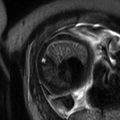
Fig. 1.1
Placenta percreta in a 28-year-old pregnant woman at 34 weeks’ gestation. Sagittal T2-FSE (a) and coronal T2-weighted HASTE images (b) show the bulging of the placenta (arrows) that invades an external layer of the bladder. Intraplacental hypointensive signal bands (newly formed vessels) are clearly seen (short arrows). Axial T2-weighted HASTE image (c) showing massive invasion of the right parametrium (arrows). The myometrial signal is absent in most part of the invaded area
Different studies compared the diagnostic performance of US and MRI in the diagnosis of PAD. One study retrospectively compared transvaginal US and MRI in 39 patients with abnormal placentation and showed 77 % sensitivity, 96 % specificity, 65 % PPV, and 98 % NPV for US and 88 % sensitivity, 100 % specificity, 100 % PPV, and 82 % NPV for MRI [8].
Another study with 13 patients showed comparable low sensitivities of US and MRI for the diagnosis of PAD (33 % and to 38 %, respectively) [9]. A multi-institutional study retrospectively evaluated 15 patients with confirmed abnormal placentation at delivery who had undergone both transabdominal sonography and MRI. Sonography had 93 % sensitivity, 71 % specificity, 74 % PPV, and 92 % NPV, whereas MRI had 80 % sensitivity, 65 % specificity, 67 % PPV, and 79 % NPV, an unremarkable difference [10].
A recent meta-analysis reviewed 18 studies involving 1010 pregnancies at risk for invasive placentation and found no difference in the sensitivity (P = 0.24) or specificity (P = 0.91) of US and MRI for the detection of PAD; however, based on the results of a single study included in the analysis, the authors suggested that MRI should always be considered to better assess both the depth and the topography of PAD [11].
In a report of 12 cases of PAD, MRI correctly gauged the depth of invasion in 3 cases underestimated by US; moreover, with reference to a standardized topographic classification that divides PADs into S1-PAD and S2-PAD (located anteriorly and posteriorly, respectively, to a plane perpendicular to the center of the so-called upper bladder axis), MRI correctly identified 3 cases of S2-PADs that were incorrectly scored as S1-PADs by US [12]. This result has great clinical implications; indeed, while S1-PADs are easily accessed during cesarean section with quick achievement of hemostasis, S2-PADs, being irrigated by deeply located vessels, often result in a massive hemorrhage that requires a complex surgical approach [13]. The MRI excellent characterization of PAD extension and invasiveness was confirmed by another report that specifically acknowledged the usefulness of these findings in the surgical planning of patients with PAD [14]. Overall, since MRI is superior to US in evaluating both the sector and the level of placental invasion, many authors propose its routine use for the implementation of the diagnostic algorithm after an US assigned diagnosis of PAD [15–17].
1.2 Placental Abruption
Placental abruption is the leading cause of vaginal bleeding in the third trimester of pregnancy, occurring in approximately 1 % of births, and accounts for up to 25 % of perinatal deaths; it originates from a premature separation of the placenta from the uterine wall and leads to the formation of retroplacental, subchorionic, or subamniotic hematomas [18]. US findings of placental abruption refer to the evidence of the hematomas but show an extremely poor diagnostic sensitiveness, with 25–50 % of false negatives; different reasons that concur to this poor performance include the similarity of the echotexture of a recent hemorrhage to that of the adjacent placenta and the small dimensions of some hematomas that spontaneously drain through the cervix [19–22].
MRI can dramatically improve the diagnosis of placental abruption. Diffusion- and T1-weighted sequences correctly identified 19 (100 %) and 18 (95 %) of 19 abruptions, with an extremely good interobserver agreement (k = 0.949) [23]. In this report, T1- and T2-weighted sequences were both required for complete tissue characterization. DWI accuracy in the detection of placental abruption was interpreted with reference to its sensitiveness to the susceptibility effects induced by the presence of blood breakdown products [24, 25], while the use of T2-weighted half-Fourier RARE and true FISP was substantiated by the coexisting presence, in cases of abruption, of acute/subacute bleeding and chronic ischemia [26].
