Cardiac Triggering
Mark Doyle
MOTIVATION
It has been said “In CMR, triggering is everything.” Although there is always the promise that one day real-time imaging will invalidate that statement, that era is yet to dawn. Given this situation, the following three important prerequisites for cardiac magnetic resonance (CMR) remain:
Triggering
Triggering
Triggering
In short, there is no cardiac image without triggering.
ESTABLISH A CLEAN ELECTROCARDIOGRAM SIGNAL
First, to establish a strong electrocardiogram (ECG) signal, good contact between the skin and the ECG electrodes is required (see Fig. 18-1). To accomplish this, certain precautions and procedures should be followed:
If body hair intrudes, it should be shaved off.
The skin should be abraded to allow effective electrical contact.
A gel should be used.
Electrodes of the highest quality should consistently be used.
The patient should be mandated to wear loose clothing to prevent buildup of sweat, which destroys electrical contact as the study progresses. This is a particularly troubling problem, because to remedy it the patient must be withdrawn, the leads repositioned, and scout scans repeated.
The airflow in the scanner should be adjusted to keep the patient at a comfortable temperature.
TIPS AND TRICKS: ELECTROCARDIOGRAM
To ensure good scan quality, it is advisable to spend time up front to obtain a good ECG signal. If signal is weak or otherwise poor, consider the following hierarchy of solutions:
Change the reference lead at the scanner console.
Reposition the leads.
If not contraindicated by the scanner manufacturer, consider positioning the leads on the patient’s back (over the heart region).
If the patient has a known myocardial infarction (MI), the triggering signal may be weaker than for a normally functioning heart. Be cognizant that the lead positions may not be the exact configuration required for a patient without an MI. If the location of MI is known, consider positioning the leads toward the side of the heart with the most function. If, after these precautions, the signal is still too weak, only spend a minimal of time changing the signal leads because the solution likely requires repositioning of the leads on the patient. It is therefore advisable to put a few extra pads on in anticipation of this, to allow easier repositioning.
POSITION ELECTRODES FOR SAFETY
Formally, electrodes could be positioned at widely separated sites on the chest. This effectively formed a wide conductance loop, but the high performance gradients and radiofrequency (RF) of modern scanners can induce currents sufficient to burn the patient. Currently, a tight configuration of electrodes is generally required for safety (see Fig. 18-1).
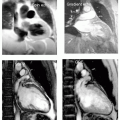
 FIGURE 18-1 Patient preparation is shown, whereby hair is shaved and skin abraded in preparation for placement of electrocardiogram (ECG) pads (left panel). The configuration of the ECG pads is shown in the right panel. Note the relatively tight configuration centered on the heart. |
ESTABLISH SIGNAL
After observing normal screening precautions, position the patient on the scanner table, typically feet first. Connect the ECG leads, respiratory gating device, and blood pressure cuff for full monitoring capability. Before positioning any receiver coils, check the adequacy of the signal at the console.
MANY WORDS ONE PHENOMENON
In the same manner that Eskimos are reputed to have more than 20 words to describe snow, magnetic resonance imaging (MRI) personnel have a wide vocabulary to describe the condition of the ECG signal:
Normal (a highly nuanced term)
Weak
Distorted
Respiratory breakthrough
Inverted
“We can live with it”
Normal Electrocardiogram Signals
Even the “normal” ECG signal has a grossly distorted “T” wave (see Fig. 18-2). The “T” wave corresponds to a period in the cardiac cycle when blood is rapidly ejected from the heart to the vascular system. Blood, which is a conducting fluid moving in a magnetic field, will generate an electrical signal of its own. This electrical signal adds to the natural “T” wave, essentially broadening and elevating it.
Weak Electrocardiogram Signals
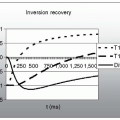
A weak ECG signal often suffers from “respiratory motion breakthrough” (see Fig. 18-3). In this situation, the whole ECG drifts up and down with the respiratory cycle, usually resulting in a very erratic triggering capability. To remedy this, consider repositioning leads or reattaching the leads at the same position. Changing the signal lead at the scanner console rarely remedies this problem, and only a minimum amount of time should be spent trying this approach.
Distorted Electrocardiogram Signals
Distortions take many forms, and surprisingly it is often possible to trigger with grossly distorted waveforms (see Fig. 18-4). The key features to look for in an ECG signal is that the “r” wave is higher and sharper than any other wave feature. If the scanner software detects the trigger point based on signal amplitude, a higher signal is required for successful and consistent triggering. However, in some scanners, the trigger point is sensitive to the maximum rate of change of the signal,




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree