12 High-Resolution/Thin-Section CT Patterns in Pulmonary Disease
Computed tomography (CT) is more sensitive and more specific than the chest radiograph in evaluation of pulmonary disease. A specific diagnosis can sometimes be made from CT findings as in centrilobular emphysema. In other cases, for example ground-glass opacification (GGO), CT findings are less specific and a differential diagnosis may only be possible. This may reflect the fact that the lung’s response to different insults is, in many cases, relatively isomorphic. It is, however, frequently possible to shorten the differential diagnosis when the clinical history and the duration of symptoms and radiologic findings are considered.
The following CT patterns will be considered:
- Ground-glass opacification and consolidation
- Multifocal peripheral consolidation
- Pulmonary nodules
- Intra- and interlobular septal thickening and reticular pattern
- Decreased lung attenuation and cystic lung change
- Inhomogeneous-mosaic lung attenuation
Ground-glass opacification reflects partial filling of the alveoli, sometimes with a degree of associated interstitial change, the latter generally being below the resolution of computed tomography. Lung attenuation is increased but this increase is not sufficient to obscure vascular markings in contradistinction to consolidation.
The difference in attenuation values between the infiltrated lung parenchyma and air-filled bronchi is larger than between normal lung and air-filled bronchi; this increased contrast leads to increased conspicuity of the bronchus, the so called “black bronchus” sign.
The differential diagnosis of pulmonary ground-glass opacification includes acute and nonacute disease processes:
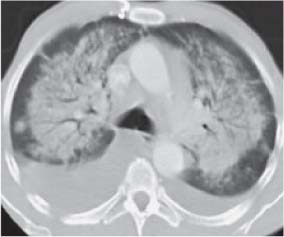
- Acute infection including Pneumocystis Jiroveci/Carinii Pneumonia (PJP; PCP): This infection is characteristically seen in patients with diminished cellular immunity and has been considered an index case for progression to AIDS in HIV-positive patients for many years. GGO may be uniform or inhomogeneous in distribution and may progress to frank consolidation (Fig. 12.1; see also Chapter 3, p. 87).
- Acute Pulmonary Hemorrhage: Acute pulmonary hemorrhage may be seen in a number of disease processes including Wegener’s Granulomatosis and Anti-Glomerular Basement Membrane disease. It also may be seen in hematologic disorders and particularly in the acute leukemias where it may be a manifestation of disease-induced bone marrow failure or a complication of chemotherapy-induced thrombocytopenia.
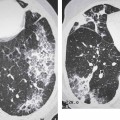
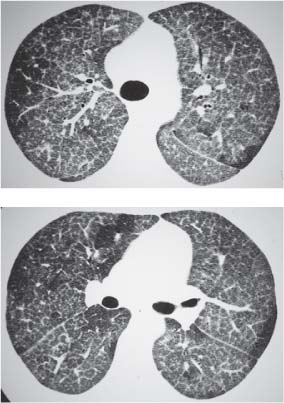
- Pulmonary Edema: Ground-glass opacification probably reflects a combination of interstitial and early alveolar edema. It characteristically has a dependent distribution and may involve the posterior portions of the upper lobes in patients confined to bed. “Smooth” interlobular septal thickening is also frequently present and probably reflects predominantly associated interstitial edema (Fig. 12.2).
- Hypersensitivity Pneumonitis/Extrinsic Allergic Alveolitis: Ground-glass opacification in a patchy or homogeneous distribution is a frequent finding in hypersensitivity pneumonitis (see also Hypersensitivity Pneumonitis, Chapter 5, p. 145).
- Respiratory Bronchiolitis-Interstitial Lung Disease (RBILD) and Desquamative Interstitial Pneumonia (DIP): Centrilobular nodules of GGO and GGO involving the entire secondary pulmonary lobule are manifestations of RBILD-DIP with a tendency towards more extensive and uniform change within the lobule in DIP (see also Idiopathic Interstitial Pneumonias, Chapter 3, p. 95).
- Lymphocytic Interstitial Pneumonia (LIP): LIP in adult HIV-negative patients is frequently found in patients with Sjögren syndrome. Ground-glass opacification, areas of consolidation, and pulmonary cysts are frequent CT findings (see also Sjögren syndrome, Chapter 3, p. 102).
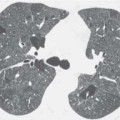
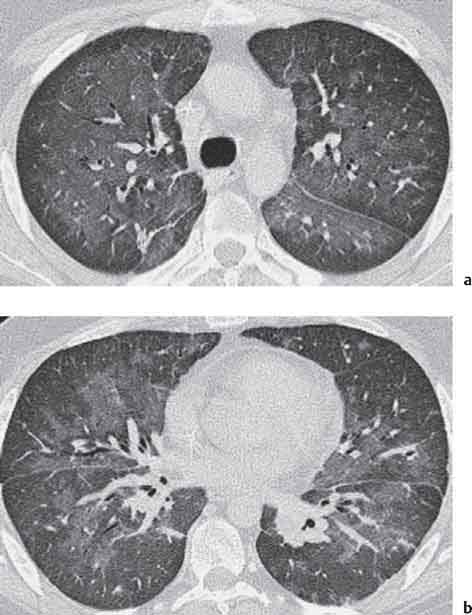
- Alveolar Proteinosis: The etiology of this rare disease is unknown but it may relate to a hereditary defect of surfactant production which decompensates to a pathologic state when additional infectious or toxic insults are imposed (e.g., the inhalation of tobacco smoke, silicates, aluminum, kaolin, or sawdust). Pathologically, the alveoli are filled with copious protein- and phospholipid-rich material. CT features are GGO in association with septal thickening leading to the characteristic “crazy paving” appearance (Fig. 12.3a, b).
- Peripheral Adenocarcinoma: Focal areas of persisting GGO may reflect slow growing adenocarcinomas with a lepidic pattern of growth (see also Solitary Pulmonary Nodule, Chapter 6, p. 149 and Noguchi Classification, Chapter 6, p. 161).
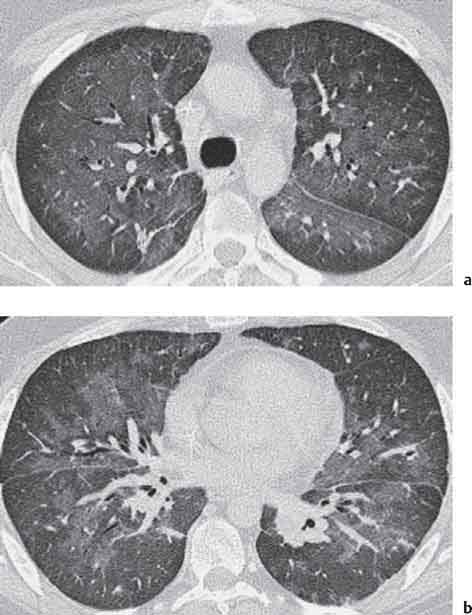
Fig. 12.1a, b Pneumocystis pneumonia. High-resolution CT image shows bilateral ground-glass opacification with evidence of the “black bronchus” sign and with sparing of the subpleural lung.
Fig. 12.2 Pulmonary edema with bilateral pleural effusions.
Fig. 12.3a, b Alveolar proteinosis. CT images show marked septal thickening superimposed on ground-glass opacification and giving the “crazy paving” pattern.
- Multifocal Bronchioloalveolar Carcinoma: Bronchioloalveolar carcinoma showing a lepidic growth pattern characteristically shows pulmonary consolidation in a peribronchial distribution.
- Pulmonary Lymphoma: Pulmonary lymphoma is characterized by nodular and linear areas of increased attenuation and consolidation. These changes tend to have their epicenter on the airway which may appear dilated and they correlate histologically with lymphomatous infiltration in a peribronchovascular distribution.
- Organizing Pneumonia: Organizing pneumonia or cryptogenic organizing pneumonia represents an organizing pneumonia and a “proliferative” bronchiolitis. High-resolution CT (HRCT) shows areas of consolidation and ground-glass opacification in a peripheral subpleural distribution (see Fig. 4.26a, b).
- Chronic Eosinophilic Pneumonia: CT manifestations of chronic eosinophilic pneumonia include peribronchial consolidation that may have a peripheral subpleural distribution in up to 50% of cases.
The distribution of pulmonary nodules on thin collimation/high-resolution CT images allows their classification into centrilobular, perilymphatic, and random in type.
Centrilobular nodules are characteristically a manifestation of small airways disease-cellular bronchiolitis
Only gold members can continue reading.
Log In or
Register to continue
![]()