The contemporary evaluation of T1-weighted, T2-weighted, and DWI images allowed the classification of hematomas as hyperacute (first few hours, intracellular oxyhemoglobin), acute (1–3 days, intracellular deoxyhemoglobin), early subacute (3–7 days, intracellular methemoglobin), and late subacute (14 days, extracellular methemoglobin) according to the paramagnetic effects of methemoglobin (Fig. 1.2). While the presence of a hematoma with hyperacute or acute MRI signal intensity characteristics anticipated the progression of the abruption to higher grades with the possible onset of fetal distress or maternal decompensation, the evidence of late subacute bleeding was reassuring since all these hematomas remained clinically stable over time. Therefore, MRI characterization of the hematoma structure can be of great utility for patient management as it represents a powerful instrument to portend a bad clinical outcome (Fig. 1.3).
Fig. 1.2
Placental abruption in a 35-year-old woman at 32 weeks of gestational age presenting with history of vaginal bleeding and unremarkable US findings. Sagittal gradient echo T1-weighted image (a) shows a marginal anterior hematoma (long arrows) with blood extending into the cervix; the hematoma appears hyperintense with respect to the placenta (short arrow). Sagittal DWI image (b) shows the markedly hyperintense anterior hematoma (long arrows) and a hypointense hemorrhage (short arrow) along the posterior uterine surface. On sagittal axial true FISP (c), the anterior hematoma signal intensity (long arrow) is similar to that of the placenta, while the posterior blood collection is hypointense (short arrow). Therefore, the different MR sequences are complementary and are all useful for a complete characterization of existing hemorrhage
Fig. 1.3
Placental chorioangioma in patient at 24 weeks of gestational age and profuse vaginal bleeding. Coronal (a) and axial (b) T2-weighted HASTE and axial true FISP (c) images show an intrauterine mass peripherally located and protruding from the fetal surface of the placenta. Note the posterior hypointense subamniotic hematoma (short arrows). Axial T1-weighted fat-saturated (d) sequence shows the subamniotic hematoma (short arrows)
1.3 MRI in the Management of Twin-To-Twin Transfusion Syndrome
Twin-to-twin-transfusion syndrome (TTTS) results from a hemodynamical imbalance of placental vascular anastomosis connecting the circulation of the two fetuses. Demise of a co-twin in a monochorionic pregnancy places the surviving twin at significant risk of death or neurologic sequelae due to severe intracranial hypoperfusion [27–29]. Fetal MRI is being increasingly used to identify fetal brain abnormalities [30] and is more sensitive than US in detecting ischemic injury and therefore may have a great theoretical role in the context of TTTS.
In a series of 21 cases of TTTS complicated by the demise of one twin, intracranial abnormalities including polymicrogyria, germinolytic cysts, intracranial hemorrhage, ventriculomegaly, and delayed sulcation were evidenced in seven cases by antenatal MRI; notably, in four of these seven cases, US did not score any brain abnormality, while in two of the remaining three cases, MRI showed additional findings with respect to US [31]. In another study on 68 TTTS with single-twin demise, nine fetuses presented brain abnormalities at MRI (13 %); expert US and MRI findings agreed in only three out of nine cases, while in the other six US underestimated or missed the brain alterations; in this latter study, the diagnostic advantage of MRI was mainly attributed to its capability to image the presence of “reparative” polymicrogyria, a specific abnormality that results from abnormal neuronal migration and cortical organization [32]. Of note, in the two abovementioned studies, MRI examinations were performed only a few days after the US examination; this limits any possible bias related to the evolutive nature of these lesions and supports the proposition that fetal brain pathology in TTTS is genuinely better imaged by MRI.
An early diagnosis of cerebral involvement can greatly influence the consultation and management of the affected pregnancy when fetal death occurs shortly before delivery or after laser coagulation of placental anastomosis that are typically performed at 22–24 weeks of gestation; in this latter case, any brain abnormality would become evident by sonography or conventional MRI at least 2 weeks from the death of the co-twin, greatly limiting the choice for the termination of pregnancy due to the viability of the surviving fetus. The problem of an early diagnosis of ischemic brain damage in TTTS can be conveniently addressed by including DWI sequences in the MRI protocol. In a prospective cohort study, 34 TTTS with single fetal death were evaluated by fetal sonography, conventional MRI, and DWI between 1 and 6 days after the death of the co-twin. Overall, DWI evidenced the presence of cerebral abnormalities in nine cases with unremarkable neurosonographic findings; six of these cases were scored as normal when using conventional MRI [33].
MRI can grant significant information when tailored to image the brain of the recipient twin even before the death of the donor. Two cases of intraventricular hemorrhage and brain ischemia of the recipient twin were found in a series of 25 pregnancies complicated by TTTS; fetal US imaging, performed within 2 h from MRI, was negative in both cases. In the first case, the donor twin died within a week after imaging and ischemia likely developed as a result of inter-twin anastomosis and hypotension; the evidence of ischemia/hemorrhage in the second recipient twin was associated with the enlargement of the cerebral venous sinuses and the reversal of the a wave in the ductus venosus supporting the causative role of a hyperdynamic cardiac decompensation in the genesis of brain injury [34].
The present gold standard for the diagnosis of TTTS is the US staging of Quintero that monitors the progressive deterioration of the donor fetus rather the intraplacental unbalanced circulatory sharing between the donor and recipient fetuses [35]. The goal of correctly addressing the early phases of the syndrome may be possibly achieved by using MRI. In one report, 17 patients with TTTS and 17 controls at a similar gestational age (25.9 ± 2.8 weeks) underwent placental MRI and expert US examination; an accelerated maturation of some sectors of the placenta, putatively triggered by reduced oxygen extraction, increased pO2 and speeded villi maturation was unrecorded by US but clearly evident on T2-weighted images [36].
1.4 MRI in the Prediction and Diagnosis of Uterine Rupture
The overall rate of cesarean section (CS) has dramatically increased in developed countries over the last decade [37]. The WHO Global Survey on Maternal and Perinatal Health advocates a trial of vaginal birth after cesarean section (VBAC) [38] despite acknowledging an increased risk of uterine rupture [39].
Uterine dehiscence refers to separation of the uterine musculature without extravasation of intra-amniotic contents, whereas uterine rupture refers to a defect in the uterine musculature with extravasation of fetal parts and intra-amniotic contents into the peritoneal cavity. The risk of uterine dehiscence/rupture is related to the thickness of the lower uterine segment; however, a lower uterine segment that is less than 3.5 mm thick on an US performed at 37 weeks of gestational age predicts the occurrence of uterine rupture with a positive predictive value of only 11.8 % [40]. Different US cutoff values and measurement techniques were reviewed in a recent publication [41].
A precise evaluation of the uterine scar thickness and of the myometrial fibers organization might create an objective tool to reasonably select those pregnancies that can safely undergo a trial of VBAC. MRI with diffusion tensor imaging (MR-DTI) and fiber tracking reconstruction is a novel noninvasive imaging technique that was used to characterize tissue morphology and can highlight the fiber architecture of the uterus [42].
The ability of US and 3T MR-DTI with fiber tracking reconstruction to assess the uterine scar was compared in a group of in 24 patients with a history of one or two previous cesarean sections: scar morphology, subjectively classified as either “linear” or “retracting,” was found discordant between US and MRI 13 cases (54.1 %); the thickness of the myometrium upstream of the scar was significantly greater when measured by 3T-MR rather than US in women with linear scar morphology; and the disruption of uterine muscular structure was greater in patients with retracting scars independently from the number of previous cesareans. These results anticipate a possible great role of MRI in predicting the risk of uterine rupture during VBAC and seem to support the obstetric guidelines that state that VBAC can be attempted independently from the number of previous CS [43].
MRI allows a clear visualization of the uterine wall; therefore, it helps to diagnose antepartum uterine rupture in patients with indeterminate US evidence, alternatively showing the tear itself [44] or other uterine wall defects including uterine dehiscence and uterine sacculation [45] (Fig. 1.4).
Fig. 1.4
A 34-year-old woman, primipara with a history of previous myomectomies, was admitted at 26 weeks of gestation presenting with vomiting, acute abdominal pain, and tenderness in the upper quadrants. Axial T2-weighted HASTE (a, b) and T1-weighted fat-saturated GRE (c) sequences showed a posterior uterine rupture (arrows) with extravasation of amniotic sac in the peritoneum. Note hemoperitoneum (short arrows in b and c). Emergency laparotomy showed an irregular uterine rupture with 3 cm bleeding
1.5 MRI in the Study of Chronic Placental Insufficiency
MRI does not only highlight the morphologic alterations of the placenta but also offers a noninvasive tool to obtain a quantitative evaluation of the intraplacental circulation during the course of various placental bed disorders, including intrauterine growth restriction (IUGR) and preeclampsia (PIH) definitively inproving the informations granted by the Doppler interrogation of the uterine arteries.
The first pass of an MRI contrast agent through the placenta was first reported in pregnant patients who underwent MRI for non-obstetrical indications and described as fast and homogeneously diffuse throughout the parenchyma [46]. MRI requested for potentially serious indications provided a unique opportunity to characterize in vivo the uteroplacental blood flow in IUGR placentas and to correlate the intervillous circulation to the progressive deterioration of fetal condition [47]. In this study, IUGR placentas displayed many patchy unperfused areas, a slow intervillous circulation, and multiple intermittent stops indicating that dynamic phenomena (vasospasm) are major contributors to the deterioration of placental perfusion; these results are in good agreement with the notion that the spiral arteries are variably occluded in IUGR [48, 49] and that the different placenta sectors do not share a common circulation [50].
MRI evaluation of placental perfusion with contrast agents cannot be routinely employed since the clearance rate of gadolinium from the amniotic compartment has not been yet established. However, the increased availability of a larger repertoire of in vivo placental MRI acquisitions is beginning to offer unparalleled access to in utero placental micro- and macrostructure, metabolism, perfusion, and function [51].
Three-dimensional (3D) volumetric placenta MRI data appear more reliable than those provided by 3D US [52]. Using quantitative 3D volumetric MRI evaluation, one study demonstrated that placental volumetric growth increases exponentially between 17 and 38 weeks in normal pregnancies and that a small placental volume, when recorded in high-risk pregnancies, anticipates the occurrence of IUGR [53].
Diffusion-weighted magnetic resonance imaging (DWI) underscores the differences of water molecule diffusion in human tissues and can provide valuable information on perfusion abnormalities in the human placenta. Indeed, while a feasibility study could not effectively monitor the process of placental maturation by generated apparent diffusion coefficient (ADC) maps [54], another report interpreted the reduction in the ADC of IUGR placentas with reference to the presence of many hematomas and infarctions in tissue degeneration and scarring (Fig. 1.5) [55]. In another study, the addition of DWI analysis of the placenta to the evaluation of the uterine arteries by standard Doppler analysis improved the sensitivity to predict IUGR from 73 to 100 % with a maintained specificity of 99 % [56]. Intravoxel incoherent motion (IVIM) was used to calculate the placenta perfusion fraction in 19 controls in 13 cases of early PIH and 8 cases of late PIH; in these latter two groups placental perfusion fraction was, respectively, smaller and larger than that of controls at the same gestational age, suggesting a distinct pathophysiology of the two forms [57].
Fig. 1.5
A 34-year-old woman at 33 weeks of GA with IUGR fetus. (a) ADC map shows low signal intensity areas (arrows), and this corresponds to the areas of high signal intensity seen on diffusion image (b) (B = 800 s/mm2). Arterial spin labeling perfusion map (c) of the placenta shows multiple areas (blue) of reduction of the perfusion (the normal areas are in green and red). Findings from histopathologic examination of specimens from the placenta were consistent with ischemic endovasculitis
In another study, IVIM confirmed a significantly reduced placental blood flow in IUGR compared to controls [58]. A recent prospective MRI study compared controls to women at risk for PIH but with normal Doppler of the uterine artery who were followed up to delivery; in all pregnancies that delivered IUGR fetuses, placental perfusion fraction was significantly decreased, regardless of the estimated fetal weight at the time of MRI examination [59].
Diffusion tensor imaging (DTI) measures the restricted diffusion of water and produces cellular tract images. Maximum diffusivity, mean diffusivity, and fractional anisotropy are calculated and represent membrane density, cellularity, and microstructural integrity. A single study used this technique and suggested an altered microstructure of the IUGR placenta [60].
Flow-sensitive alternating inversion recovery (FAIR) imaging is used to measure the perfusion of a target organ, by applying a pulse sequence to a vascular network with unidirectional blood flow. The multidirectional blood flow of the placenta challenges the classic paradigm of FAIR imaging and limits the interpretation of classic perfusion measurements [61]. To date, only two studies have explored the use of in vivo FAIR imaging in the evaluation of placental perfusion with discordant results [59, 62].
The paramagnetic properties of oxygen can be used to study oxygenated and deoxygenated blood using oxygen-enhanced MRI (OE-MRI) and blood oxygen level-dependent (BOLD) imaging. One study attempted to decipher if maternal hyperoxia can result in detectable changes in placental oxygenation using OE-MRI and BOLD techniques and showed that in healthy uncomplicated pregnancies, the administration of supplemental oxygen to the mothers is associated with a significant increase in the placenta OE-MRI signal, i.e., to an increased tissue oxygenation [63].
Additional reports used BOLD MRI in healthy pregnancies to investigate the putative effects of placental hyperoxia on the fetal brain; in these studies, placental hyperoxygenation was not paralleled by changes in the oxygenation state of fetal brain, suggesting that oxygen extraction remains constant over wide variations of oxygen delivery as a result of a mechanism that protects the brain of healthy fetuses from the detrimental effects of hyperoxia [64, 65].
Magnetic resonance spectroscopy (MRS) can be used to study intracellular metabolism of different organs. Most commonly, MRS uses signals from hydrogen protons (1H) to determine the relative concentrations of target metabolites, but phosphorus (31P) has also been described for human tissue analysis. 31P-NMS evidenced an increased signal related to adenosine phosphodiesters in the human placenta with advancing gestational age, suggesting an increased cell membrane turnover in aging placenta [66]. Despite a wider availability, only one study explored the use of 1H-NMS in the study of human placenta reporting a low choline–lipid ratio in growth-restricted pregnancies; however, the significance of this finding was hampered by the high choline–lipid ratio that is normally present in the placenta and therefore limits a meaningful interpretation of the spectra and the possible clinical application of this technique (Figs. 1.6 and 1.7) [67].
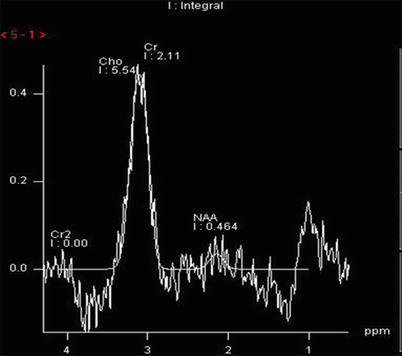
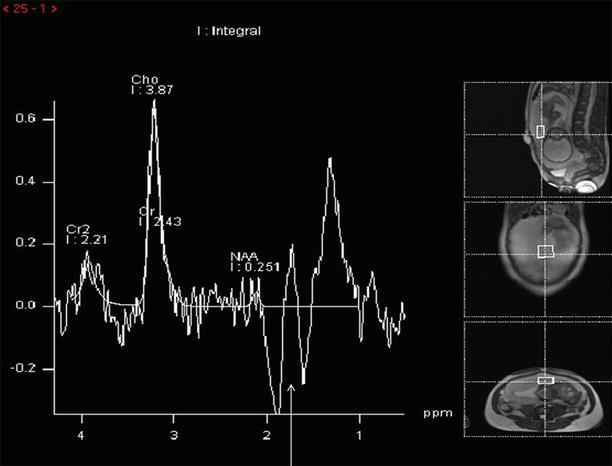
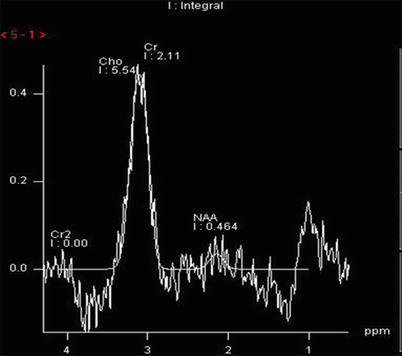
Fig. 1.6
2 × 2 × 4 cm voxel MRS acquired at 144 ms from the placenta of a healthy participant. Choline and lipid spectral peak demonstrated at frequencies of 3.21 ppm, and 1.3 ppm and 0.9 ppm per million (ppm), respectively
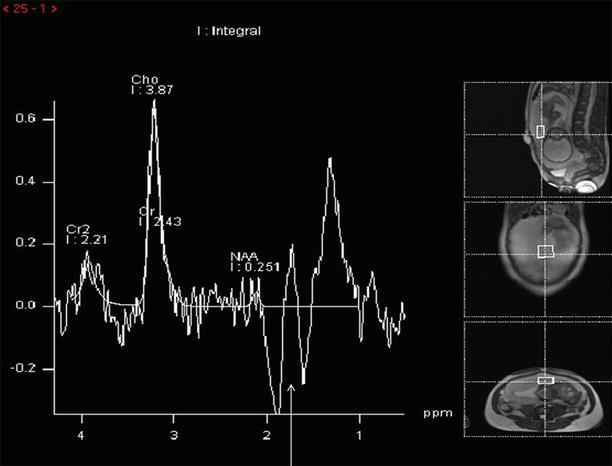
Fig. 1.7
2 × 2 × 4 cm voxel MRS acquired at 144 ms from the placenta of a patient with IUGR. In this case, lactate peak is visible as an inverted double peak at 1.32 ppm frequency (arrow). Lactate peak is produced by anaerobic metabolism
1.6 MRI in Preeclampsia/Eclampsia
Cerebral MRI is not necessary for most patients with PIH or eclampsia but can be considered in the presence of focal neurological deficits or prolonged coma; also, in cases of atypical PIH (onset before 20 weeks’ gestation or forms refractory to adequate magnesium sulfate therapy), it may improve the therapeutic planning through a better definition of the pathophysiology of the ongoing disorder. Hypertensive encephalopathy, occurring when high perfusion pressure exceeds cerebral blood flow autoregulation resulting in vasodilatation and brain edema, is considered as the model of central nervous system (CNS) perfusion abnormalities during PIH. In this regard, in a series of 9 normotensive controls and 12 untreated women with PIH, velocity-encoded phase contrast MRI of the middle and posterior cerebral arteries showed an increased cerebral artery blood flow in the affected pregnancies [68]. However, hypertensive encephalopathy does not represent the only possible pathophysiological derangement of cerebral circulation in PIH. Reversible posterior leukoencephalopathy syndrome (RPLS) is associated with PIH/eclampsia and clinically overlaps the classical picture of hypertensive encephalopathy (headache, altered mental functioning, seizures, and loss of vision) [69]. MRI of PRES demonstrates the presence of a symmetric edema that is prevalent in the hypoperfused junctional zones between the territories of the lateral and medial cerebral arteries and is generated by a hyperreactive cerebral vasoconstriction triggered by endothelial toxicity [70]. Indeed, many cases of PRES occur with minor increases of blood pressure, and the extent of brain edema does not correlate to the severity of hypertension [71]. The pathophysiological difference between hypertensive encephalopathy and PRES can be documented by MRI and have great clinical implications with reference to the use of magnesium sulfate, a commonly used drug for the treatment of PIH; indeed magnesium may be alternatively beneficial or detrimental according to the prevalence of cerebral vasodilatation or vasoconstriction since it is a potent vasodilator used in human to ameliorate the cerebral vasoconstriction triggered by a subarachnoid hemorrhage [71].
1.7 MRI in Clinical Pelvimetry and Prediction of Dystocia
MRI pelvimetry may represent a suitable approach in some rare circumstances that include patients that have either the fetus in breech presentation or a history of previous pelvic trauma but want to undergo a trial of labor [72]. One study evaluated eight singleton diabetic pregnant mothers who underwent MRI; a significant correlation was found between the MRI measurements obtained with different sequences and the actual shoulder diameter, with true FISP being the most accurate [73].
1.8 Cervical Incompetence and Prediction of Preterm Labor
Cervical incompetence, i.e., premature shortening of the cervix in the absence of uterine contractions, is due to the occurrence of premature cervical softening, a process that reduces cervical compliance through a disarrangement of collagen fibrils and an increased tissue hydration. The greatest obstetrical challenge of a sonographic short cervix consists in its poor anticipation of a forthcoming delivery, i.e., parturition within 7 days.
Cervical ripening, the cervical counterpart of active labor, is an accelerated process, totally independent from the slowly progressive shortening of the cervix, that occurs shortly before birth and is marked by an increased water permeability of cervical epithelia along with focal periglandular dissolution of the cervical connective tissue.
High ADC map intensity values in the subglandular area of the uterine cervix are significantly associated with the occurrence of delivery within 7 days (unpublished results). If confirmed in subsequent studies, this information will be of great clinical value when managing asymptomatic patients presenting at a critical gestational age with a sonographic short cervix.
1.9 MRI in the Evaluation of Maternal Acute Abdomen
A wide variety of diseases may present with acute abdominal pain during pregnancy and present diagnostic and therapeutic challenges. The diagnosis is often confounded by several common features of normal pregnancy including nonspecific pain, nausea, and vomiting and by the displacement of abdominal and pelvic structures that hampers the clinical examination. Moreover, leukocytosis is a normal finding in pregnancy and levels of C-reactive protein are higher than in nonpregnant women. Prompt diagnosis and treatment are essential for maternal and fetal well-being, and imaging is commonly requested to clarify the clinical picture and expedite diagnosis.
Given the established risks to the fetus from radiation exposure, only US and MRI are routinely considered for the diagnostic evaluation of the abdomen during pregnancy. In this regard, an increasing number of studies have substantiated the use of MRI as the technique of choice in the evaluation of pregnant patients with acute abdominal pain (Figs. 1.8 and 1.9).
Fig. 1.8
Obstruction in a 38-year-old woman at 30 weeks of gestational age presenting with acute abdominal pain and vomiting. Coronal (a) and axial (b) T2-weighted HASTE images show persistent focal transition point “beak sign” (arrows), indicative of proximal obstruction. These findings are suggestive of an adhesion, the presence of which was confirmed at laparoscopy
Fig. 1.9
Coronal T2-weighted HASTE MR image (a) shows a complex mass with fluid and solid components on the left ovary (borderline tumor) (arrows). Note low hyposignal into the right lateral ventricle (arrow), better seen on sagittal T2-weighted MR (b); axial T1-weighted sequence (c) shows hyperintense signal at the level of the right lateral ventricle, indicative of intraventricular hemorrhage. Axial T1-weighted MR image (d), performed in the newborn 10 days after birth, demonstrates a germinal matrix hemorrhage extended to the right ventricular system (arrow)
Acute appendicitis is the most common non-obstetrical surgical condition of the abdomen during pregnancy; it is often associated with perforation due to delayed diagnosis (43 % vs. 4–19 % in the general population) and to a significant fetal loss of (20–25 %). These data emphasize the need for accurate early diagnosis and timely surgical intervention [74–76]. Ultrasonography with graded compression is scarcely valuable for detecting acute appendicitis in pregnant women due to the infrequent visualization of the appendix; in one report, US detected the appendix in only 29 % of surgically proven cases occurring during the second and third trimesters of pregnancy [77]; in another study, US sensitivity and specificity to diagnose acute appendicitis during pregnancy were 78 % and 83 %, respectively [78].
MRI can dramatically improve the diagnosis of appendicitis [79] with a visualization rate of the appendix as high as 70 % and an extremely high specificity [80].
The overall sensitivity, specificity, positive predictive value, and negative predictive value of MRI for the diagnosis of acute appendicitis ranged from 90 to 100 %, 93 to 98 %, 61 to 82 %, and 99 to 100 %, respectively [81, 82].
This diagnostic performance was recently confirmed in a retrospective study from a university tertiary referral center [83].
Bowel obstruction in pregnancy is fairly uncommon (1 per 2,500 to 1 per 3,500 pregnancies), normally results from the mechanical effects exerted on the bowel by the enlarging gravid uterus or from the presence of adhesions, and is poorly characterized by US [74]. Magnetic resonance studies for bowel obstruction, particularly if performed with the use of multiplanar T2-weighted single-shot fast spin-echo (SSFSE) imaging can accurately depict the site of small bowel obstruction in up to 70 % of cases [84, 85] (Fig. 1.8).
Magnetic resonance enterography (MRE) is extremely valuable in the diagnostic evaluation for Crohn’s disease (CD) with reported sensitivity and specificity being 83–91 % and 86–100 %, respectively, in the presence of a bowel wall thickness greater than 3 mm and of increased signal intensity on T2-weighted images [86]; these evidences were particularly useful in the evaluation of the active state of CD in a group of 9 pregnant patients [87]. These results are particularly significant because up to one-third of women with inflammatory bowel disease (IBD) relapse during pregnancy as a consequence of a voluntary cessation or tapering of therapy, usually triggered by the fear of putative but undemonstrated teratogenic effects.
The assessment of the extent and severity of acute severe colitis and the identification of toxic dilatation of the colon are more challenging during pregnancy due to the preferential avoidance of ionizing radiation. Magnetic resonance colonography (MRC) performed in a pregnant patient according to a protocol that included multiplanar T1- and T2-weighted sequences and diffusion-weighted imaging (DWI) following intravenous (IV) administration of antispastics clearly evidenced the hallmarks of active ulcerative colitis (circumferential thickening together with a marked restricted diffusion in the involved segment of the colon) [88].
Symptomatic biliary tract disease in pregnancy is uncommon, despite the high prevalence of gallstones in pregnancy. Magnetic resonance cholangiopancreatography (MRCP) clearly evidenced the obstructive etiology in four out of eight pregnant patients with an undetermined biliary dilatation detected by US and was proposed as the most appropriate second-line imaging test to fully evaluate biliary dilatation during pregnancy [89].
Pregnancy-induced hepatic morbidity is rare and is usually seen in two forms: hepatic necrosis associated with the hemolysis, elevated liver enzymes, and low platelet count syndrome (HELLP) and acute fatty liver of pregnancy (AFLP). Hepatic involvement in HELLP syndrome is initiated by intravascular fibrin deposition (leading to sinusoidal obstruction) and hypovolemia, leading to hepatic ischemia/infarction and hemorrhage. The initial diagnosis of HELLP syndrome is usually made using a combination of biochemical criteria and clinical findings (right upper abdominal pain); urgent MRI can be performed to corroborate the diagnosis of HELLP by showing the presence of liver ischemia [90] or alternatively to evaluate the possible occurrence of a hematoma beneath Glisson’s capsule [91].
AFLP is initiated by a hampered intramitochondrial fatty acid oxidation leading to severe microvesicle steatosis and acute liver dysfunction. MRI performed with T1-weighted dual gradient-echo in-phase (IP) and out-of-phase (OOP) sequences is confirmatory of the diagnosis as it depicts a dramatic loss of hepatic signal intensity in OOP images [92].
Women with sickle cell disease who become pregnant are at increased risk for developing PIH and eclampsia [93]. Liver MRI in cases of sickle cell disease shows a low signal on T2*-weighted sequences: in the proper clinical setting, subtle increases of the T2 signal in the hepatic parenchyma can allow a presumptive diagnosis of end-organ ischemia and early preeclampsia [90].
Urolithiasis and urinary tract infection are the most common causes of abdominopelvic pain in pregnancy, and urolithiasis is the most common non-obstetric indication for hospitalization.
Ultrasound, despite its poor diagnostic performance, is the first imaging test for suspected urolithiasis in pregnancy; false negatives due to obstruction without dilatation are rare, but false positives are common because a physiological dilatation of the collecting system occurs in pregnancy [94]. Magnetic resonance urography (MRU) can rapidly acquire images of the upper urinary tract without the administration of intravenous contrast agents and is a valuable examination in pregnancy. In a series of 24 pregnant patients with symptomatic hydronephrosis, MRU clearly differentiated physiological urinary tract dilatation from abnormal dilatation related to urolithiasis by showing different indirect signs including renal enlargement, perirenal fluid collection, signal voids overlying the high signal of urine within a dilated ureter, the presence of a standing column of urine below the level of the pelvic brim, and an abrupt ending of the ureter [95]. MRU accuracy in detecting small ureteral calculi may be further improved by the use of thin-slice, high-resolution SSFSE with a positive predictive value of 80 % [96]. Finally, MRU can effectively score complications such as diffuse or focal pyelonephritis (visualized at as an enlarged edematous kidney or areas of lower signal intensity on T2-weighted images and restricted proton diffusion on the DWI, respectively) [97].
1.10 MRI to Improve Imaging of Fetal Structural Abnormalities
MRI can be extremely useful in the recognition of the developing fetal anatomy, detection of subtle fetal abnormalities, and evaluation of complex lesions.
The development of fetal MRI techniques predictably led to comparisons between the accuracies of MRI and US. A review consisting of 13 published studies comparing anomaly detection rate of US compared to MRI found that fetal MRI provided additional anatomical information in up to 45.3 % of the cases [98]. Many of these earlier studies presented significant bias because US was not usually performed in expert centers, their results were known to the radiologist and used in MRI interpretation, and significant intervals often elapsed between ultrasound and MRI (potentially allowing sufficient time for lesions evolution toward more identifiable forms). However, a number of recent prospective studies directly compared US and MRI and confirmed that this latter technique has a greater detection rate for many fetal anomalies [99, 100].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree