Thoracic Magnetic Resonance Angiography
Robert W. W. Biederman
The study of thoracic angiography is chiefly concerned with evaluation of the aorta and its branch vessels. Cardiovascular magnetic resonance (CMR) has rapidly become a valuable modality for evaluation of both adult and pediatric aortic disease. The reason for this rapid acceptance of CMR is multifactorial: chiefly, the ability of CMR to image in a noninvasive manner, coupled with its intrinsic ability to image in any three-dimensional (3D) plane, makes it an ideal imaging tool, and the resolution that CMR provides for evaluation of the sometimes complex, perturbations that occur, adds another level of utility to this technique.
CMR has been shown to be the reference standard for the evaluation of aortic aneurysms (see Figs. 10-1 and 10-2), as well as having the highest sensitivity and specificity for the detection of aortic dissections (see Figs. 10-3, 10-4, and 10-5). When compared to transesophageal echocardiography (TEE) and x-ray angiography, CMR for the detection of aortic aneurysms, has been shown in multiple studies to have a sensitivity and specificity >98%. Particularly for aortic aneurysms, the ability to serially follow with high dimensional reproducibility allows optimal timing of surgical intervention. This issue has even greater relevance when nonaxial imaging is used. Reliance on axial imaging, frequently over- or underestimates dimensions compared to measurements made in nonorthogonal views. For instance, in the elderly population, as the descending aorta approaches the diaphragmatic hiatus, the lumen no longer travels perpendicular to the transversal plane, and the obliquity of the vessel results in overestimation of the lumen size. These features of CMR have an immediate clinical translation, avoiding inadvertent referral for surgery or worse still, actual surgical intervention. For this reason, CMR has been demonstrated to be the most appropriate modality, adding important surgical information, such as the presence of mural thrombus and other intraluminal perturbations, with near 100% accuracy.
More recently, the ability to add magnetic resonance angiography (MRA) to traditional magnetic resonance imaging (MRI) has further improved the capability of evaluating the aorta. Although older MRA data sets were acquired slice by slice, acquisitions were long and laborious, often taking 30 minutes of acquisition, and requiring extensive post-processing time. These acquisitions have been largely replaced with gadolinium contrast studies (see Figs. 10-6 and 10-7). The gadolinium agent is inert with almost no demonstrable side effects in patients with normal kidney function, and the increased T1 effect granted to the blood pool improves, not only the time of acquisition, but improves contrast, allowing increased fidelity of reconstruction. Three-dimensional reconstruction is now performed in an automated or semiautomated manner, and results in exquisite high-resolution surface and volume renderings. These images provide excellent roadmaps for planning surgical interventions (see Fig. 10-8).
The basis of CMR imaging for the thoracic vessels typically relies on double inversion recovery (DIR) and steady state free precession (SSFP) sequences, allowing diagnosis of aortic anatomy. Generally, non-breath-hold oblique images provide the necessary fidelity and resolution to allow assessment of intraluminal dimensions and morphologic features with high reproducibility. Flow-related enhancement (FRE) is a particularly important feature that must be accounted for in the determination of both luminal wall thickness and intraluminal pathology. Obtaining breath-hold images, reducing slice thickness, or changing the phase direction can improve image quality when considering flow-related artifacts. The SSFP sequence allows improved image contrast, to distinguishing between thrombus (dark) and normal blood (bright). On DIR images, slow-moving blood will not have had sufficient time to exit the imaging plane, and therefore may also be seen in these images (see Fig. 10-3). Direction of flow in antegrade or retrograde patterns is helpful in ascertaining the likelihood
for dissection propagation, as well as for detecting thrombus deposition. The pattern of blood flow within dissected lumens and aneurysms is well characterized by CMR using the SSFP sequence. The SSFP sequence represents a major improvement over the gradient-recalled echo (GRE) sequence for the determination of intraluminal pathology, because contrast is related to the intrinsic T2/T1 ratio of the tissue, and is not dominated by blood flow characteristics.
for dissection propagation, as well as for detecting thrombus deposition. The pattern of blood flow within dissected lumens and aneurysms is well characterized by CMR using the SSFP sequence. The SSFP sequence represents a major improvement over the gradient-recalled echo (GRE) sequence for the determination of intraluminal pathology, because contrast is related to the intrinsic T2/T1 ratio of the tissue, and is not dominated by blood flow characteristics.
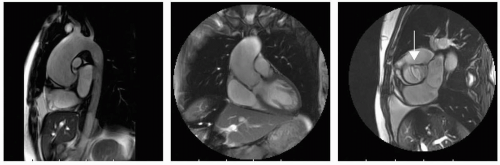
 FIGURE 10-1 Proximal ascending aortic aneurysm originating at the sinotubular junction sparing the sinus of Valsalva but distorting the aortic valve architecture with resultant mild (1+) aortic regurgitation. Note the prior sternal wires (left panel) from coronary artery bypass graft (CABG) surgery 10 years before distorting the anterior aorta, but minimally affecting the double inversion recovery (DIR) images (right panel) not precluding accurate measurements. The etiology of the aneurysm is not likely due to postoperative (iatrogenic) mechanism due to the symmetric nature and its involvement equilaterally around the sinotubular junction. |
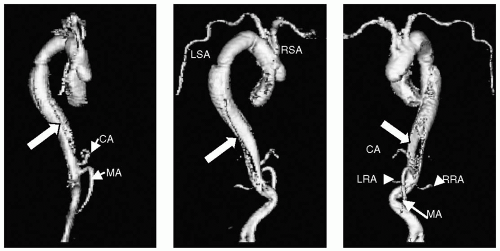
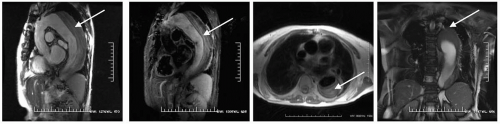 FIGURE 10-3 Selected steady state free precession (SSFP) images (left panels) demonstrate a type B aortic dissection and what appears to be a large thrombosed false lumen. The right to left panels are selected double inversion recovery sequences, demonstrating the multiple layers of accumulated thrombus. Images relate to case study 2. |
The use of MRA techniques involving a paramagnetic agent infused as a bolus (to reduce the blood T1) has resulted in high signal contrast of blood vessels, and
in some cases coronary arteries or bypass grafts (see Fig. 10-9). In situations where either the DIR or SSFP sequences are not optimal, coordinated timing of contrast administration (using one of several approaches) permits rapid and reproducible vascular imaging. The fidelity of image acquisition allows vessels of submillimeter dimensions to be visualized. For instance, in a compliant patient, the intercostals vessels are often well seen in routine thoracic MRA. This has particular advantage for patients who have dissections, to allow an understanding of the need for an operation and for considering maintaining patency of the adjacent small vessels. Because acquisitions can be obtained in one to four table moves, the single bolus injection can be tracked as it passes through the aorta. Timed correctly, one can visualize the ascending aorta, arch, descending
aorta, abdominal aorta, iliac vessels, and finally the femoral and infrageniculate arteries.
in some cases coronary arteries or bypass grafts (see Fig. 10-9). In situations where either the DIR or SSFP sequences are not optimal, coordinated timing of contrast administration (using one of several approaches) permits rapid and reproducible vascular imaging. The fidelity of image acquisition allows vessels of submillimeter dimensions to be visualized. For instance, in a compliant patient, the intercostals vessels are often well seen in routine thoracic MRA. This has particular advantage for patients who have dissections, to allow an understanding of the need for an operation and for considering maintaining patency of the adjacent small vessels. Because acquisitions can be obtained in one to four table moves, the single bolus injection can be tracked as it passes through the aorta. Timed correctly, one can visualize the ascending aorta, arch, descending
aorta, abdominal aorta, iliac vessels, and finally the femoral and infrageniculate arteries.
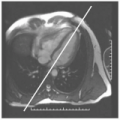
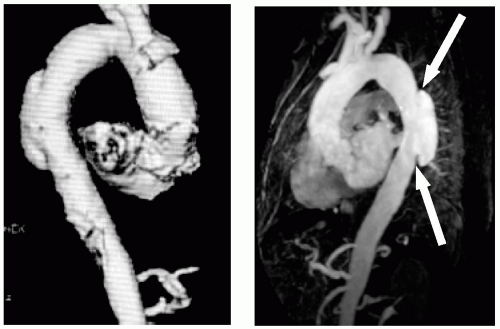 FIGURE 10-5 The two magnetic resonance angiographies(MRAs) demonstrate the focal Type Aortic III mushroom-shaped dissection of the mid thoracic descending aorta; however, the steady state free precession (SSFP) demonstrates the physiology of the dissection and suggests the etiology: a penetrating ulcer, arrowed. Images relate to case study 3. |
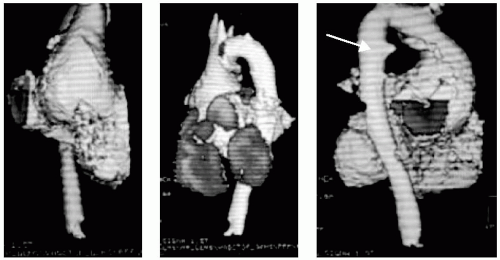
 FIGURE 10-6 Magnetic resonance angiography (MRA) depicts a focal, atypical aneurysm of the proximal ascending aorta. Note the bovine aorta (arrow). Images relate to case study 4. |
 FIGURE 10-8 Cardiovascular magnetic resonance (CMR) was performed to evaluate for cardiac source of emboli, revealed multiple areas of atherosclerotic, as well as mobile plaque (left panel). The multiple location and sporadic nature of the plaques and mobile atheroma precluded surgical options, relegating her to coumadinization, for which a repeat magnetic resonance angiography (MRA) eight weeks later revealed resolution (right panel). Images relate to case study 6. |
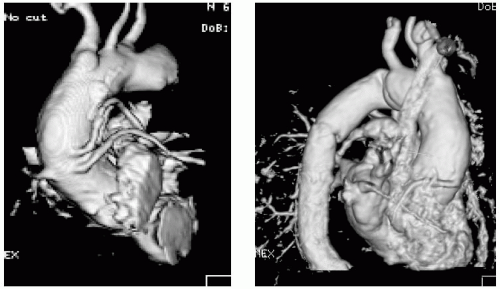 FIGURE 10-9 Cardiovascular magnetic resonance (CMR) of aorta, demonstrating no abnormality. Note also, the patency of three grafts. The saphenous vein graft (SVG) to left anterior descending (LAD) and SVG to obtuse marginal 1 (OM1) were both patent (left panel) as was the saphenous vein graft of the right coronary artery (SVG-RCA) (right panel). Images relate to case study 7. |
STRATEGIES FOR DETECTION OF AORTIC DISSECTIONS BY CARDIOVASCULAR MAGNETIC RESONANCE
It bears mentioning that the CMR magnet is generally not in close proximity to the emergency room or intensive care units. As a precaution, unstable patients have not been routinely imaged by CMR; however, careful screening of patients permits reasonably safe, accurate and relatively fast, high-quality images to be obtained in certain circumstances. For the intubated and paralyzed patient, paradoxically, CMR performs better, because it is much easier to manage breath-holding by manual control, permitting high-quality imaging in the patient who may otherwise have been uncomfortable. In our facility, we conduct a discussion with the patient when possible, to explain the details of the study to be performed, the breath-hold instructions to be followed, and the plan for contrast administration. All of this helps to reassure and relax the patient. Nonetheless, evaluation of the patient by the imaging clinician is important in cases of a patient in extremis. By evaluating each patient prescan, when believed to be in an emergent situation, we have been successful in imaging many patients who might not have been considered candidates for CMR, turning down only the rare patient who is severely hypotensive, coding, or actively infarcting. This adds a small element of a time penalty, but the benefit to the patient to have the optimal examination performed is far more beneficial than the added morbidity and mortality of other more invasive and, potentially less accurate, techniques.
Once in the scanner, a rapid series of non-breath-hold double axial inversion recovery (IR) images are first obtained, which quickly provide a large amount of information, allowing a preliminary working diagnoses to be formed. If breath-hold images are required, they are then conducted. A series of parasagittal and coronal SSFP images of the aorta serves as the major imaging strategy, providing a large amount of important clinical information relating to structure, flow direction and characteristics, lumen patency, and localization of pathology. Oftentimes, in the setting of aortic dissection, the ability to detect and characterize intrinsic intimal flap fenestrations helps to dictate the need for subsequent interventional protection of mesenteric, renal, and runoff vessels. Specifically, if a Type aortic III dissection is present (see Tables 10-1 and 10-2 for classifications), surgical correction of the
ascending and arch aorta may be performed followed by balloon correction of aortic intimal flap fenestrations if they are not detected. In our laboratory, the evaluation of aortic pathology is not complete until the associated valvular and ventricular anatomy and physiology are defined. This entails evaluation of the aortic valve, sinus of Valsalva, and sinotubular junction, to detect the presence of aortic regurgitation. If present, the mechanism of valvular dysfunction is described, aiding in considerations for composite graft implantation. The extent, direction, and magnitude of the aortic regurgitation can be semiquantitatively assessed, and can be quantified by phase velocity mapping. SSFP images of the ventricle can be obtained to assess the impact of aortic regurgitation, left and right ventricular function, the presence of left ventricular hypertrophy, regional wall motion abnormalities, and left ventricle (LV) size. The presence of a pericardial effusion is an ominous sign, and should alert the interpreter that the dissection plane has extended through the pericardium. Generally, this means that there is occult dissection extending into the proximal ascending aorta. Given the large field of view (FOV) that CMR provides, the presence of a pleural effusion, especially a left pleural effusion, suggests that there has been extravasation of blood beyond the aortic wall and this is a major adverse cardiovascular prognostic sign.
ascending and arch aorta may be performed followed by balloon correction of aortic intimal flap fenestrations if they are not detected. In our laboratory, the evaluation of aortic pathology is not complete until the associated valvular and ventricular anatomy and physiology are defined. This entails evaluation of the aortic valve, sinus of Valsalva, and sinotubular junction, to detect the presence of aortic regurgitation. If present, the mechanism of valvular dysfunction is described, aiding in considerations for composite graft implantation. The extent, direction, and magnitude of the aortic regurgitation can be semiquantitatively assessed, and can be quantified by phase velocity mapping. SSFP images of the ventricle can be obtained to assess the impact of aortic regurgitation, left and right ventricular function, the presence of left ventricular hypertrophy, regional wall motion abnormalities, and left ventricle (LV) size. The presence of a pericardial effusion is an ominous sign, and should alert the interpreter that the dissection plane has extended through the pericardium. Generally, this means that there is occult dissection extending into the proximal ascending aorta. Given the large field of view (FOV) that CMR provides, the presence of a pleural effusion, especially a left pleural effusion, suggests that there has been extravasation of blood beyond the aortic wall and this is a major adverse cardiovascular prognostic sign.
CASE STUDIES
Case Study 1.
A 45-year-old male presents with mild chest discomfort and is discovered to have a systolic ejection murmur. In Fig. 10-2, the left panel demonstrates a moderately dilated proximal descending aortic aneurysm extending up to the distal descending aorta tapering at the arch. The middle panel of Fig. 10-2 further demonstrates mild sinotubular effacement and an asymmetric aortic valve. The explanation for all is revealed in the third panel on the right panel of Fig. 10-2, which depicts a bicuspid aortic valve (arrow), which is strongly associated with ascending aortic dilatation.
Case Study 2.
Presenting with severe back pain radiating to the abdomen and very different from his earlier myocardial infarction chest pain for which he underwent prior coronary artery bypass graft (CABG) years ago, this 72-year-old hypertensive man is emergently referred for CMR. Selected SSFP images (see Fig. 10-3, left panels) demonstrate a type B aortic dissection with what appears to be a largely thrombosed false lumen. Note the origination site in extremely close proximity to the left subclavian artery (LSA). Selected DIR




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree