- The structure and mechanical function of the cardiac chambers and valves
- Myocardial tissue characteristics, e.g. presence of myocardial scar and/or oedema
- Presence of stress-induced, reversible or irreversible perfusion defects in the myocardium
- Patency of the coronary arteries
Plain Chest Radiography
Plain chest radiographic evidence of heart disease may be given by the size and shape of the heart together with any cardiac calcification, and by the size of pulmonary vessels and the presence of pulmonary oedema.
Heart Size and Shape
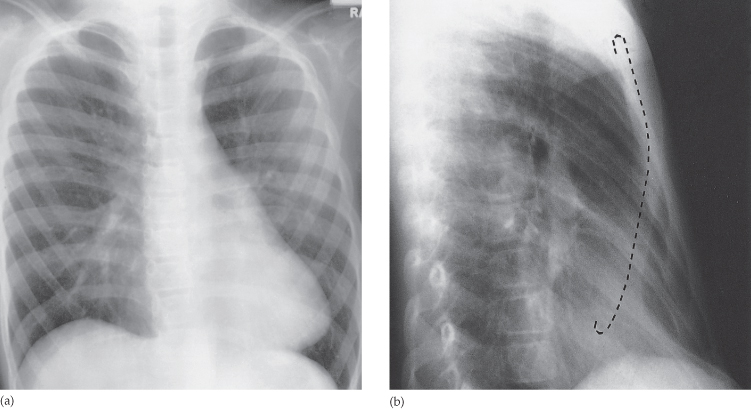
The standard plain films for the evaluation of cardiac disease are the PA view and a lateral chest film (Fig. 3.1). The cardiothoracic ratio (CTR) is a widely used, but crude, method of measuring heart size. The transverse diameter of the heart is normally less than half the internal diameter of the chest when measured on erect PA films (Fig. 3.2). Anteroposterior views magnify the heart, and films taken in supine or semi-erect positions lead to cardiac enlargement. Knowing whether or not the heart has increased in size compared with previous films is often more useful than the CTR in isolation. It should, however, be realized that the transverse cardiac diameter varies with the phase of respiration and, to some extent, with the cardiac cycle. Thus, changes in transverse diameter of less than 1.5 cm should be interpreted with caution. An overall increase in heart size may be due to dilatation of one or more cardiac chambers and/or to pericardial effusion. A potential pitfall is a patient with a severely depressed sternum (pectus excavatum) in whom the cardiac outline may appear enlarged and altered in shape from simple rotation and displacement (Fig. 3.3).
Fig. 3.1 Outline of the heart in posteroanterior and lateral views. Ao, aorta; LA, left atrium; LAA, left atrial appendage; LV, left ventricle; PA, pulmonary artery; RA, right atrium; RPA, right pulmonary artery; RV, right ventricle.
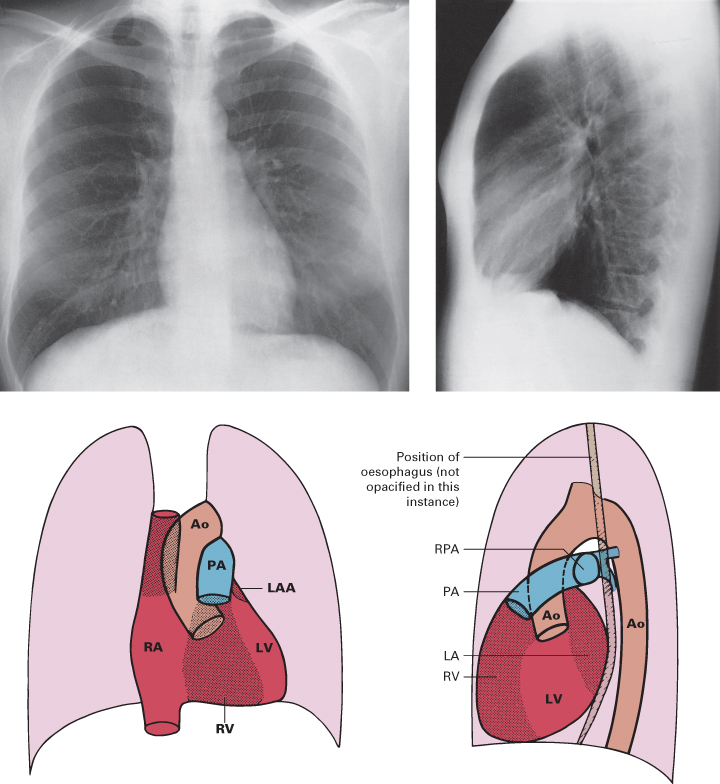
Fig. 3.2 Measurement of heart size. The transverse diameter of the heart is the distance between the two vertical tangents to the heart outline. When the cardiothoracic ratio (CTR) is calculated, the transverse diameter of the heart (B) is divided by the maximum internal diameter of the chest (A).
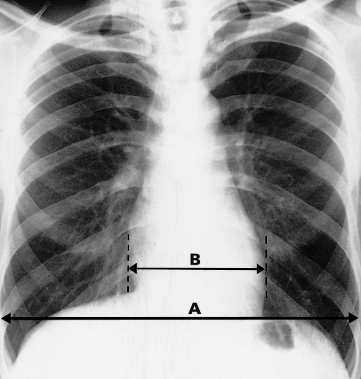
Fig. 3.3 Pectus excavatum. (a) Posteroanterior view. Note how the heart is displaced and altered in shape by the depressed sternum. (b) Lateral film. The edge of the sternum has been traced in on this film. There was no cardiac disease in this patient.
The only plain film information directly relating to morphology of the valves is calcification, which is best evaluated at echocardiography. Calcification of the mitral valve ring is occasionally seen on CXRs in the elderly, and is often associated with mild mitral regurgitation.
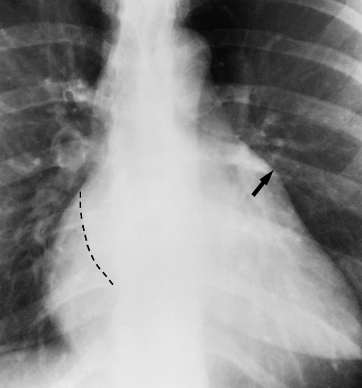
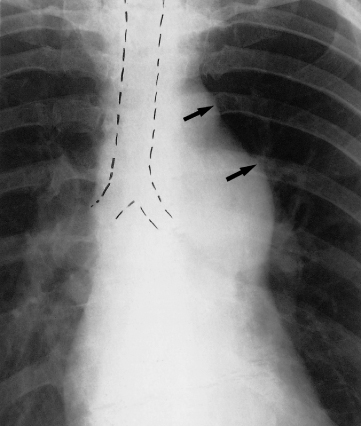
Diagnosing specific chamber enlargement on plain films, with the possible exception of dilatation of the left atrium, is fraught with problems. It is rarely possible to distinguish ventricular hypertrophy from dilatation by looking at the external contours of the heart. Ventricular dilatation is recognized only as an overall increase in transverse cardiac diameter. Assessment of atrial size on the CXR, particularly left atrial enlargement (Fig. 3.4), is easier: the right border of an enlarged left atrium is visible as a double contour adjacent to the right heart border, usually within the main cardiac shadow. The left atrial appendage, when dilated, is seen as a bulge below the main pulmonary artery on the PA view. Right atrial enlargement causes an increase in the curvature of the right heart border and is often accompanied by enlargement of the superior vena cava.
Fig. 3.4 Left atrial enlargement in a patient with mitral valve disease showing the ‘double contour sign’ (the left atrial border has been drawn in) and dilatation of the left atrial appendage (arrow).
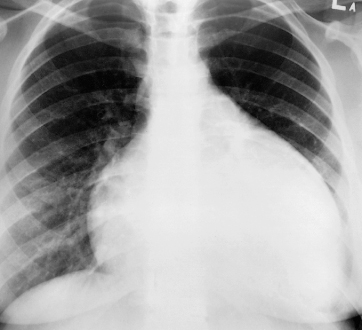
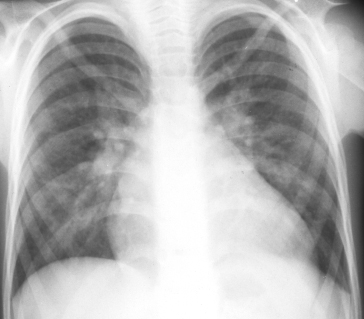
It is unusual to be able to diagnose a pericardial effusion from the plain CXR. Indeed, a patient may have sufficient pericardial fluid to cause life-threatening tamponade, but only have mild cardiac enlargement with an otherwise normal contour. A marked increase in the transverse cardiac diameter within a week or two, particularly if no pulmonary oedema occurs, is virtually diagnostic of the condition. Pericardial effusion should also be considered when the heart is greatly enlarged and there are no features to suggest specific chamber enlargement (Fig. 3.5). Extensive pericardial calcification is seen in patients with constrictive pericarditis.
Fig. 3.5 Pericardial effusion. The heart is greatly enlarged. (Three weeks before, the heart had been normal in shape and size.) The outline is well defined and the shape globular. The lungs are normal. The cause in this case was a viral pericarditis. This appearance of the heart, though highly suggestive of pericardial effusion is not specific to it – a similar appearance can be seen with other causes of cardiac enlargement, e.g. cardiomyopathy.
Main Pulmonary Artery and Pulmonary Vasculature
The CXR provides a simple method of assessing the size of the main pulmonary artery and the pulmonary vasculature. Even though it is not possible to measure the true diameter of the main pulmonary artery on plain film, there are degrees of bulging that permit one to say that it is indeed enlarged (Fig. 3.6). The assessment of the hilar vessels can be more objective since the diameter of the right lower lobe artery can be measured: the diameter at its midpoint is normally between 9 and 16 mm. The size of the vessels within the lungs reflects pulmonary blood flow. There are no generally accepted measurements of normality, so the diagnosis is based on experience with normal films. By observing the size of these various vessels it may be possible to diagnose one of the following haemodynamic patterns.
Fig. 3.6 Enlarged main pulmonary artery in a patient with pulmonary valve stenosis. The bulge of the main pulmonary artery (lower arrow) is clearly greater than normal and at first glance one might be deceived into diagnosing enlargement of the aorta. However, the aortic knuckle is the first ‘bump’ on the left mediastinal border (upper arrow). It projects 2.5–3 cm lateral to the trachea. The pulmonary artery forms the segment immediately below the aortic knuckle.
Increased Pulmonary Blood Flow Due to Left to Right Shunts
Atrial septal defect, ventricular septal defect (Fig. 3.7) and patent ductus arteriosus are the common anomalies in which there is shunting of blood from the systemic to the pulmonary circuits (so-called left to right shunts), thereby increasing pulmonary blood flow. In patients with a haemodynamically significant left to right shunt (2 : 1 or more), all the vessels from the main pulmonary artery to the periphery of the lungs are large. This radiographic appearance is sometimes called pulmonary plethora.
Fig. 3.7 Ventricular septal defect in a child. The heart is enlarged and there is obvious enlargement of the pulmonary vessels. The left to right shunt in this case was 3 : 1.
Pulmonary Arterial Hypertension
The conditions that cause significant pulmonary arterial hypertension (Box 3.2) all increase the resistance of blood flow through the lungs.
- Various lung diseases (e.g. cor pulmonale)
- Pulmonary emboli
- Mitral valve disease
- Left to right shunts
- Idiopathic pulmonary hypertension
Pulmonary arterial hypertension (Fig. 3.8) has to be severe before it can be diagnosed on plain films. The CXR features are enlargement of the pulmonary artery and hilar arteries, the vessels within the lung being normal or small. The reason for pulmonary arterial hypertension may be visible on CXR, such as radiologically visible lung disease in cor pulmonale.
Fig. 3.8 Right ventricular enlargement in an adult with primary pulmonary hypertension. The heart is enlarged with the apex of the heart somewhat lifted off the diaphragm. Note also the features of pulmonary arterial hypertension – enlargement of the main pulmonary artery and hilar arteries with normal vessels within the lungs.
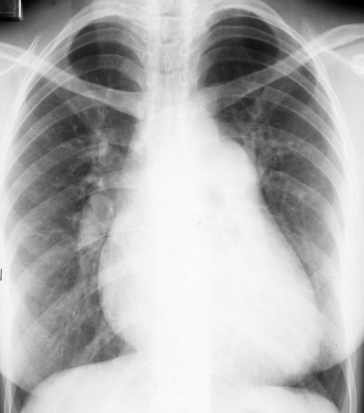
Pulmonary Venous Hypertension
Mitral valve disease (Fig. 3.9) and left ventricular failure are the common causes of elevated pulmonary venous pressure. In the normal upright person, the lower zone vessels are larger than those in the upper zones. In raised pulmonary venous pressure, the upper zone vessels enlarge and in severe cases become larger than those in the lower zones. Eventually, pulmonary oedema will supervene and may obscure the blood vessels.
Fig. 3.9 Pulmonary venous hypertension in a patient with mitral valve disease. The upper zone vessels (straight arrows) are larger than the equivalent vessels in the lower zones (curved arrows). This is the reverse of the normal situation. (The left atrial border has been drawn in.)

Pulmonary Oedema
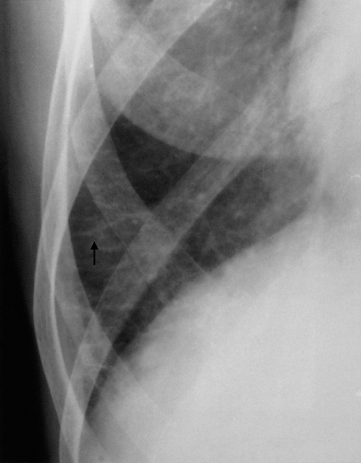
There are two radiographic patterns of cardiogenic pulmonary oedema: alveolar and interstitial. As oedema initially collects in the interstitial tissues of the lungs, all patients with alveolar oedema also have interstitial oedema.
Interstitial oedema (Fig. 3.10). There are many septa in the lungs which are invisible on the normal CXR because they consist of little more than a sheet of connective tissue containing very small blood and lymph vessels. When thickened by oedema, the peripherally located septa may be seen as lines, known as Kerley B lines, named after the radiologist who first described them. They are horizontal lines, never more than 2 cm long, seen laterally in the lower zones. They reach the lung edge and are, therefore, readily distinguished from blood vessels, which never extend into the outer centimetre of the lung. Another sign of interstitial oedema is that the outline of the blood vessels may become indistinct owing to oedema collecting around them. Fissures may appear thickened because oedema may collect against them.
Fig. 3.10 Septal lines known as Kerley B lines in a patient with mitral stenosis. Note that these oedematous septa are horizontal, non-branching lines that reach the pleura. One such line in the right costophrenic angle is arrowed.
Alveolar oedema (Fig. 3.11) is a more severe form of oedema in which the fluid collects in the alveoli. It is almost always bilateral, involving all the lobes. The pulmonary opacification is usually maximal close to the hila and fades out peripherally, leaving a relatively clear zone peripherally that may contain septal lines. This pattern of oedema is sometimes referred to as the ‘butterfly’ or ‘bat’s wing’ pattern.