4 Chronic Obstructive Pulmonary Disease and Diseases of the Airways
Chronic obstructive pulmonary disease (COPD) is very common and has been reported as being second only to arteriosclerosis as a cause of disability and absence from work (Heitzman 1993, Hofner et al. 1977).
COPD is characterized by increased airway resistance and obstructive-type ventilatory impairment. The term has a strong correlation with a smoking history and encompasses two main disorders:
- Emphysema
- Chronic bronchitis
Diseases of the airways are characterized by increased airway resistance, sputum production, obstructive type ventilatory impairment, and air trapping.
Diseases of the airways include:
- Bronchiectasis
- Small airway disease/bronchiolitis
- Bronchial asthma
Emphysema is common in the elderly. Mild degrees of emphysematous change are found in two-thirds of all autopsies while more severe forms are present in approximately 10% of cases (Otto 1976, Thurlbeck and Müller 1994).
The word emphysema means “lung overinflation” (emphysein = to inflate). We define this entity as “a chronic and irreversible dilatation of the airspaces distal to the terminal bronchiole with associated destruction of their walls” (World Health Organization 1961).
Emphysema may lead to significant respiratory impairment with resulting dyspnea, cyanosis, and eventual cor pulmonale.
The classification of emphysema most commonly used today is based on the anatomical distribution of lung destruction. This subdivision into three main groups is as follows: centrilobular (centriacinar, proximal acinar), panlobular (panacinar), and paraseptal (distal acinar). This “pathological” classification of emphysema is useful as it correlates with findings on high-resolution computed tomography (HRCT).
In practice, the diagnosis of emphysema usually is based on the appropriate clinical history, abnormal pulmonary function tests, reduced diffusing capacity, and a chest radiograph showing pulmonary hyperinflation. However, as both standard chest radiographs and pulmonary function tests are relatively insensitive to the presence of early disease, HRCT is useful when there is diagnostic uncertainty (Webb et al. 1992).
Pathology
Destruction of alveolar septa reduces both the surface area available for gas exchange and the total crosssectional area of the pulmonary vessels. This leads to increased vascular resistance and pulmonary hypertension. A further pathophysiologic phenomenon is ventilation-perfusion mismatch: in normal individuals the von Euler-Liljestrand reflex, also known as hypoxic vasoconstriction, regulates regional perfusion and matches it to ventilation. In emphysema, this control mechanism is lost and very poorly ventilated regions continue to be perfused. This results in an effective venoarterial shunt with systemic arterial hypoxemia.
Macroscopically, the lungs are large and hyperinflated. Emphysematous change may be patchy in distribution and interspersed between areas of normal lung. The lungs do not collapse when the chest is opened as elastic recoil is diminished. The diaphragm is depressed and hypertrophic, sagittally oriented muscle fibers may indent the surface of the liver.
Dilated confluent airspaces result from destruction of both alveolar and lobular septa. They may form bullae, which are air-containing cystic cavities greater than 1 cm in diameter (bullous emphysema). Bullae occupying more than one-third of the lung are known as giant bullae.
The resulting pulmonary arterial hypertension leads to ectasia and sclerosis of the pulmonary arteries and right ventricular hypertrophy. Eventually, right ventricular decompensation may supervene (cor pulmonale).
Clinical Features
Manifestations of emphysema include dyspnea and cyanosis. Transitional forms are common but sometimes it is possible to identify specific clinical patterns:
- “Pink puffer”: These individuals usually are thin and dyspneic. However, they are not cyanosed and clinical features indicating the presence of associated chronic bronchitis are absent.
- “Blue bloater”: These are “heavy-set” individuals who are cyanosed and have concomitant chronic bronchitis.
Physical examination reveals a barrel chest, relatively shallow respirations, and hyperresonance to percussion. Spirometry shows increased FVC, diminished FEV1, and decreased FEV1/FVC ratio. Blood gas analysis reveals arterial hypoxemia and hypercapnia particularly in blue bloaters. Arterial oxygen and carbon dioxide levels may be relatively normal in pink puffers.
Radiologic Findings
Chest Radiograph
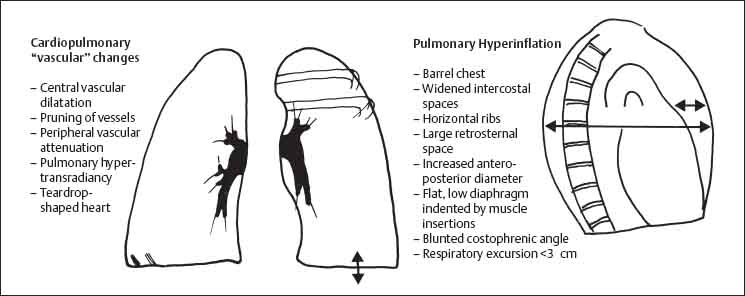
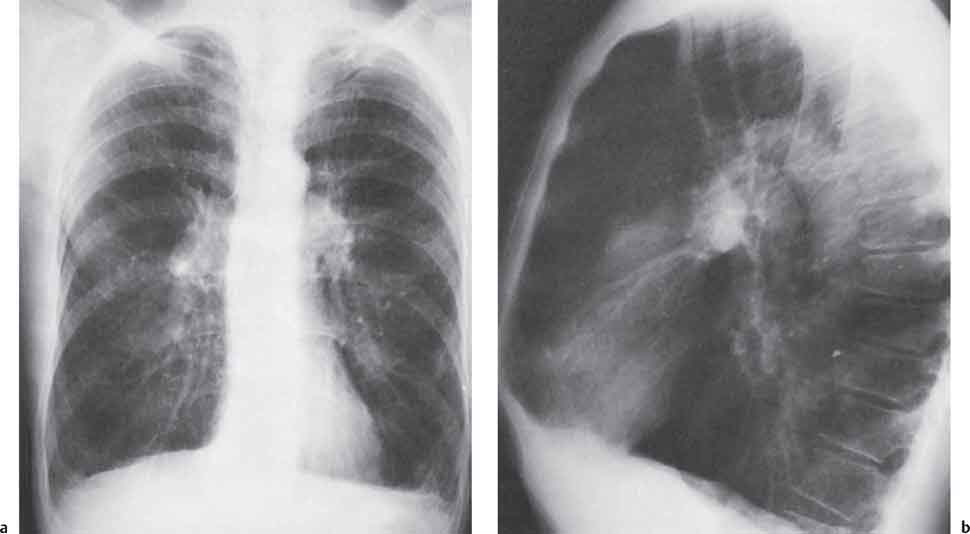
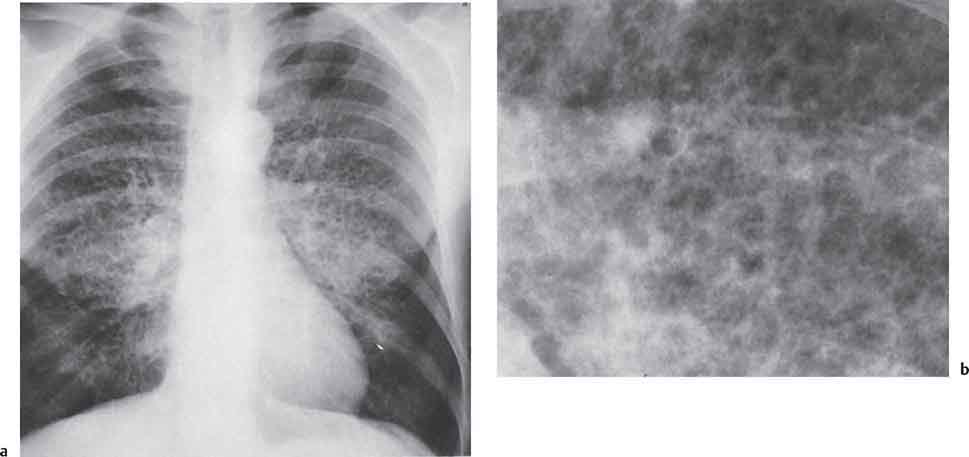
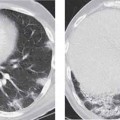
Findings on the chest radiograph are secondary to pulmonary hyperinflation with subsequent deformity and/ or displacement of the chest wall, heart, and diaphragm. There is also attenuation and disorganization of the pulmonary vasculature with features of oligemia and pulmonary hypertension (Figs. 4.1 and 4.2).
- Barrel chest: Sagittal chest diameter is increased, the posterior ribs have a horizontal orientation, and the intercostal spaces are widened.
- Diaphragmatic depression: Findings include flattening of the domes of the diaphragm and a costophrenic angle of approximately 90° (so-called “pseudoblunting”). On the lateral view, the diaphragm may show inferior convexity. Respiratory diaphragmatic excursion is also restricted (<3 cm in emphysema vs. normal values of 5–10 cm).
- Small, vertically orientated cardiac shadow: In the presence of a relatively low diaphragm, the heart assumes a vertical orientation and cardiothoracic ratio decreases on the frontal radiograph. There may also be a degree of left ventricular atrophy as left heart filling and left ventricular output sometimes are reduced in patients with emphysema, especially in cases complicated by cor pulmonale.
- Increased retrosternal space: On the lateral radiograph, the retrosternal space is widened due to both the increased sagittal diameter of the chest and the relatively “small” heart.
- Dilatation of the central pulmonary arteries: Increased pulmonary vascular resistance and subsequent pulmonary arterial hypertension lead to dilatation of the central pulmonary arteries. This is manifest as bilateral symmetric hilar enlargement on the chest radiograph.
- Rapid tapering of pulmonary vessels: The dilated central vessels decrease markedly in caliber at the segmental level. This may occasionally give the appearance of an “amputated hilum.”
- Attenuation of peripheral pulmonary vessels: The combination of pulmonary hyperinflation together with attenuation of peripheral vessels results in increased lucency in the lung periphery.
- Marker vessels: Emphysema is often focal in distribution. In these cases, pulmonary blood flow will be redistributed to areas of relatively normal lung and result in regional vascular dilatation. In addition, emphysematous bullae may compress adjacent normal lung and cause crowding, displacement, and draping of vessels. These findings are best appreciated on conventional and computed tomography (CT).
- Bullae: Thin-walled emphysematous spaces greater than 1 cm in diameter sometimes are visible on the chest radiograph. However, CT will show these thin-walled, air-filled cysts much more convincingly.
- Increased bronchovascular markings: Emphysema often is found in association with chronic bronchitis. Peribronchovascular fibrosis is found in the latter and is manifest as tortuosity, poor definition, and segmentation of vascular shadows (increased pulmonary markings, “dirty chest,” Thurlbeck and Müller 1994).
- Atypical appearance of pneumonia and pulmonary edema: Emphysema may alter the radiographic appearance of other pulmonary diseases. Conversely, emphysema frequently becomes apparent on the chest radiograph only when common disorders such as pneumonia and pulmonary edema supervene (Fig. 4.3). Pneumonic consolidation and cardiogenic edema develop with relative sparing of regions of avascularity. Therefore, emphysematous lung that is devoid of capillaries tends to be spared. This results in nonhomogeneous, relatively coarse infiltration. Pulmonary edema may be asymmetrical or localized depending on the distribution of emphysematous involvement.
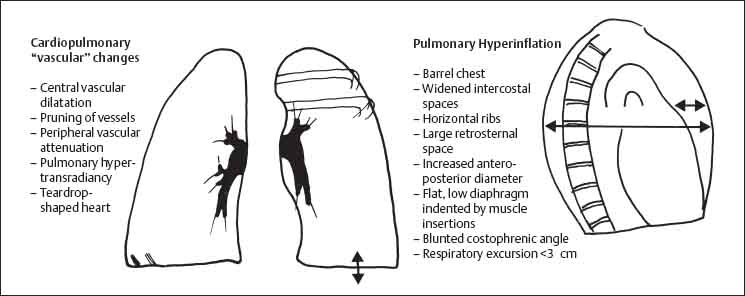
Fig. 4.1 Pulmonary emphysema.
Computed Tomography
Correlation between CT and spirometric data has been reported to be relatively poor (Miller 1989). HRCT, however, is valuable in detection of early disease. It is also possible to classify emphysema on the basis of findings on HRCT:
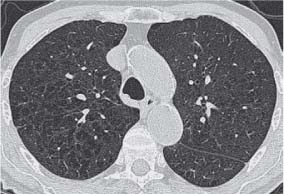
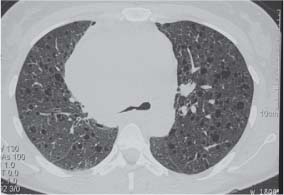
- Centrilobular emphysema: Centrilobular emphysema classically develops in the setting of chronic bronchitis and shows a predilection for the upper lobes. Alveolar destruction is mainly around the respiratory bronchioles at the center of the pulmonary acinus and therefore involves the center of the secondary pulmonary lobule (Webb et al. 1992). HRCT shows centrilobular areas of low attenuation, sometimes several millimeters in diameter. These foci have imperceptible walls, which helps in differentiating them from cysts, bronchiectasis, and the honeycombing of pulmonary fibrosis (Figs. 4.4, 4.5).
- Panlobular emphysema: This is characterized by destruction of alveoli throughout the lobule. Panlobular emphysema is associated with α1-antitrypsin deficiency and has a predilection for the lower lobes. This is an autosomal recessive disease associated with low serum levels of α 1-antitrypsin. Homozygotes have 20% of normal enzyme activity. This deficiency allows leucocyte proteases to attack and destroy the lung parenchyma with changes most marked in regions of maximal perfusion (i. e. the basal zones). Clinical presentation is most common in the fourth decade of life. HRCT shows panlobular low attenuation which persists on expiratory views (Fig. 4.6).
- Paraseptal emphysema, a form of bullous emphysema with a familial tendency, is characterized by subpleural bullae (Fig. 4.7). It usually is asymptomatic unless complicated by a spontaneous pneumothorax.
- HRCT will show subpleural and perifissural bullae and CT studies have shown a high incidence of apical paraseptal emphysema in young adults presenting with spontaneous pneumothorax (Lesur 1990).
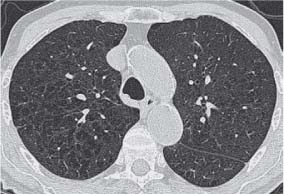
Fig. 4.4 Centrilobular emphysema. HRCT shows areas of decreased lung attenuation lying centrally within the secondary pulmonary lobule.
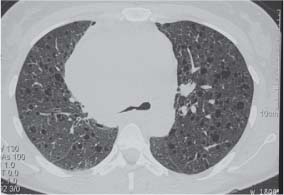
Fig. 4.5 Centrilobular emphysema.
Quantification of abnormally low lung attenuation due to emphysema is possible with volumetric CT acquisition and three-dimensional reconstructions using a threshold for inspiratory studies of approximately -900 Hounsfield units. This method has been reported as showing good correlation with pulmonary function tests (Mergo et al. 1998).