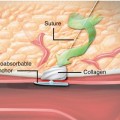
Fig. 23.1
Single-vessel chronic total occlusions
There were four scenarios which were deemed to be appropriate for revascularization in the setting of the single-vessel CTO. These four scenarios included patients with severe angina (CCS Class 3 or 4) who were treated with maximum medical therapy (two or more antiangina drugs), regardless of the risk associated with noninvasive imaging (low, intermediate, or high). One additional scenario included patients with mild angina (CCS Classes 1 and 2) who were on maximal therapy and found to have high-risk noninvasive imaging features. There were six clinical scenarios deemed to be inappropriate. These included patients that were asymptomatic, not on maximal medical therapy, regardless of the noninvasive risk assessment and those who were found to have low risk stress testing and on less than two anti-ischemic drugs regardless of their symptom classification (none, mild, or severe). The remaining nine clinical scenarios were deemed to be of uncertain appropriateness.
Recall that appropriate is defined as highly likely to confer benefit to the patient, inappropriate was unlikely to confer benefit to the patient, and uncertain was uncertainty based upon a lack of data, to confer benefit to the patient. While these criteria were intended to inform physicians, payers and patients as to the appropriateness of “revascularization,” these criteria have been used and in the future will be used to address the appropriateness of PCI specifically [7].
Figure 23.2 illustrates the eighteen clinical scenarios that include patients with one- or two-vessel disease not involving the proximal LAD. It is particularly interesting to note that there are five down codes in the appropriateness of the single-vessel chronic total occlusion in comparison to one- or two-vessel disease not involving the proximal LAD (i.e., non-CTO disease).
Fig, 23.2
Eighteen clinical scenarios that include patients with one- or two-vessel disease not involving the proximal LAD
Symptomatic Patients
Considering the four scenarios where appropriateness is downgraded among patients with symptoms and a single-vessel CTO compared to a subtotal lesion, it is difficult to imagine that a patient with a chronic total occlusion would derive less benefit from revascularization than patients with a chronic subtotal occlusion. Take for instance two patients with mild angina on maximal medical therapy with intermediate risk noninvasive imaging studies. One has a 70 % mid right coronary artery lesion and receives PCI or bypass surgery. That procedure would be graded as appropriate. The other patient has a 100 % mid right coronary artery lesion. Revascularization with either PCI or CABG surgery in this case would be considered of uncertain appropriateness. While an uncertain rating does not preclude revascularization, it does imply less certainty over benefit. This can no longer be argued in light of several studies, some recent and some not so recent [8–10].
Whether assessed by physician reported (CCS class) or patient reported methods (e.g., the Seattle Angina Questionnaire [11]), successful CTO PCI is associated with improvements in symptoms and quality of life as compared to unsuccessful CTO PCI. Recently, Safley and colleagues [12] have shown that CTO PCI was as effective at alleviating symptoms and restoring physical function and quality of life as non-CTO disease (Table 23.1). In this study, the final Seattle Angina (SAQ) scores and Rose dyspnea scale scores among the CTO group were equal to the non-CTO group despite lower success rates in the CTO groups (86 % vs. 96 %, p < 0.05).
Table 23.1
Success of CTO vs. no CTO
CTO n = 124 | No CTO n = 1833 | ||
|---|---|---|---|
Baseline health status | |||
SAQ physical limitation score | 72.1 ± 26.9 | 77.9 ± 23.4 | 0.016 |
SAQ angina frequency score | 70.1 ± 28.1 | 72.9 ± 23.6 | 0.212 |
SAQ quality of life score | 54.3 ± 25.5 | 56.0 ± 25.4 | 0.487 |
Rose dyspnea score | 1.9 ± 1.5 | 1.7 ± 1.5 | 0.209 |
6-month health status | |||
SAQ physical limitation score | 96.2 ± 12.8 | 95.7 ± 12.9 | 0.742 |
SAQ angina frequency score | 91.0 ± 19.0 | 93.2 ± 15.1 | 0.126 |
SAQ quality of life score | 80.6 ± 21.4 | 80.5 ± 19.9 | 0.951 |
Rose dyspnea score | 1.0 ± 1.4 | 0.9 ± 1.3 | 0.497 |
One scenario does preclude revascularization for CTO but not non-CTO disease. Consider the patient with Class 3 or 4 angina on less than two anti-ischemic drugs and a low risk noninvasive imaging study. Revascularization in a patient with these characteristics and a 70 % mid right coronary artery lesion would be of uncertain appropriateness, whereas if the lesion were a chronic total occlusion, revascularization would be deemed inappropriate. Again, it is inconceivable that the patient with a symptom causing CTO would be less likely to benefit from revascularization than one with a symptom causing non-CTO. It cannot be argued that concerns over procedural safety drove this inconsistency because revascularization could have been done by CABG surgery, which carries the same risk no matter what the severity of occlusion.
Especially among those patients who are symptomatic, the systematic down coding in the appropriateness of revascularization for patients with chronic total occlusions is illogical, even when applying the AUC solely to percutaneous revascularization. There is no doubt that revascularization confers the benefit of angina relief among patients with CTOs, especially when the revascularization method is PCI. These logical incongruities violate the principle that revascularization should be offered based upon the patient’s needs as reflected in their symptoms, not the angiogram, and should be corrected in future AUC updates.
Asymptomatic Patients
It can be argued that PCI outside of the setting, acute coronary syndrome does not confer a survival advantage. This contention however is being challenged by a plethora of data suggesting a potential of survival benefit no matter what method of ischemic burden reduction is used. There is now sufficient equipoise to warrant a randomized controlled trial of PCI vs. medical therapy based on the baseline ischemic burden (ISCHEMIA trial www.NIH.gov).
It has long been suggested that among patients with a CTO successful PCI, compared to unsuccessful CTO PCI, there is associated survival advantage. Among patients who are asymptomatic, with a high-risk stress test, on maximal medical therapy and with a subtotal culprit lesion, revascularization is deemed appropriate. However, when the culprit is a CTO, revascularization is rated of uncertain appropriateness.
CTO PCI and Survival
In 2001, Suero and colleagues published the first retrospective analysis that suggested there may be an association between successful CTO PCI and survival [13]. These findings have been reproduced by several other groups and institutions and have also been challenged. In a recent meta-analysis of 13 reports of success vs. failed CTO PCI, Joyal et al. found that the odds ratio of death during the variable time of follow-up among the reports was 0.56 with a 95 % confidence interval of 0.43–0.72 and p < 0.0001 [9]. While retrospective analyses are potentially confounded and can only be used in hypothesis generation there is no potential for a US randomized controlled trial (RCT) to definitively address this hypothesis. There are two efforts to test the hypothesis through an RCT outside the United States, one in Southeast Asia (DISCOVER CTO, www.NIH.gov) and the EuroCTO trial. It will be 5–10 years before these trial results are known, and until then practicing cardiologists will face the difficult decision of whether or not to offer CTO PCI to asymptomatic patients with CTOs. To say that there is no evidence to support CTO PCI among asymptomatic patients is as dishonest as claiming that there is irrefutable evidence supporting CTO PCI. Therefore, patients must be informed about ALL of the data that exists and must be engaged in the decision to proceed with revascularization or medical therapy alone.
In order for a hypothesis to warrant testing, there must be biological plausibility. There are, indeed, several studies in CTO patients where specific mechanism of benefit are suggested, and the findings corroborate the survival hypothesis.
Ischemia is associated with adverse event and many CTOs, even those that are “well collateralized result in ischemia [14]. Hachamvitch and colleagues described a linear relationship between ischemic burden and mortality [15]. This was confirmed and extended in the nuclear substudy of the COURAGE trial where baseline ischemic burden was again linearly related to 3-year death and MI rates [16]. Further, Shaw et al. reported that among patients in the COURAGE trial with moderate to large ischemic burden, PCI was more effective than medical therapy at reducing the ischemic burden by at least 5 % and amount previously shown to be prognostically significant.
Safley and colleagues evaluated the ischemic burden reduction among 312 patients with CTO who were successfully treated [17]. They found that the baseline ischemic burden was associated with the likelihood of reducing the ischemic burden by 5 % or more. Using a receiver operator model, they found that a baseline ischemic burden of greater than 12.5 % of the LV mass was predictive of a 5 % reduction in ischemia, whereas a baseline ischemic burden of less than 6.25 % was associated with an increase in ischemic burden by 5 %. A 5 % reduction in ischemic burden was associated with improved survival as compared to those with minimal or no reduction in ischemia.
Another plausible mechanism of increased mortality due to a CTO is the “double jeopardy” theory. Multivessel disease in the setting of an acute myocardial infarction (AMI) is associated with excess mortality as compared to single-vessel disease. Dutch investigators have demonstrated that this excess mortality is mostly attributable to the presence of a CTO [18]. They confirmed and extended this observation in a subsequent study landmarked at 30 days and showed continued divergence of the survival curves over time with the highest mortality among patients who present with AMI and are found to have a CTO in a nonculprit vessel (18 % at 5 years after 30-day landmarking), followed by those with AMI and significant non-CTO disease (11 % at 5 years after 30-day landmarking) and then those who present with AMI and no other significant CAD (10 % at 5 years after 30-day landmarking) [ 19]. Further, CTO was associated with the development of left ventricular dilation and/or a fall in ejection fraction (HR 3.5 95 % CI 1.6–7.8, p < 0.01). These observations lead to the initiation of the EXPLORE trial. The EXPLORE trial will test the hypothesis that early CTO PCI (within the index hospitalization) as compared to no CTO PCI will result in improved ejection fraction and less LV remodeling as assessed by MRI at 4 months after AMI. It is not powered for testing a mortality endpoint.
Recently, the VACTO study demonstrated that among patients who had undergone AICD implantation for primary prevention and had incomplete revascularization, the appropriate arrhythmia therapy (antitachycardia pacing or defibrillation) during the 3 year follow-up timeframe was 30 % among those with a CTO and 15 % among those with non-CTO incomplete revascularization, p < 0.01 [20].
Taken together, these observations suggest that CTOs are associated with adverse events including death, MI, potentially fatal arrhythmias, and adverse LV remodeling regardless of the symptom status. There is only one randomized controlled trial designed to test the hypothesis that CTO PCI will alter the course of adverse events among asymptomatic patients based on any of these hypotheses, the EXPLORE trial. Hopefully results from that trial will be available in the next 3–4 years to help guide decision-making. Unfortunately that trial is not powered for a mortality endpoint, so these surrogates for survival (LV remodeling and EF) will have to suffice. Again, fully informed consent, which includes a discussion of these nuances and incorporates the patient’s wishes, should precede CTO PCI procedures.
In summary, CTO PCI is noninferior to non-CTO PCI when it comes to relief of symptoms (including dyspnea), restoration of physical function, and restoration of quality of life. In the absence of symptoms, there are compelling data supporting the hypothesis that CTO PCI is associated with a mortality benefit. Without a full armamentarium of techniques to enhance procedural success and safety, interventional cardiologists are likely to deny their patients access to this form of effective therapy. When faced with a patient who has a CTO, the operator need only ask himself, “if it were 90 %, would I perform PCI?” If the answer is affirmative, there is an obligation to perform the procedure or refer the patient to a competent CTO operator.
Classic Technique and the Myth of the True Lumen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree