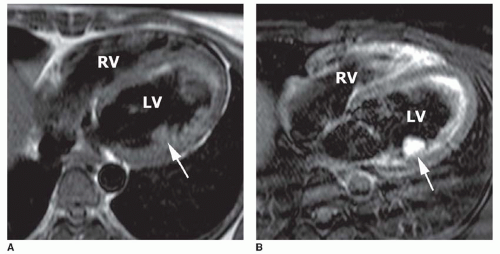
Fig. 35-10) or into the corresponding ventricle during diastole. Rarely, myxoma can have a wide point of attachment to ventricular endocardium (
Figs. 35-11 and
35-12).
Usually, myxomas display intermediate signal intensity (isointense to the myocardium) on T1-weighted SE images. On T2-weighted SE images, myxomas usually have higher signal intensity than myocardium. However, myxomas with very low signal intensity have also been observed. Fibrous stroma, calcification, and the deposition of paramagnetic iron following interstitial hemorrhage can reduce the signal intensity of the tumor on T2-weighted SE images. Rarely, myxomas have been reported to be invisible on SE images because of a lack of contrast with the dark blood pool. Such tumors can be delineated with cine MRI, on which they appear with high contrast against the surrounding bright blood. Most myxomas show increased signal intensity after the administration of Gd-DTPA on T1-weighted images (
Fig. 35-13) and on delayed gadolinium-enhanced images, which is probably secondary to an increased interstitial space and, therefore, a larger distribution volume of the contrast agent within the tumor than in normal tissue.
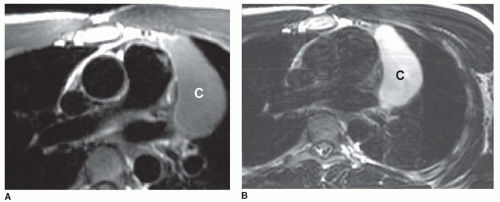
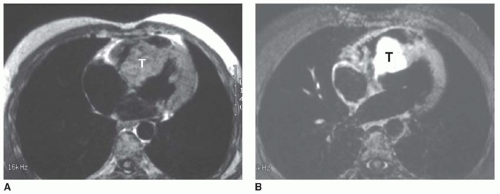
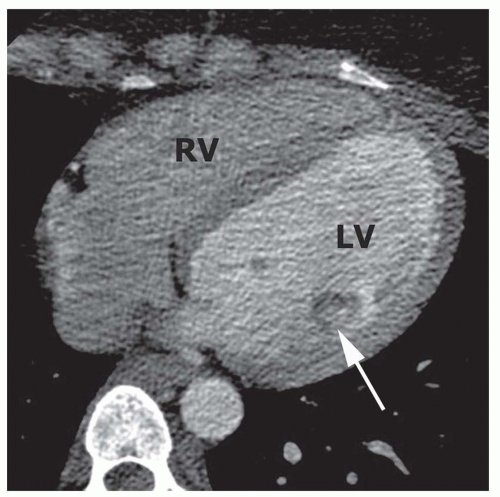
Lipoma and Lipomatous Hypertrophy of the Atrial Septum
Lipomas are reported to be the second most common benign cardiac tumor in adults but may actually be the most common. If the mass projects into the right atrium, it is called a lipoma, while lipomatous hypertrophy is confined to the atrial septum. They may occur at any age but are encountered most frequently in middle-aged and elderly adults. Lipomas consist of encapsulated mature adipose cells and fetal fat cells. The tumor consistency is soft, and lipomas may grow to a large size without causing symptoms. Lipomas are typically located in the right atrium (
Fig. 35-14) or atrial septum. They arise from the endocardial surface and have a broad base of attachment. Lipomas have the same signal intensity as subcutaneous and epicardial fat on all MRI sequences. Because fat has a short T1 relaxation time, lipomas have high signal intensity on T1-weighted images, which can be suppressed with fat-saturating pulse sequences (see
Fig. 35-14). Usually, they appear with homogeneous signal intensity but may have a few thin septations. They do not enhance after the administration of contrast. On T2-weighted images, lipomas have intermediate signal intensity.


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access