- Most cervical spine injuries are relatively minor, but they can be potentially devastating, requiring prompt diagnosis and stabilisation
- Cervical spine radiographs are difficult to interpret and 20% of fractures may not be visible. Therefore, there should be a low threshold to proceed to CT
- CT is now the imaging modality of choice in major trauma
- MRI is indicated if there is suspicion of neurological, ligamentous or disc injury
Injuries to the cervical spine can occur either in isolation or in association with head injury or multisystem injury following major trauma. Most of these injuries are relatively minor, but they can be potentially devastating, requiring prompt diagnosis and stabilisation to minimise the risk and severity of associated neurological injury. The pattern, frequency and distribution of these injuries vary between different populations. In adults, the C1–2 and C5–6 levels are most typically affected. In children, injuries are less common and usually involve the upper cervical spine.
Up to 40% of cervical spine injuries are associated with neurological injury, with 5–10% reported as the result of missed injury and consequent lack of cervical stabilisation. About 0.1% of cervical spinal cord injuries do not present with a radiographic abnormality. These spinal cord injuries without radiographic abnormality (SCIWORA) most typically affect children and young adults but also occur in older patients, often with associated cervical spine degenerative disease.
Anatomy
The cervical spine (Figure 10.1) is comprised of seven bony segments, separated by intervertebral fibrocartilaginous discs and supporting ligaments. The third to seventh vertebrae are morphologically similar, each with a vertebral body and a posterior neural arch that is comprised of bilateral pedicles, facets and laminae with a single posterior spinous process. They form a protective bony spinal canal, around the spinal cord. Small transverse processes transmit the vertebral arteries via the foramina transversaria, usually from C2 to C6.
Figure 10.1 Anatomy of cervical spine with line drawing.
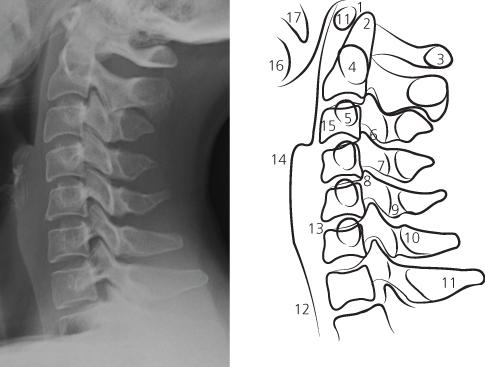
The ring-like C1 vertebra (atlas) has anterior and posterior arches but no vertebral body, articulating with C2 and the base of the skull via bilateral lateral masses and the anterior atlantodental joint. There is no C1–C2 intervertebral disc. The C2 vertebra (axis) is distinguished from the adjacent levels by a superior bony projection, the odontoid process or dens, which articulates with C1.
Stability of the cervical spine depends mainly on the integrity of soft tissue structures, in particular the spinal ligaments. The major longitudinal ligaments are the anterior and posterior longitudinal ligaments and the ligamentum flavum. The supraspinous and interspinous ligaments connect the spinous processes. Tough capsules support the facet joints. The apical ligament, alar ligaments and the tectorial membrane (continuation of the posterior longitudinal ligament) give support to the craniocervical junction, and the transverse ligament spans the interval between C1 lateral masses posterior to the dens supporting the C1–C2 articulation.
Imaging of the cervical spine
Patients who are fully conscious with no history of alcohol consumption or drug intoxication, no head injury, no distracting injuries, no symptoms and no clinical signs do not require any imaging. A three-view plain film series (lateral, anteroposterior and open mouth odontoid radiographs) is often performed as the first line investigation for patients whose cervical spine cannot be cleared by clinical assessment alone. Unfortunately, plain radiographs are often suboptimal and even good quality radiographs can fail to demonstrate up to 20% of fractures, so there should be a low threshold to proceed to CT.
CT is a useful adjunct to plain films and is now the first line imaging modality for the spine in major trauma patients, where there is a high risk mechanism as part of whole body CT.
- High velocity motor vehicle collision (>35 m.p.h.)
- Closed head injury
- Fall >10 ft
- Fractures (pelvic, multiple limbs)
- Spinal neurological symptoms
- Death at scene (motor vehicle collision)
- Neck pain/tenderness
- Hyperflexion
- Hyperextension
- Rotation
- Axial compression
- Distraction
- Lateral bending/shearing
- Complex or combined vectors
MRI is also indicated where there is neurological injury or possible major ligamentous or intervertebral disc damage (Figure 10.2). Lateral flexion and extension radiographs are no longer recommended.
