Daniel Do • Claudio J. Schönholz
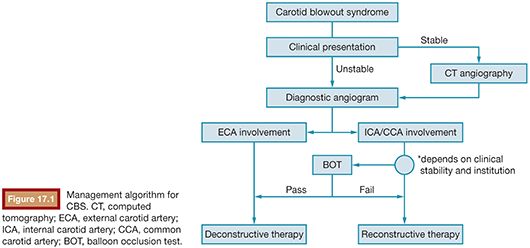
Carotid blowout syndrome (CBS), first described in 1962, is a severe clinical condition that usually presents in the setting of patients with underlying head and neck cancer, specifically those with prior radiation treatments.1–4 Its reported incidence is 3% to 4% in patients with neck dissection, with a 7.6-fold increased risk in the setting of additional radiation therapy.5,6 CBS involves compromise of the carotid artery and/or its branches and can present as transoral or transcervical hemorrhage. When associated with open surgical treatment, high mortality (40%) and neurologic morbidity (60%) have been reported.2,3 As such, multiple endovascular options have been developed and are divided into either deconstructive or reconstructive techniques. Deconstructive techniques have been described involving permanent occlusion of carotid vasculature through use of coils, liquid embolic agents, detachable balloons, and Amplatzer Vascular Plugs (St. Jude Medical, Inc., St. Paul, Minnesota).2–5,7,8 Deconstructive techniques are typically used when the external carotid artery (ECA) is involved as neurologic sequelae would be unusual and unexpected (Fig. 17.1). In the setting of common carotid artery (CCA) or internal carotid artery (ICA) involvement, a balloon occlusion test (BOT) is typically performed for clinical assessment of adequate contralateral cerebral circulation. If the patient tolerates BOT without transitional neurologic deficit, then permanent vessel occlusion may be pursued. On the other hand, reconstructive techniques maintain vascular patency through use of covered stent. Depending on the institution, this may or may not represent first-line treatment in the setting of CBS. Generally, it is the preferred treatment option in those patients who either fail BOT, are unable to clinically undergo BOT, or demonstrate incomplete collateral circulation through the circle of Willis. CBS has been described to represent a clinical spectrum and categorized into multiple groups: threatened (group 1), sentinel hemorrhage/impending rupture (group 2), acute rupture (group 3), and recurrent CBS.3,4 Group 1 involves patients with exposed carotid arterial segments either identified by physical examination or imaging whose natural course is likely rupture. Group 2 involves patients who have experienced a hemorrhagic event, which was either self-resolved or limited with simple surgical packing. Group 3 involves patients with active, large-volume hemorrhage that cannot be controlled with surgical packing alone. Recurrent CBS refers to the subset of patients who have undergone initial treatment and subsequently rebleed.
CLINICAL APPLICATIONS
Timing of intervention is primarily dictated by clinical presentation. By definition, threatened CBS patients are likely stable, whereas acute rupture would be actively exsanguinating, necessitating immediate intervention. In unstable patients, adequate resuscitation efforts with dedicated anesthesia monitoring and appropriate inotrope usage are necessary before intervention. If the patient is clinically stable, preprocedural cross-sectional imaging is recommended. Neck computed tomographic angiography (CTA), including the aortic arch, may be able to identify the causative lesion and assist in prediction of vessel size and tortuosity, preprocedural supplies, expedite methods of action and execution, and management. Pertinent CTA findings in CBS involve necrosis, artery exposure, viable tumor, pseudoaneurysm, and contrast extravasation.9 If the clinical presentation precludes a CTA, the patient should be taken directly for a diagnostic arteriogram. If the CCA or ICA is found to contain the offending lesion, reconstructive therapy is preferred in cases where the patient fails BOT and if BOT or contralateral collateral examination cannot be performed secondary to patient sedation, intubation, or fragile clinical status. Additionally, reconstructive management may be the primary treatment modality in all technically feasible cases dependent on institution given the ability to achieve hemostasis and preserve vascular patency. In cases of contralateral carotid occlusion, carotid reconstruction may be the only endovascular option. Deconstructive management is the preferred treatment option in cases involving the ECA as neurologic sequelae from permanent vessel occlusion is minimal. Regarding ICA and CCA lesions, if the patient has an uneventful BOT or angiographically demonstrates adequate contralateral collateral circulation through an intact circle of Willis, embolization may be performed. The selection of primary treatment modality is institution dependent. Deconstructive therapy may be a preferred option in the treatment of patients with preexisting carotid occlusion or when vessel tortuosity precludes adequate stent placement.
TECHNIQUE
When performing the diagnostic angiography, it is important to remember that most patients in either group 2 or 3 will likely have complex intubations or tracheostomies.8 Performing the study under local anesthetic and moderate sedation is ideal, particularly in the setting of BOT. Typical standard femoral artery access and angiographic techniques are used. If the angiogram is the initial imaging modality, diagnostic interrogation of the entire carotid circulation is performed, which includes an aortic arch and selective bilateral common carotid and vertebral arteriograms. Identification of endoluminal irregularity, pseudoaneurysm formation, disruption, or frank extravasation within the CCA, ICA, or ECA should warrant definitive treatment. Evaluation of an intact circle of Willis and posterior collateral circulation via the vertebral arteries is mandatory if permanent CCA or ICA occlusion is considered. Additional interrogation of the subclavian artery, thyrocervical trunk, and costocervical branches should be considered in cases of lower neck hemorrhage.8 Selection of the supra-aortic arch vessels can be performed with standard reverse curve (Simmons types 1 to 3) or angled tip catheters (Vertebral, Headhunter).
Deconstructive endovascular techniques involve the use of permanent arterial occlusion through coils, liquid embolic agents, and Amplatzer Vascular Plugs. Detachable balloons were previously used but are no longer available in North America. Embolization of the ECA is typically achieved through use of coils and/or liquid embolic agents. If used in conjunction, primary placement of coils followed by liquid embolic introduction is preferred for formation of a matrix.8 Coverage distal and proximal to the hemorrhagic lesion is crucial in achieving hemostasis, eliminating the possibility of continued filling via collateralization. Particles can be used to achieve small vessel occlusion in distal ECA branches. Embolization of the ECA and the selection of the embolic agent should be done knowing that there are multiple collateral circulation pathways between branches of the ECA and ICA that could be the source of nontarget embolization leading to stroke complications.
If embolization of the CCA or ICA is considered, a BOT is performed to demonstrate patient’s tolerance without increased neurologic sequelae. BOT is only used in a stable, cooperative patient. Following a baseline neurologic examination, a microcatheter with distal nondetachable Hyperform balloon (Covidien, Irvine, California) is placed proximally within the culprit vessel. After adequate systemic heparinization, the balloon is carefully insufflated with occlusion confirmed with hand contrast injection through the catheter. Continuous neurologic monitoring is then performed for a 15- to 20-minute period. If there is no change from the patient’s neurologic baseline, occlusion of the ICA or CCA can be considered. If new neurologic symptoms are experienced, the balloon should immediately be deflated to prevent permanent ischemic injury. If the BOT cannot be performed due to patient instability or intubation and reconstructive techniques are unachievable, the examination of the contralateral collateral circulation can be performed during balloon insufflation for evaluation. The ICA occlusion can be achieved through use of coils and self-expandable occlusion devices. Optimally, embolization would begin intracranially, specifically at the level of the petrous or cavernous ICA segment. This reduces potential thromboembolic phenomenon often associated with proximal embolization caused by residual large-volume blood stagnation. Sparing of the ophthalmic segment is beneficial, allowing for reversed collateral supply into the remainder of the intracranial ICA.8
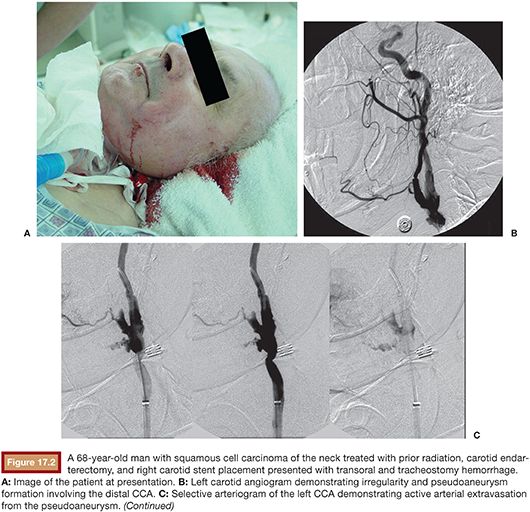
Endovascular reconstruction of the carotid artery employs use of covered stent placed across the offending lesion, achieving both hemostasis and preservation of blood flow (Fig. 17.2). However, as covered stents are known to serve as a thrombogenic nidus, an antiplatelet regimen with acetylsalicylic acid or clopidogrel should be incorporated.10,11 Varying treatment patterns have been reported but commonly involve preprocedural antiplatelet administration and intraprocedural systemic heparinization, with the goal of having the activated clotting time two to three times the baseline. Again, antiplatelet regimen ad infinitum should follow the stent graft placement.8,10,12–18 Additional use of intravenous glycoprotein IIb/IIIa inhibitors in conjunction with heparin has also been described, especially in cases where preprocedural antiplatelet treatment is not feasible.13 If the anticipated stent placement crosses the carotid bifurcation, embolization of the ECA is recommended to prevent rebleeding through collateral filling. Due to the natural anatomic configuration of the carotid bulb, type I endoleaks may be encountered, producing a potential source for persistent or recurrent hemorrhage. Maldonado et al.19 and Chen et al.20 described the use of N-butyl cyanoacrylate (NBCA) to assist in sealing the endoleak. This is achieved through use of an additional access with placement of a microcatheter across the lesion before stent deployment. Following stent deployment, the microcatheter is positioned with NBCA administered in appropriate placement. Immediate microcatheter withdrawal is followed upon completion of injection. Embolization with liquid embolic agents like cyanoacrylate and Onyx (Covidien, Irvine, California) should be reserved for interventionists with extensive experience using these embolic agents. Additionally, broader stent graft coverage of the lesion has been suggested given natural disease progression in possible prevention of rebleeding complications.21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree