Cardiovascular Anatomy
Robert W. W. Biederman
Innumerable textbooks have been solely devoted to dissertations on cardiac anatomy over the centuries. Most of these have focused on practical, autopsy-based anatomy with few depicting image-based, non-autopsy or pragmatic clinical anatomy. The natural question that one may ask is, “What is the difference? Why does it matter?” The answer is that the difference becomes clinically relevant when the anatomic features that are visible on images approach or exceed those observable to the naked eye at autopsy or in the surgical suite. Is it possible that the evaluation of closed-chest cardiovascular anatomic features could actually be seen with better clarity and precision than when the postmortem body is explored or view directly on the operating table? Investigations by us and others suggest that the answer to that question is, “Yes”. Specifically, many features of the heart are visible in the beating, contracting state that are paradoxically masked when the heart stops. When the heart finally stops beating, upon natural death or arrested for surgical purposes, rather then stopping at an arbitrary point in the cardiac cycle, the heart ceases beating when calcium cycling terminates, resulting in massive calcium overload and frank tetanus, and obligatorily ending the cardiac cycle in systole. Therefore, the heart stops in the contractile state, in fact in a massive state of hypercontraction with resultant emptying of most of the ventricular volume such that, when combined with the extreme vasodilatory state, due to absent venous return, the heart is at a markedly unnaturally small and shrunken state. This results in rigorous retraction of the otherwise subtle but important anatomic features, such as the valvular/papillary muscle relationship, trabeculae carnae, as well as deflation of the venous and arterial system, with subsequent distortion of the relative relationships of the normal cardiac structures to each other.
The cardinal notion here then is that cardiovascular magnetic resonance (CMR), with its high spatial resolution and modest temporal resolution, permits imaging in the normal, unadulterated state, permitting a more realistic and “natural state” assessment, often portraying features of the left ventricle (LV) not recognized by the pathologist or the surgeon. In this chapter, details of the cardiac and related cardiovascular anatomy will be delineated; their relations in the normal state will be illustrated and presented in standard CMR imaging planes.
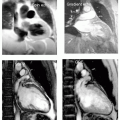
In general, imaging in our hands starts with a series of multislice transverse axial acquisitions, obtained in either the double inversion recovery sequence or a steady state free precession (SSFP) sequence. In the following figures, CMR images will be demonstrated in the SSFP sequence, with the moving anatomy viewable in the accompanying digital video disc (DVD). The motion during the natural cardiac cycle often helps to define the interrelationships based on an anatomicophysiologic basis. Figures 7-1 to 7-5 display the multislice axial transverse acquisitions from the great vessels through to the diaphragm; Figs. 7-6, 7-7 show coronal anatomy; Figs. 7-8, 7-9 show parasagittal views; Figs. 7-10, 7-11 show short axis views. Figures 7-12, 7-13, and 7-14 are two-chamber, three-chamber, and four-chamber views, respectively, with Fig. 7-15 showing the paraxial aortic valve (AV) view. Here, descriptions and discussions of integral anatomic segments of the heart and vascular and there interrelations are presented, generally without specific reference to any particular view. Table 7-1 gives an explanation of abbreviations used in text and figures.
CARDIAC ANATOMY
The heart is considered to have three segments: the atria, ventricles, and the great vessels. The atria and ventricles are each partitioned into two compartments, the left and right sides, with two atrioventricular valves that connect the respective ventricle to the atria and the semilunar valves that connect the great vessels to the ventricles.
The heart is a central mediastinal organ that lies generally in the left chest and aligned with the long axis
traveling from the posterior right shoulder to the left nipple, as related to the sagittal plane of the body. This is the standard position, defined as normal or levocardia. Infrequently, the heart is in the opposite chest, with a mirror image denoted as dextrocardia. An even rarer finding is that of mesoposition, where the heart occupies the midline position.
traveling from the posterior right shoulder to the left nipple, as related to the sagittal plane of the body. This is the standard position, defined as normal or levocardia. Infrequently, the heart is in the opposite chest, with a mirror image denoted as dextrocardia. An even rarer finding is that of mesoposition, where the heart occupies the midline position.
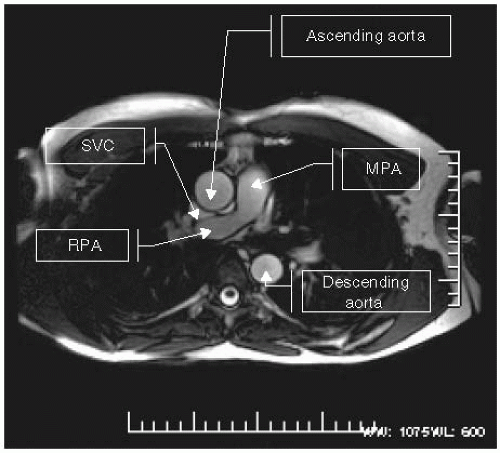 FIGURE 7-1 Transverse image (see Table 7-1 for abbreviations). |
SIDEDEDNESS
In healthy individuals, the cardiovascular, gastrointestinal, and respiratory organs are asymmetric such that sidedness occurs. The cardiovascular side is defined by the position of the morphologic right atrium. This is determined specifically by the size and shape of the right atrial appendage. Importantly, it is not decided by position of the LV, ventricular apices, relationship of the great arteries, or more importantly, by the particular side that the gastrointestinal or respiratory system occupies. Similarly, definitions of sidedness for the pulmonary and gastrointestinal system can be defined by the relationship of the lungs to the liver/inferior vena cava system. Sidedness has many variants: situs solitus is normal as described in the preceding text,
whereas situs inversus is the mirror image of the entire mediastinal respiratory and gastrointestinal system. Situs isomeric defines a more symmetric pattern with situs indeterminate and situs ambiguous defining less clear relationships of the three systems to each other. Finally, right isomerism is when there is bilateral right-sided symmetry and left isomerism is when there is bilateral left-sided symmetry. In the former, there is a bilateral morphologic right atria (two) while the spleen is absent, known as asplenia syndrome.
whereas situs inversus is the mirror image of the entire mediastinal respiratory and gastrointestinal system. Situs isomeric defines a more symmetric pattern with situs indeterminate and situs ambiguous defining less clear relationships of the three systems to each other. Finally, right isomerism is when there is bilateral right-sided symmetry and left isomerism is when there is bilateral left-sided symmetry. In the former, there is a bilateral morphologic right atria (two) while the spleen is absent, known as asplenia syndrome.
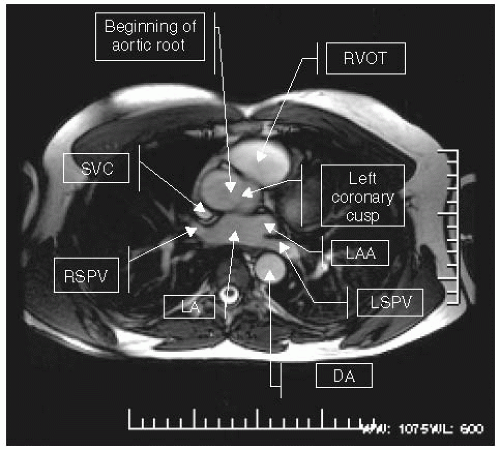 FIGURE 7-2 Transverse image (see Table 7-1 for abbreviations). |
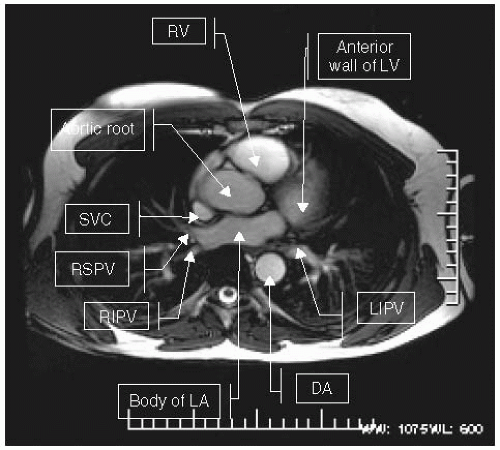 FIGURE 7-3 Transverse image (see Table 7-1 for abbreviations). |
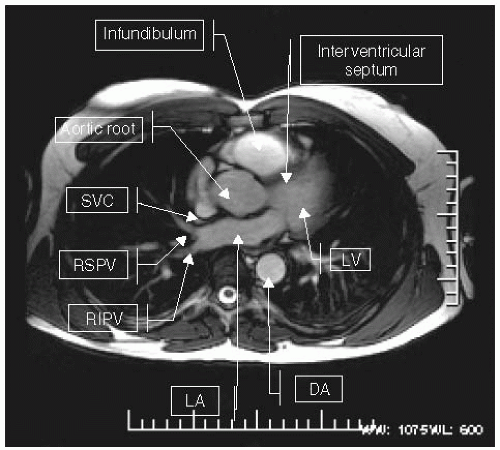 FIGURE 7-4 Transverse image (see Table 7-1 for abbreviations). |
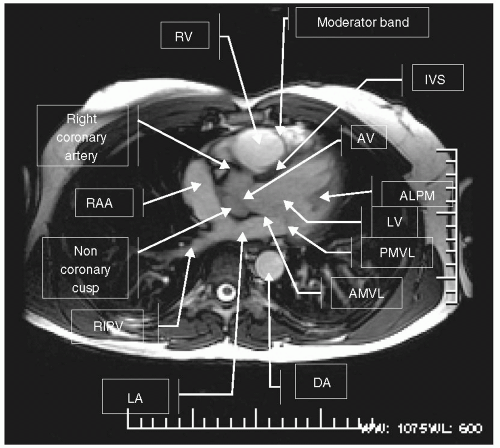 FIGURE 7-5 Transverse image (see Table 7-1 for abbreviations). |
ATRIA
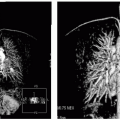
An understanding of the morphologic features of the right and left atria in healthy individuals is critical. While seemingly mundane, a well-founded anatomic understanding in healthy individuals is essential to allow insight into pathologic states, especially in congenital heart disease. The right atrium has small-to-absent pectinate muscles and, as a large tricorn appendage, receives the superior and inferior vena cava, as well as the coronary sinus. An important feature, helping to define the right atrium, is a subtle projection from the inside of the right atrium called the crista terminalis. The projection of this feature as viewed from the pericardial side is the sulcus terminalis. The morphologic left atrium is smaller than the right, has slightly thicker walls, and has a windsocklike appendage with larger pectinate muscles. There is no crista terminalis and the body of the left atrium receives the four pulmonary veins. The left atrium has a septum primum, whereas the right atrium has the septum secundum, which forms the interatrial septum. Not seen by current imaging techniques, are the foramina venarium minima, which are small venous openings returning venous flow directly from the cardiac muscle. The right atrium is superior and rightward to the heart. The entrance to the right atrium can be traced from three pathways: superior vena cava (SVC) (superior), inferior vena cava (inferior), and the coronary sinus (located inferior and posterior and below the floor of the left atrium). A fourth entrance is through the tricuspid valve. Entrance into the left atria, however, is through the four pulmonary veins, which are normally located as two right (upper and lower) and two left (upper and lower). The position and number of pulmonary veins can vary considerably from four, and the appearance on images is quite variable. In patients referred for pulmonary vein isolation, we and others have described as many as seven veins and as few as two. Frequently, the pulmonary veins do not lie in a superior-inferior direction, but enter the body of the atrium in one plane, making it difficult for an electrophysiologist to locate the anatomic variants. A considerable amount of variability is sometimes not recognized, and therefore not reported. Especially, when more than four pulmonary veins are identified, one can imagine the difficulty encountered when the electrophysiologist isolates the first four pulmonary veins and,
unknown to him, there are several more. CMR has a unique ability to define these anatomic variants and relate them in space using SSFP or three-dimensional magnetic resonance angiography (MRA) reconstruction techniques.
unknown to him, there are several more. CMR has a unique ability to define these anatomic variants and relate them in space using SSFP or three-dimensional magnetic resonance angiography (MRA) reconstruction techniques.
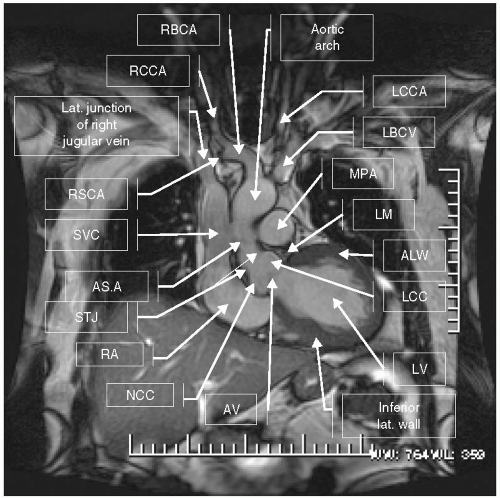 FIGURE 7-6 Coronal image (see Table 7-1 for abbreviations). |
VENTRICLES
Right Ventricle
The right ventricle (RV) receives the deoxygenated blood of the superior and inferior vena cava, as well as deoxygenated coronary blood flow from the coronary sinus and the small Thebesian veins, which drain from the right ventricular myocardium directly into the right ventricular chamber. Anterior to the RV is the pericardium and sternum, whereas inferiorly is the diaphragm, to the left and posteriorly is the ventricular septum. The RV is essentially crescent shaped and consists of three parts: the inflow, outflow, and body. The outflow portion known as the infundibulum is a tubular-shaped channel that leads to the pulmonary valve. A thick muscular ridge called the supraventricular crest separates the pulmonary and tricuspid orifices. Trabeculae carnae are rounded and irregular projections that arise from the body of the RV and are embryologically remnants from the mesocardium, whose purpose is somewhat ambiguous. Some authors believe that they may be helpful in redirecting flow in an efficient manner from the inflow to the RV body and into the outflow infundibulum. Others believe, including us, that they aid in a more efficient contractile and ejection patterns to exclude blood. The pattern of myocardial fiber orientation is less mechanically effectively organized in the RV compared to the LV. The ultimate trabeculae carnae are the papillary muscles, which are attached to chordae tendonae, which parachute out towards the tricuspid valve. The RV, as compared to the LV, is recognized by its morphology, with a moderator band, which houses the right bundle branch electrical conduction system for the right ventricular free wall. In many hearts a septal-parietal band is present, which houses the origination of the papillary muscles, as opposed to arising off the floor of the right ventricular apex. The RV




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree