Figure 14.1.1
Trisomy 13 with holoprosencephaly, hypotelorism, echogenic kidneys, and midline facial defect. A: Coronal image of fetal head demonstrating fusion of the ventricles into a large monoventricle (arrows) and absence of the falx, characteristic of alobar holoprosencephaly. B: Coronal image of the face showing the orbits (arrows) abnormally close together. C: Transverse image of fetal abdomen demonstrating enlarged, echogenic kidneys (arrows). D: Coronal image of face showing midline facial defect (arrow).
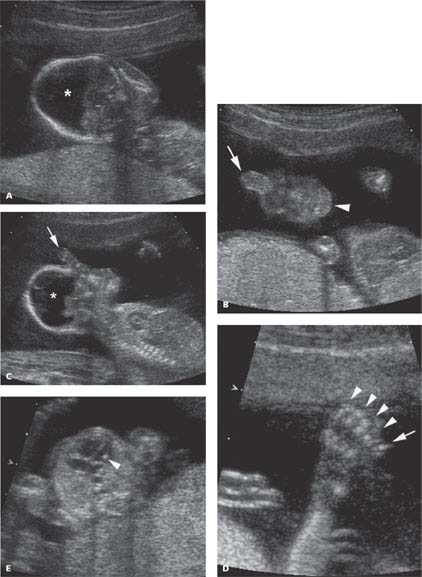
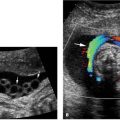
Figure 14.1.2
Trisomy 13 with holoprosencephaly, proboscis, polydactyly, and echogenic intracardiac focus. A: Coronal image of fetal head showing large monoventricle (*) of alobar holoprosencephaly. B: Coronal image of face showing elevated and upward pointing proboscis (arrow) instead of a normal nose. The arrowhead points to the chin. C: Sagittal image of face demonstrating very abnormal profile with proboscis (arrow) extending superiorly from the upper part of the face. The large monoventricle (*) is visible in the head. D: Image of clenched fist demonstrating four digits together (arrowheads) and an extra digit (arrow) next to the little finger, protruding from the side of the hand. E: Transverse image of thorax with four-chamber view of the heart showing a bright echo within the left ventricle (arrowhead), representing an echogenic intracardiac focus.
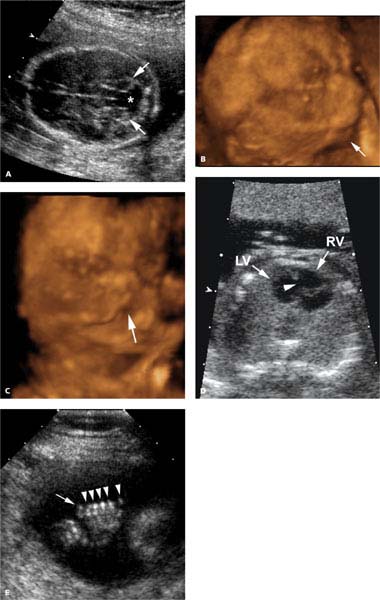
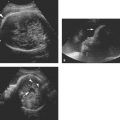
Figure 14.1.3
Trisomy 13 with Dandy–Walker malformation, micrognathia, midline facial cleft, atrioventricular canal, and polydactyly. A: Axial image of fetal head demonstrating splaying of the cerebellar hemispheres (arrows) in the posterior fossa and absence of the vermis, as well as fluid (*) extending from the region of the fourth ventricle to the cisterna magna, representing a Dandy–Walker cyst. B: 3D image of face in profile showing very small chin (arrow). C: 3D image of front of face demonstrating midline cleft in upper lip (arrow). D: Transverse view of the thorax demonstrating a large defect in the ventricular septum (arrowhead) and abnormal appearing atrioventricular valves, characteristic of an atrioventricular canal cardiac anomaly (LV arrow = left ventricle, RV arrow = right ventricle). E: Image of hand showing thumb and four fingers (arrowheads) in fist with an extra digit (arrow) next to the little finger.
14.2. Trisomy 18 (Edwards Syndrome)
Description and Clinical Features
Trisomy 18 is a chromosomal anomaly in which the fetus has an extra chromosome 18 (i.e., it has three, instead of the normal two, chromosomes 18). It is a rare anomaly, occurring in approximately 3 per 10,000 births. Like other trisomies, the incidence increases with advancing maternal age. Fetuses with trisomy 18 generally have severe structural anomalies involving multiple organ systems. Most die within the first year of life, and the few long-term survivors are severely neurologically impaired.
