Chapter 10 Cholangiocarcinoma
Epidemiology and Risk Factors
IHCC occurs most commonly in the sixth and seventh decades. There is male-to-female predominance of 3:2. The age-adjusted mortality increased from 0.15 to 0.66 per 100,000 persons from 1973 to 1997.1 The incidence of IHCC also increased from 0.13 to 0.67 per 100,000 from 1973 to 1997. The 5-year survival is less than 10%. The survival approaches 0% in the setting of intrahepatic metastasis. Surgery offers the best outcome.2
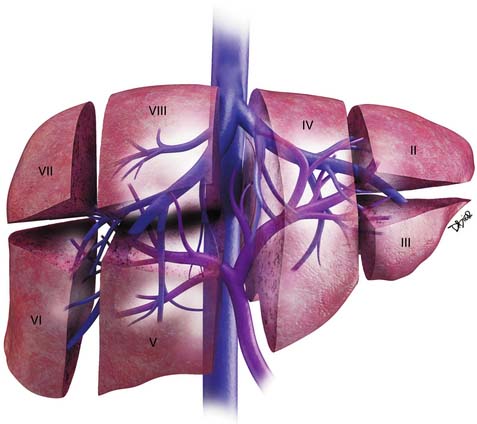
Anatomy
The liver is divided into the right and left lobes and subdivided into eight anatomic segments (Figure 10-1). The segments are defined by their portal vein supply and separated from each other by the hepatic veins. The caudate lobe is considered segment I. The portal supply to the caudate lobe arises commonly from the main portal vein but may be seen from the left or right portal veins. Segments II and III of the liver are in the left lobe and are supplied by the first and second lateral branches of the left portal vein, respectively. Segment IV is also in the left lobe of the liver and is separated from segments II and III by the left hepatic vein and the falciform ligament; it is supplied by the medial branches of the left portal vein. The right hepatic vein separates segments in the right lobe of the liver: segment VII from VIII and segment VI from V. Segments VII and VI are supplied by the posterior branch of the right portal vein, superior and inferior branches, respectively. Segments VIII and V are supplied by the anterior branch of the right portal vein, superior and inferior, respectively. The middle hepatic vein separates the right and left lobe of the liver (segment VIII from IV and segment V from IV). Segment V is also separated from segment IV by the GB fossa (see Figure 10-1).
The liver has a variety of vascular variants. Michel’s classification describes 10 hepatic arterial variants.3 The most common, type I, has a common hepatic artery that arises from the celiac artery and bifurcates into the right and left hepatic artery, supplying the right and left lobes of the liver. Other common vascular variants include a replaced or accessory right hepatic artery from the superior mesenteric artery and a replaced or accessory left hepatic artery from the left gastric artery. There are also hepatic venous variants, for example, an accessory hepatic vein draining segment VI to the lower retrohepatic vena cava. Surgical intervention and transarterial chemoembolization (TACE) rely on the complete understanding of the liver arterial anatomy. Documentation of the vascular supply of the liver is essential for correct treatment planning.
Pathology
The gross pathology evaluation of IHCC reveals a firm, gray-white tumor. The tumors are usually large and solitary. Satellite nodules are not infrequent.4 The tumors with periductal infiltration tend to have a higher incidence of satellite nodules and also of nodal metastases. Although more commonly seen in HCC, large portal vein and hepatic vein tumor invasion can be detected on gross specimen evaluation. IHCCs occur in noncirrhotic livers.
Clinical Presentation
Patients with IHCC present with nonspecific symptoms such as weight loss, abdominal pain, nausea, and malaise.5 In addition and in contrast to other cholangiocarcinomas that may not present with signs of biliary obstruction, IHCC typically presents with signs and symptoms associated with a large mass in the liver. The symptoms include pain, discomfort, weight loss, and anorexia. An enlarged liver may be detected on physical examination. Some cases present with an incidental liver mass, and imaging studies or endoscopic evaluation are performed in search for the site of possible primary GI tumor. In these cases, the diagnosis of IHCC is made as the diagnosis of exclusion. In contrast to HCC, the patients do not present with ascites, cirrhosis, or portal hypertension.
Laboratory testing shows normal bilirubin, elevated CA19-9 (median 140 U/mL with > 60% with CA19.9 > 100 U/mL).6 The median carcinoembryonic antigen (CEA) is elevated near 2.1 ng/mL and is not significantly different between intrahepatic and extrahepatic tumors.6
Staging Classification
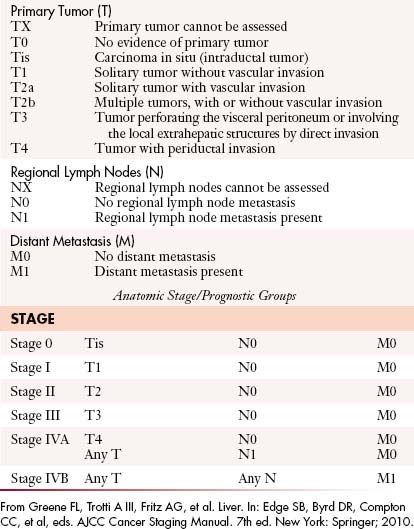
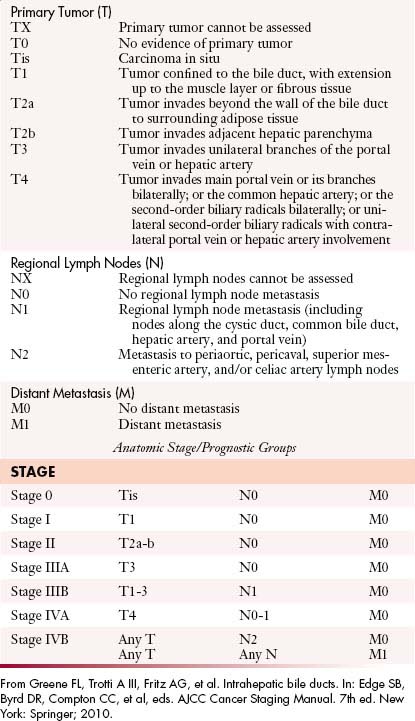
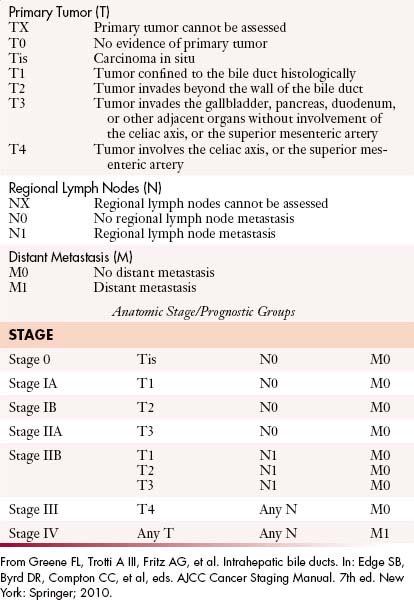
The most recent tumor-node-metastasis (TNM) staging criteria of the seventh edition of the American Joint Committee on Cancer (AJCC) is based on tumor number, size, and vascular invasion (T), local and distant metastatic adenopathy (N), and the presence of metastatic disease (M).6a The same staging is used for HCC (Table 10-1).
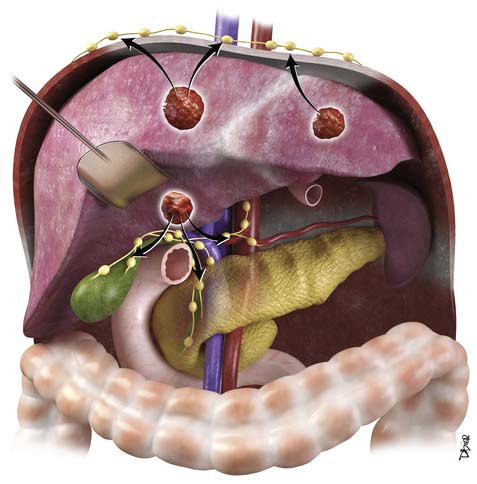
The nodal disease defines N1 and N2 nodes as regional or distant nodal spread of disease. In the central IHCC, the nodes along the hepatoduodenal ligament are considered N1 and nodes distant to this location are considered N2 (e.g., retroperitoneal nodes). Diaphragmatic nodes in the anterior, posterior, or middle diaphragmatic nodal stations may be considered as N1 nodes for IHCCs that are located near the dome of the liver (Figure 10-2). IHCC can present with distant metastases. Common sites of metastasis include the lungs, bone, adrenals, peritoneum, and brain. The lung metastases can be single or multiple nodules. The bone lesions are mostly lytic, and adrenal metastases are large, irregular masses. Thickening of omentum or discrete nodules are signs of peritoneal spread of tumor.
Patterns of Tumor Spread
IHCC may present with intrahepatic or extrahepatic tumor spread. The pattern of tumor spread is very similar to HCC.7 Similar to HCC, the most common type of tumor spread is intrahepatic via portal vein invasion. Biliary tract involvement is not common. The lymph nodes, skeleton, lung, and peritoneum are common sites of spread. Nodes along the hepatic hilum are a common site of tumor spread. The para-aortic, retropancreatic, and common hepatic nodes may also show tumor. For tumors in the left lobe of the liver, the left gastric, the paracardiac, and the nodes along the lesser curvature of the stomach may be involved (see Figure 10-2). Common distant lymph node involvement includes mediastinum and para-aortic nodes. For more peripheral tumors, the diaphragmatic nodes may be involved. Invasion through the liver capsule and extension to adjacent sites is more common in IHCC than in HCC. Extrahepatic spread has been reported as 50% to 67% based on autopsy series.8
Key Points Tumor spread of intrahepatic cholangiocarcinoma
Imaging
Primary Tumor
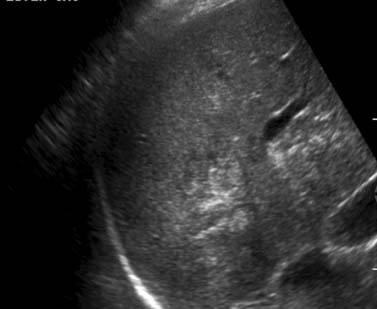
Similar to other GI malignancies, ultrasound (US) evaluation of the abdomen is commonly the first imaging modality to evaluate patients with IHCC. US provide a fast and relatively inexpensive evaluation. It is limited in that it is dependent on the experience of the operator and quality of the equipment. IHCC presents as a mass in the liver with variable echogenicity (Figure 10-3). Contrast-enhanced US will demonstrate relative hypoperfusion on the arterial phase of contrast administration and hypoenhancement on the portal venous phase.9 US may also be useful as guidance for fine-needle aspiration (FNA) biopsy and to evaluate vascular invasion with the aid of color Doppler techniques. US is very limited in the assessment of lymph node invasion and metastatic disease.
Computed tomography (CT) plays a major role in the clinical evaluation of patients with IHCC. The availability and short duration of the scan makes CT the major diagnostic tool in oncologic imaging, and IHCC is no exception. The CT imaging protocol of a patient with a liver mass is the multiphasic examination, same as HCC, obtained during the precontrast, late arterial, portal venous, and excretory phases of contrast administration. A bolus tracking technique is utilized to optimize the first phase of contrast administration. The images are obtained with at least a 16-slice multidetector row computed tomography (MDCT) scanner at 5 mm and reconstructed at 2.5 mm for each phase of contrast administration.
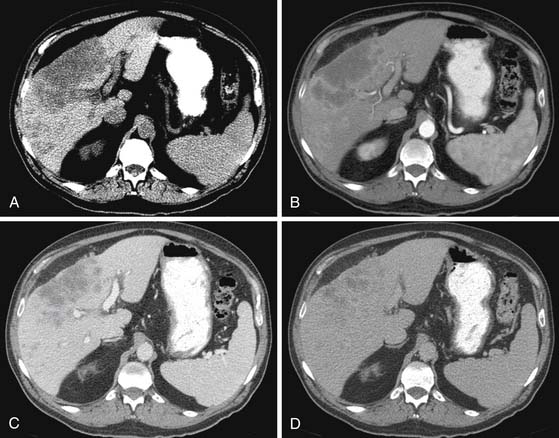
The IHCC will present as large, hypoattenuating masses in the precontrast images (Figure 10-4). During the late arterial phase of contrast administration, the enhancement, if present, is minimal and at the periphery (see Figure 10-4). On the portal venous phase, the enhancement will continue in a centripetal fashion and continue to progress on the delayed and excretory phases of contrast administration (see Figure 10-4). The CT findings of IHCC are very similar to those of hypovascular metastases, especially from the GI tract. Features that will suggest the diagnosis of IHCC include a large single mass, absence of a primary GI tumor, and absence of multiple nodules. Other CT findings seen on IHCC include calcifications and capsular retraction.
The multiphasic CT evaluation provides key information for surgical planning. This includes hepatic artery, portal vein, and hepatic vein anatomy. This is important in the setting of variant anatomy. Before surgery, calculations of future liver remnant (FLR) are made (FLR = future liver volume [FLV]/total expected liver volume [TELV]). In the setting of an FLR less than 20% (for a noncirrhotic liver) and less than 40% (for a cirrhotic liver), embolization of the portal vein is utilized with resultant compensatory hypertrophy and subsequent reduction in postoperative complications.10
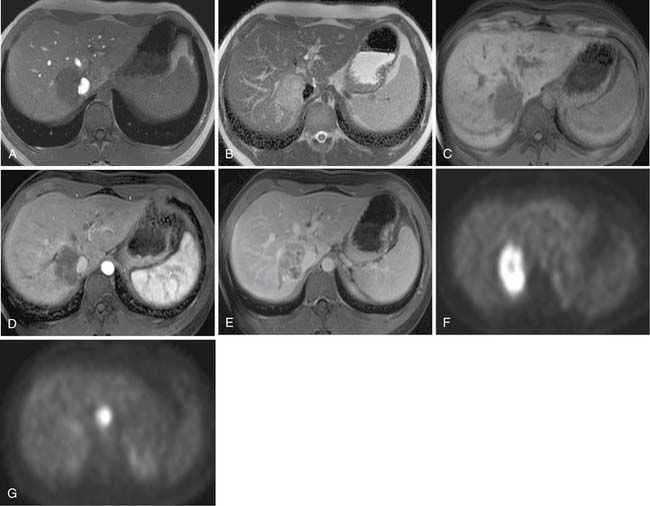
Two of the main reasons for the common use of CT for imaging patients with IHCC are its availability and short examination time. In contrast, magnetic resonance imaging (MRI) examinations are longer and may not be as readily available. However, MRI provides a higher contrast of lesion to liver on the various imaging sequences. The MRI protocol for the evaluation of patients with IHCC includes T1-weighted images (T1WI) and T2-weighted images (T2WI). The T1WI technique is a breathhold gradient echo sequence obtained at two echo times (2.1 [out-of-phase] and 4.2 [in-phase] msec), 1.5-T magnet. These two echoes can be obtained during a single repetition time (TR). The T2WIs consist of fast spin echo (FSE) and diffusion-weighted images (DWI). The FSE T2WI can be obtained with a respiratory-triggered technique or with breathhold technique. Our protocol utilizes a respiratory-triggered FSE sequence with time to excitation (TE) of 85 msec. On these noncontrast sequences, IHCC will demonstrate low signal relative to the liver on the T1WI, high signal on the T2WI, and restrictive diffusion on the DWI (Figure 10-5). On the T2WI, signal can be variable as a function of fibrosis (dark), mucous secretions (bright), or necrosis (bright).8,11 The darker central fibrosis may be a distinctive feature not commonly seen on metastatic disease to the liver.8 The DWI can be obtained at two different B values (0 and 500 sec/mm2). On this sequence, IHCC is usually hyperintense to liver at B of 0 and remains hyperintense to liver at B of 500 sec/mm2) (Figure 10-6). The larger B value allows the suppression of signal from vessels, bile ducts, and other fluids, resulting in an increased contrast between liver and lesion. The primary tumor as well as vascular invasion will have similar imaging features on the DWI. This is useful in the assessment of vascular invasion.
The postcontrast MRI evaluation consists of precontrast, late arterial, portal venous, delayed, and excretory phases of contrast administration. The timing of the injection is less critical than that for the evaluation of patients with HCC. The tumor will demonstrate peripheral enhancement with concentric fill-in (see Figure 10-5). Metastatic disease from colorectal cancer may show a pattern of enhancement similar to that seen on CT. The delayed complete enhancement may be seen only on the excretory phase or even later in the examination. In the setting of hepatocyte contrast administration, IHCC will not demonstrate uptake of contrast during the hepatocyte phase and will appear hypointense relative to the liver.3
Positron-emission tomography (PET) has become an important imaging modality in oncologic imaging. The most widely used radiopharmaceutical is fluoro-2-deoxy-D-glucose (FDG; see Figure 10-5). The benefits of PET/CT over CT include the increased accuracy in the detection of distant metastatic disease.12 Unfortunately, the sensitivity for detection of locoregional disease is less than 25%.13
Lymph Nodes
Lymph node metastases are a poor predictor of survival. In various series, the rate of positive lymph nodes found at surgery ranges from 31% to 59%.14–17 There is a reported negative effect on survival in the setting of lymph node metastases. In one series, the presence of three or more nodes had a 0% 3-year survival compared with 50% and 60% for one/two nodes and no nodes, respectively.16
Imaging features that may suggest tumor extension to the lymph nodes include size larger than 1 cm, low-density center, or delayed enhancement. CT has a high negative predictive value but a low positive predictive value for nodal involvement.18
Nodal stations that should be carefully examined in a patient with IHCC include the anterior, posterior, and middle diaphragmatic, celiac, hepatic artery, left gastric, and retroperitoneal nodal stations.19–21 Evaluation of retroperitoneal nodes is important in the search of N2 nodal stations. In our experience, DWI has shown to be very useful in the detection of lymph nodes (see Figure 10-6).
Metastatic Disease
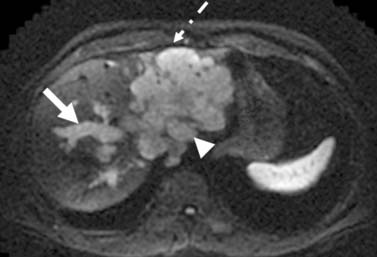
The pattern of tumor spread for IHCC may be extrahepatic or intrahepatic. Intrahepatic spread may include extension of tumor into the portal vein. The portal vein tumor will demonstrate postcontrast enhancement features similar to those of IHCC.22
Preoperative imaging should detect satellite nodules because these increase the risk of dying by approximately 4 to 11 times that found when satellite nodules are not present.15,23 Thus, satellite nodules may be considered a relative contraindication to surgery.
Treatment
Surgery
The routine intraoperative lymph node dissection is not recommended because it has limited effect on survival.17 For the evaluation of disease in the lymph nodes, optimum imaging and attention to detail in preoperative imaging interpretation are essential in correctly identifying surgical patients.
The primary tumor usually presents as a large mass that invades adjacent structures requiring extended hepatectomy. An extended hepatectomy is defined as the resection of four or more Couinaud segments. In large series, it was required in approximately 50% of cases.24,25 The extended resection may include vascular and biliary resection.26,27 There is a significant difference in survival between an R0 and an R1 resection. The R0 survival group had a median overall survival (OS) of 46 months. The R1 group had a 5-month median OS and the only explored group was 7 months.26 The 5-year OS for resected patients is 23% to 40%.15,23,26 The OS for an R0 resection is 36% to 63%.28,29 The resection rate for patients explored for curative intent is 50% to 87%.2,25,30 Prognostic factors for recurrence include a positive margin, satellite lesions, lymph node metastases, and vascular invasion.2,15,23,31
The use of liver transplant for treatment of IHCCA has been reported.
Key Points Surgery for intrahepatic cholangiocarcinoma
Transarterial Chemoembolization
Various publications describe the application of TACE to the management of patients with IHCC. In multiple series, the median survival was 21 to 24 months after TACE.32–34 Chemotherapy agents used include mitomycin C, doxorubicin, and cisplatin.35 The median survival in the nonsurgical population is 6 to 12 months.
Radiofrequency Ablation
The principle of radiofrequency ablation (RFA) is to apply a localized thermal treatment resulting in tumor death. The high temperatures of 100°C reached during RFA will result in coagulative necrosis of the tumor and surrounding liver. There are limited reports of RFA of IHCC 3.36,37 The effectiveness of the treatment is a function of tumor size (best at < 3 cm) with complete necrosis of the treated tumors in some cases.37 The radiologic description of the tumor should indicate the proximity to major vessels, diaphragm, or other structures that may interfere with the technical success of this procedure. Tumor response to RFA is best evaluated with extent of necrosis rather than size criteria used in the Response Evaluation Criteria In Solid Tumors (RECIST) criteria.
Chemotherapy
Single agents and combination therapies have been evaluated in patients with IHCC. Single-class agents include 5-fluorouracil (5-FU), mitomycin C, and gemcitabine. These have demonstrated low response rates. Combination therapy including cisplatin/gemcitabine, 5-FU/cisplatin, carboplatin/5-FU, and epirubicin/5-FU have also demonstrated low response rates.
Radiotherapy
Radiation therapy (RT) in biliary cancers is administered in the adjuvant setting after surgical resection or for the palliation of advanced disease.38 Local recurrence is the most common type of failure after surgical resection, and therefore, adjuvant radiation has a strong rationale. Unfortunately, level one evidence regarding adjuvant RT after surgical resection is lacking because there are no randomized, controlled trials. At our institution, patients have been selectively referred for adjuvant chemoradiation when they have positive lymph nodes or positive margins. Typical doses of radiation are roughly 50 Gy administered over 5 to 6 weeks with concurrent fluoropyrimidine chemotherapy.
Surveillance
After RFA, on imaging, the ablated tissue will show changes owing to hemorrhage and necrosis (liquefactive and coagulative).39,40 The hemorrhage will result in high signal on T1WI, the coagulative necrosis will result in low signal on T2WI, and the liquefactive necrosis will result in high signal on the T2WI. The liquefactive necrosis will demonstrate nonrestrictive diffusion on DWI (B = 500) and increase in apparent diffusion coefficient (ADC).41
It is important to note that the WHO and RECIST criteria are suboptimal in the evaluation of post–RFA-treated IHCC. The size of the cavity following RFA treatment will appear larger than the size of the original tumor. In these first scans, the evaluation should be centered on the margin of the RFA cavity. The detection of a nodular enhancement, irregular wall, or the distortion of a smooth tumor margin is a sign of an unsuccessful treatment.40 Subtraction images in MRI using the precontrast as the mask for subtracted images can be very helpful in detecting intracavity enhancement.
On follow-up studies, successful RFA will demonstrate a subsequent decrease in size of the cavity.39 An increase in size of the cavity (on CT or MRI) indicates either interval hemorrhage or recurrent disease.42,43
Epidemiology
The risk factors are the same as for other cholangiocarcinomas and include a family history of congenital fibrosis or cysts (Caroli’s disease, choledochal cyst, polycystic liver, or congenital hepatic fibrosis). Also included as risk factors are PSC, ulcerative colitis (UC), drugs (oral contraceptives, methyldopa, and isoniazid), chemical exposure (thorotrast, radionucleides, asbestos, arsenic, and dioxin), and primary biliary cirrhosis.44 For patients with UC, the risk of EHCC is 0.5%. The risk also increases with biliary cirrhosis, cholelithiasis, alcoholic liver disease, diabetes, and chronic pancreatitis.45 Infectious pathogens associated with EHCC include liver flukes (Clonorchis sinensis).
Clinical Presentation
Serum markers CEA and CA19-9 are commonly elevated in EHCC.46,47 In a series of 57 patients with EHCC, the laboratory values for bilirubin, CA19-9, and CEA levels are elevated. The median bilirubin was 9.4 mg/mL, CA19-9 was 140 U/mL, and CEA was 2.1 ng/mL.6 In patients with PSC and a value of CA19-9 greater than 100 U/mL, there is a sensitivity and specificity of 89% and 86% for EHCC, respectively.47 The CA19-9 is not specific because a portion of the population cannot synthesize the protein or may be elevated secondary to inflammation rather than tumor.48 The laboratory values of CA19-9 are elevated to a higher degree in the setting of IHCC.6
Anatomy
The combination of hepatic artery, bile duct, and portal vein is considered the porta triad. These anatomic structures course together to the various segments of the liver along the portal vein supply. The intimate relationship between these structures can lead to an unfortunately poor prognosis even in the setting of early disease because a small bile duct tumor can extend to either the portal vein or the hepatic artery and make the patient potentially inoperable. To provide the best outcome and analysis of radiologic imaging, familiarity with the variant arterial supply to the liver is of great importance. Michel’s classification of the hepatic artery describes variants of arterial supply to the liver.3 The most common variants include a replaced/accessory right hepatic artery from the superior mesenteric artery and a replaced/accessory left hepatic artery from the left gastric artery.
Pathology
The EHCCs are mostly well-differentiated, mucin-producing adenocarcinomas.4 Histopathology will demonstrate an increased nucleocytoplasm ratio, nucleolar prominence, concentric layering of cellular stroma around neoplastic glands, and a combination of normal-appearing cells with cells having large nuclei with prominent nucleoli.4 The histology may also demonstrate stromal and perineural invasion. p53 gene expression is seen in 94%.49