ABCs systematic assessment
- Adequacy
- Alignment
- Bone
- Cartilage and joints
- Soft tissues
- Lateral: base of skull to T1 superior endplate
- AP: C3 to T1 vertebrae and C2 spinous process
- Open mouth odontoid: C1 and C2 margins should be visible
Interpretation of lateral radiographs
Always review the lateral view as if the patient had turned to the right. This will orientate the lateral view in the same direction as the sagittal CT reconstructions and the sagittal MRI
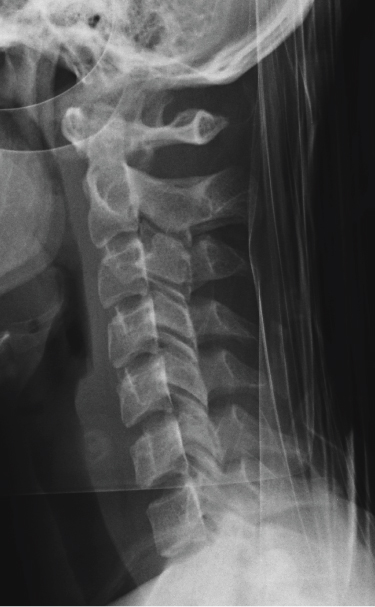
Adequacy (Figure 10.3)
The base of skull to the superior endplate of the T1 vertebral body should be demonstrated with clear cortical and trabecular detail. The outline of the pre-vertebral soft tissues and tip of the spinous processes should also be shown. The lower cervical spine should not be obscured by overlying anatomy (shoulders) or extrinsic structures such as jewellery or monitoring devices. If the C7–T1 junction cannot be seen, a swimmer’s view should be performed, progressing to CT if still inadequate.
Figure 10.2 Sagittal STIR MR image following a hyperflexion image demonstrating disruption of the C3/4 disc, ligamentous injury and cord contusion.

Alignment
The cervical spine normally forms a smooth lordotic curve, which may be flattened (Figure 10.4) or slightly reversed due to pain, muscle spasm, immobilisation or supine position. Pre-existing congenital anomalies or pathology such as degenerative change can also result in abnormal alignment. The anterior longitudinal line, posterior longitudinal line and spinolaminar line should all be traced looking for any abrupt alterations in alignment, which may infer ligamentous or disc injury and instability. The spinolaminar line may deviate slightly anteriorly between C1 and C3 on flexion and slightly posteriorly on extension.
The posterior margins of the facet joints should also form a smooth lordotic curve but this line can be difficult to assess due to rotation. The spinous processes form a tighter lordotic curve from C2 to C7 with no sudden widening of the interspinous distance although the curve may not be perfect due to anatomical variation.
Figure 10.3 Lateral radiograph demonstrating the normal anterior longitudinal line (light blue), posterior longitudinal line (blue) and the spinolaminar line (white).
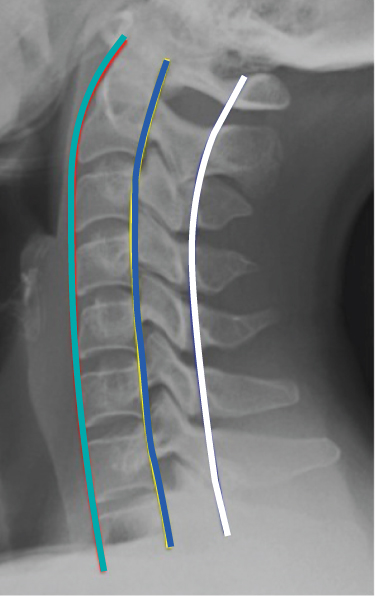
Figure 10.4 Lateral radiograph with patient immobilised on a spinal board demonstrating flattening of the normal lordosis.
Hyperflexion injuries (Figure 10.5) result in a focal anterior angulation, which may be accompanied by abrupt widening of the interlaminar and interspinous distances, indicating injury to the posterior ligament complex and subluxation or dislocation of the facet joints.
Figure 10.5 Hyperflexion injury with acute angulation at C3/4, facet joint subluxation and interspinous widening.
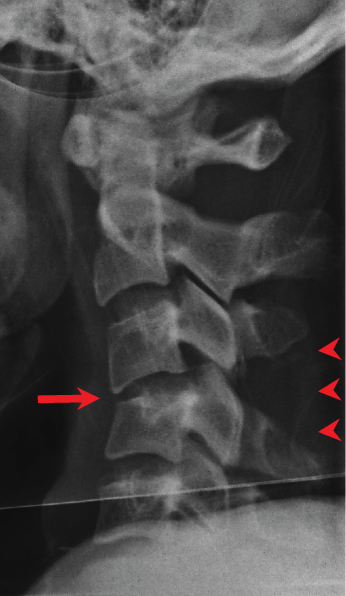
Figure 10.6 Bilateral facet joint dislocation with anterior subluxation of C6 on C7.
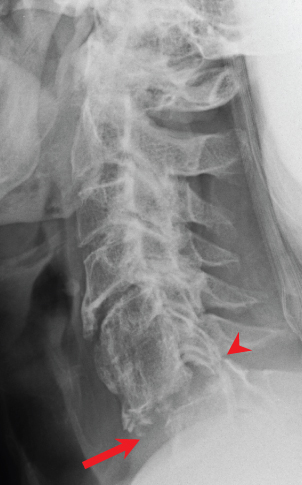
Figure 10.7 The Powers ratio (BC AO) for assessing craniocervical alignment: 0.6–1.0, normal; >1.0, anterior dislocation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree