Chapter 34 Care of patients during radiotherapy
However, everyone involved in this provision is well aware that patients have a right to expect that they will be well cared for and supported during this time. The quality of this care is dependent on a multiplicity of factors and the aim should be that it is all encompassing; addressing both the physical and emotional needs of patients and this should be our aspiration whether the treatment intent is to cure or to palliate. The most simplistic method of exploring supportive care in radiotherapy is to consider any aspect of care that may be experienced by the patient within the physical, psychosocial and spiritual realm and this chapter will introduce some of the key themes within supportive care of all radiotherapy patients. The physical aspects of supportive care in relation to the management of site-specific conditions are addressed in related chapters throughout this text. In addition, these and the other aspects of care can be explored further in specialist texts which deal with issues relating to palliative care, symptom control and psychosocial interventions [1, 2].
Assessment of individual patient and carer needs
• control and management of physical effects of treatment and disease and associated side effects
• evidence-based quality assured patient information materials, including written, DVD, and utilizing digital and web based technologies
• good communication and involvement in decision making
• psychological, social and spiritual support
Skin reactions
One such side effect is the reaction of skin to radiotherapy. Although there have been recent advances in the technical delivery of radiotherapy which have resulted in the use of higher energy beams, customised treatment shapes and escalated dose, skin toxicity still remains a challenge. Indeed the situation may also be further enhanced with the increasing trend of combined adjuvent therapies. All patients receiving external beam therapy are at some risk of skin damage [3] and as such, in most departments this is addressed by offering suitable advice and support by monitoring and recording the severity of these reactions during treatment.
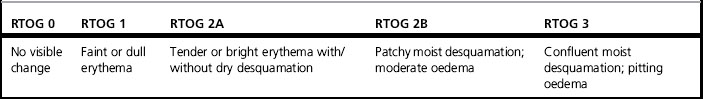
Skin reactions range from mild erythema to moist desquamation and occur more frequently in the head and neck area, breast and chest wall and areas with skin folds. The most widely used assessment tool is the Radiation Therapy Oncology Group grading (Table 34.1).
The severity of skin reactions has been attributed to a number of extrinsic (treatment related) and intrinsic (how people react to radiotherapy) factors [4] and these may well have a genetic basis. However, the goal of good management is to have a system in place which facilitates the identification of risk and delays the onset of skin reactions. This can be facilitated by having a patient review process that includes the assessment grading and recording of skin reactions.
Patients should be provided with information explaining:
• how and why skin reactions occur
• when they are likely to appear
• what they will look and feel like
• where the reaction is likely to occur
Involving patients in the prevention/care of skin reactions is an important element of the management process and reducing irritants to irradiated skin is a part of this self-care strategy. Skin can be exposed to a number of irritants which, if avoided, can lessen the likelihood of a troublesome reaction (Table 34.2) [5, 6].
Table 34.2 Recommendations for reducing irritants to irradiated skin during a course of radiotherapy
| Sun exposure | Protect from direct sun exposure: cover with clothing or shade area. Stress that risk from sun exposure is lifelong and following radiotherapy a sun block should always be used if exposure unavoidable |
| Mechanical irritants | Minimize friction: wash or shower gently; avoid using a washcloth; pat dry with a soft, clean towel; wear loose fitting, soft clothing Avoid shaving or shave causing as little trauma to skin as possible- suggest electric shaver Avoid scratching Avoid rubbing vigorously and massaging Avoid use of adhesive tape in treatment field |
| Chemical irritants | Use mild soap (un-perfumed) and rinse thoroughly Apply only recommended products- check with treatment centre. Any topical cream or lotion to be used at room temperature Avoid perfume, aftershave, deodorant Use mild detergent to wash clothing |
| Thermal irritants | Use tepid water Avoid exposure to temperature extremes Avoid application of ice packs or heat (e.g. heating pad, hot water bottles, sun lamp) |
How to care for radiation skin reactions once they have occurred and what products to recommend in this event requires a knowledge of the more general wound care literature. It is important that advice and treatment given to patients is evidence based and that advice such as ‘no washing’ is now seen as inappropriate. Sadly this remains an area which lacks robust evidence from the literature, which in turn, creates challenges when making recommendations, Table 34.3 provides some small detail of skin-care products which can be utilized.
Table 34.3 Characteristics of skin-care products for each stage of radiation skin reactions
| No change in skin (RTOG0) | No intervention required. Aqueous cream if desired ( n.b. this will not prevent or delay skin reaction |
| Faint or dull erythema (RTOG 1) | Aqueous cream applied to skin within the treatment field – may soothe and moisturise skin |
| Tender or bright erythema (RTOG 2a) | Aqueous cream – may soothe and moisturise skin, relieve itching Hydrocortisone cream – can be used sparingly for up to one week, skin to be reviewed and documented daily |
| Patchy moist desquamation (RTOG 2b) | Dressings should be non adhesive Hydrogel and non adhesive dressings, soft polymer dressings, hydrocolloid dressings |
| Moist desquamation (Pitting oedema) (RTOG 3) | Dressings should be non adhesive Hydrogel dressings, hydrocolloid dressings, anti microbial dressings, polyurethane foam dressings |
Other sources which may be useful include published national skin-care guidelines [7]. When moist desquamation becomes infected or infection is suspected, use of a silver or iodine based antimicrobial dressing may be used. Care should be taken to ensure the dressing is designed to prevent silver being absorbed by the wound (check manufacturer’s information) and the dressing should be removed daily before treatment.