Sonography
Many of the structural anomalies in fetuses with trisomy 18 can be identified by ultrasound. Among these are the following:
Central nervous system
Agenesis of the corpus callosum
Choroid plexus cysts
Hypoplastic cerebellum with enlarged cisterna magna
Strawberry-shaped skull
Face
Micrognathia
Hypotelorism
Microphthalmia
Neck
Cystic hygroma
Extremities
Clenched hand with overlapping index finger
Limb contractures
Clubfoot
Rocker bottom foot
Omphalocele
Diaphragmatic hernia
Cardiac anomalies
Renal anomalies
Intrauterine growth restriction
When a constellation of anomalies, including several of the above, is detected by ultrasound (Figures 14.2.1 to 14.2.3), the diagnosis of trisomy 18 should be considered and amniocentesis should be offered. Furthermore, several anomalies that occur in trisomy 18 carry an increased incidence of aneuploidy even when seen as an isolated finding (e.g., microphthalmia, clenched hand with overlapping index finger, rocker bottom foot, omphalocele, diaphragmatic hernia) and thus should prompt consideration of amniocentesis.
Fetuses with trisomy 18 have an increased incidence of choroid plexus cysts (Figure 14.2.4) in the second trimester compared to fetuses with normal chromosomes. Since choroid plexus cysts may be seen in normal fetuses as well as fetuses with trisomy 18, a choroid plexus cyst is considered a “marker” for trisomy 18, not a congenital anomaly. The presence of this “marker” increases the likelihood that the fetus has trisomy 18. The risk of trisomy 18 is even higher in fetuses found to have choroid plexus cysts together with another anomaly (Figures 14.2.5 and 14.2.6), especially one of the anomalies listed above.
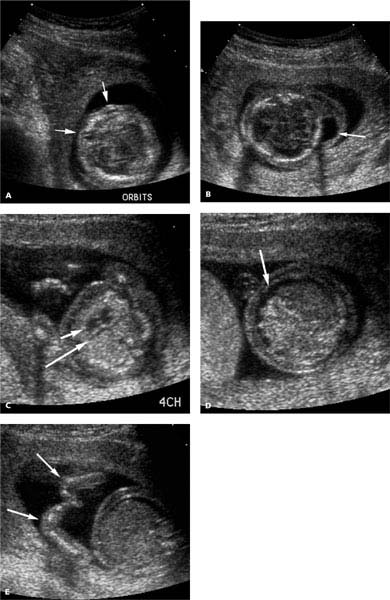
Figure 14.2.1
Trisomy 18 with microphthalmia, nuchal cystic hygroma, hypoplastic left heart, ascites, and persistent flexion of the wrists. A: Axial image through upper face showing hypoplastic orbits (arrows). B: Image through head and upper neck demonstrating a fluid collection in soft tissues of neck, representing a cystic hygroma (arrow). C: Image of four-chamber heart showing small left ventricle (long arrow) and normal right ventricle (short arrow). D: Axial image of abdomen demonstrating ascites (arrow). E: View of both hands showing abnormal flexion of both wrists (arrows).
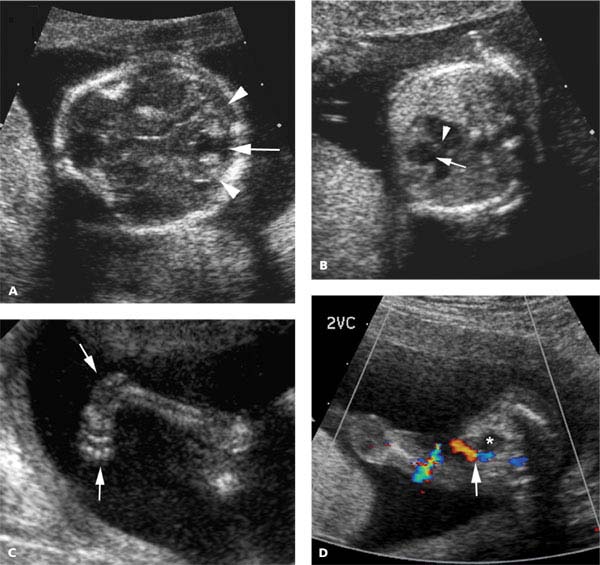
Figure 14.2.2
Trisomy 18 with Dandy–Walker malformation, cardiac defect, clubfoot, and single umbilical artery. A: Axial image of posterior fossa showing absence of the cerebellar vermis, with fluid (arrow) between the cerebellar hemispheres (arrowheads) connecting the fourth ventricle to the cistern magna. B: Four-chamber view of the heart showing a large ventricular septal defect (arrow) and defects in both atrioventricular valves (arrowhead). C: Image of lower extremity demonstrating clubfoot (arrows). D: Axial color Doppler image of pelvis showing single umbilical artery (arrow) on one side of the bladder (*).
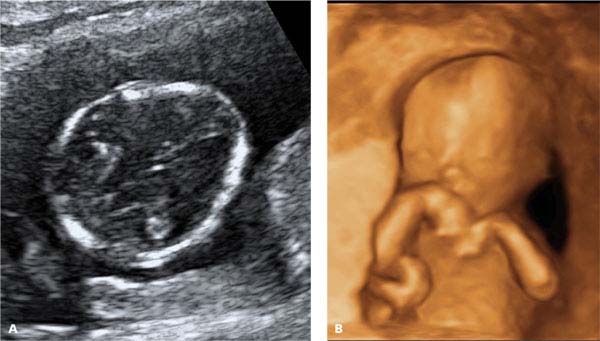
Figure 14.2.3
Trisomy 18 with strawberry skull and persistent wrist flexion. A: Axial image of head demonstrating strawberry-shaped cranium. B: 3D image of fetus demonstrating abnormal flexion of both wrists.
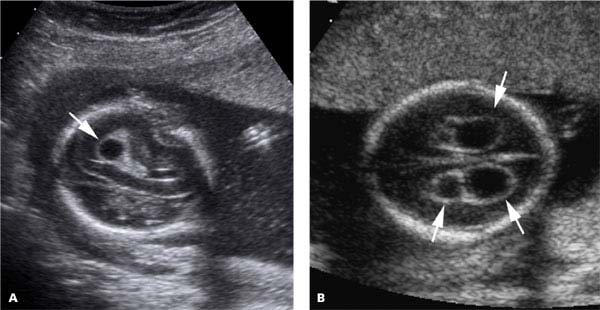
Figure 14.2.4
Choroid plexus cysts. A: Oblique image of fetal head showing single choroid plexus cyst (arrow). B: Axial image of fetal head showing multiple bilateral choroid plexus cysts (arrows).
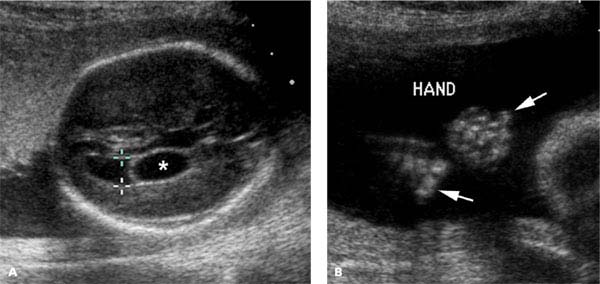
Figure 14.2.5
Trisomy 18 with choroid plexus cyst and clenched hands with overlapping digits. A: Axial image of head showing cyst (*) within the choroid plexus of the lateral ventricle (calipers). B: Image of both hands showing abnormal overlapping of index finger over middle finger bilaterally (arrows).
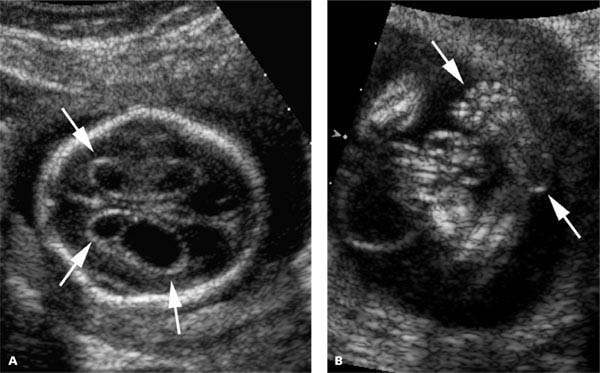
Figure 14.2.6
Trisomy 18 with choroid plexus cysts and clubfoot. A: Axial image of head showing bilateral choroid plexus cysts (arrows). B: Image of clubfoot (arrows).
14.3. Trisomy 21 (Down Syndrome)
Description and Clinical Features
Trisomy 21 is a chromosomal anomaly in which the fetus has an extra chromosome 21 (i.e., it has three, instead of the normal two, chromosomes 21). It is the most common chromosomal anomaly in newborns, occurring in 1 per 700 births. Like other trisomies, the incidence of trisomy 21 increases with advancing maternal age.
Fetuses with trisomy 21 have increased incidence of cardiac defects, duodenal atresia, and other structural anomalies. Trisomy 21 is not usually fatal unless there is a life-threatening cardiac structural defect. Children and adults with trisomy 21 have subnormal intelligence.
Sonography
Many of the structural anomalies in fetuses with trisomy 21 can be identified by ultrasound. Among these are the following:
Cerebral ventriculomegaly
Macroglossia
Neck
Cystic hygroma
Thickened nuchal translucency at 11–14 weeks
Thickened nuchal fold (≥5–6 mm) at 16–20 weeks
Cardiac
Atrioventricular canal
Ventricular septal defect
Tetralogy of Fallot
Thorax
Pleural effusion
Pericardial effusion
Duodenal atresia
When one or more of these anomalies is detected by ultrasound (Figures 14.3.1 to 14.3.3), the diagnosis of trisomy 21 should be considered and amniocentesis should be offered.

Figure 14.3.1
Trisomy 21 with hydrocephalus and duodenal atresia. A: Axial image of fetal head showing dilated lateral ventricle (calipers) measuring 1.15 cm. B: Axial image of upper abdomen showing two dilated cystic structures, representing the dilated stomach (S) and dilated duodenal bulb (D), characteristic of duodenal atresia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree