Chapter 40 Complications in the Oncologic Patient
Abdomen and Pelvis
Introduction
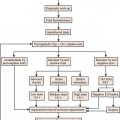
Radiation complications occur in an acute, subacute, or chronic timeframe (Table 40-1).1
Table 40-1 Radiation Effects Can Be Stratified into Specific Time Segments
| EFFECT | TIMEFRAME |
|---|---|
| Acute | <90 days |
| Early delayed | >90 days |
| Late | >90 days |
I Hepatobiliary, Spleen, and Pancreas
Liver
Chemotherapy Change
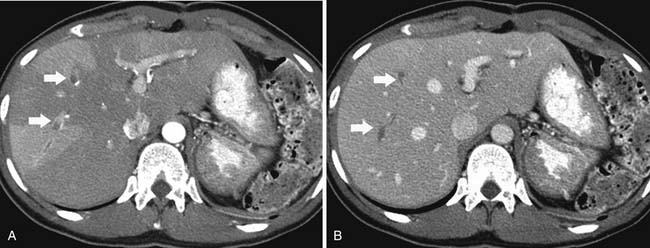
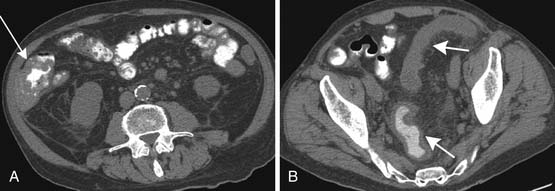
Fatty infiltration of the liver is seen with administration of all chemotherapy agents, especially irinotecan and oxaliplatin.2 It can be focal or diffuse; when diffuse, it is called chemotherapy-associated steatohepatitis. Knowing the different imaging appearances and characteristic sites can aid in differentiating between liver metastases and fatty change. Fatty infiltration can be either focal or diffuse. The focal lesions can sometimes cause difficulty in distinguishing from metastatic disease. Clues that a lesion may represent fatty infiltration are location in the falciform ligament, porta hepatis, and gallbladder fossa and a geometric, well-defined shape. Ultrasound can show a well-defined hypoechoic region. CT and MRI can be used for diagnosis. On CT, there will be a low-attenuation region (Figure 40-1). MRI with in- and out-of-phase imaging is very useful in confirming the diagnosis.2
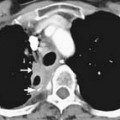
Portal vein thrombosis has also been seen with patients undergoing preoperative chemotherapy.3 Portal vein thrombosis is seen on CT as a filling defect within the portal vein. On ultrasound, there is echogenic thrombus within the portal vein. Branch portal vein thromboses can cause wedge-shaped areas of perfusion change, which need to be distinguished from development of metastatic disease (Figure 40-2). Treatment is conservative and consists of anticoagulation.
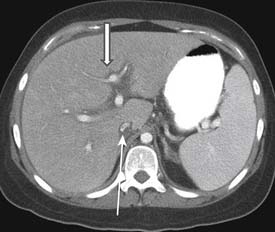
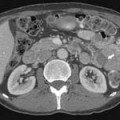
Veno-occlusive disease has been described in patients with stem cell transplants and also in patients with colorectal liver metastatic disease taking oxaliplatin.4 Clinically, the patients have hepatic failure and jaundice. CT scan shows a heterogeneous liver with narrowing of the right hepatic vein, periportal edema, and ascites5 (Figure 40-3). Ultrasound examination shows ascites; reversal of hepatic venous flow is a late sign. This can be distinguished from hepatic graft-versus-host disease (GVHD) by its early presentation in the first 20 days after stem cell transplant.6
Changes that have been observed after intra-arterial chemotherapy infusion are chemical hepatitis, gastrointestinal ulceration, sclerosing cholangitis, and biliary cirrhosis.7
Radiation Change
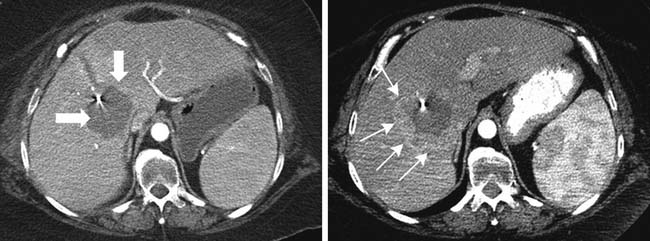
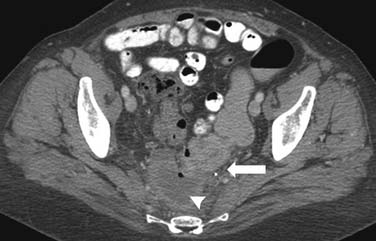
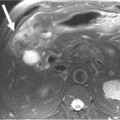
Radiation-induced liver disease (RILD) occurs in approximately 5% to 10% of people who received whole liver irradiation in doses exceeding 30 to 35 Gy.8 Patients usually present 2 to 8 weeks (up to 4 months) after radiation exposure with hepatomegaly, ascites, and elevated liver enzymes.9 Pathologically, there is a picture of veno-occlusive disease with congestion of the central portion of the lobule with sparing of the larger veins. The radiologic picture is that of a clear demarcation—also known as the straight border sign—between the area that has received radiation and that which has not been irradiated.10 This can be differentiated from vascular changes by its nongeographic distribution. In the acute and subacute phases, the area that has been irradiated is seen at CT to be lower in attenuation than the adjacent liver, likely due to edema (Figure 40-4). On MRI, the irradiated area has low T1 signal and high T2 signal due to edema. Chronic changes can occur with fibrosis and volume loss. Usually, patients have resolution of findings in 3 to 5 months, but a small portion progress to liver failure.
Surgical Change
Surgical resection is performed for patients with hepatocellular carcinoma, cholangiocarcinoma, and metastatic disease. Postoperative fluid collections that can be seen at the surgical site are abscess, postoperative seromas, and bile duct leak. At our institution, these are usually drained percutaneously. Over time, these collections and the perfusion change along the hepatic surgical margin will resolve. It is important to distinguish between postsurgical change and recurrence of tumor by reviewing the initial imaging study in the postoperative period. Over time, the remaining liver may regenerate.
Radiofrequency ablation (RFA) is being increasingly used in the treatment of colorectal metastatic disease to the liver.11 On CT and MRI, the RFA defect site is a low-density area in the place of the treated metastasis. There may be hypervascularity surrounding the surgical site initially, which usually resolves within 3 months. Tumors adjacent to the portal vein pedicle can lead to injury of the bile duct, with stricture and possible sepsis.11 It is important to diagnose recurrence, which is any change in the size of the cavity, mass effect, nodularity, and enhancement (Figure 40-5).
Spleen
Chemotherapy Change
Splenic rupture is a rare complication of stem cell transplant or treatment with granulocyte colony–stimulating factor (G-CSF). G-CSF is given to cancer patients for treatment of therapy-induced neutropenia.12 In splenic rupture, patients usually present with abdominal pain and left shoulder pain. On CT, there is irregularity of the spleen, splenomegaly, and high-density fluid surrounding the spleen and in the abdomen, consistent with hemoperitoneum. Treatment usually consists of intravenous hydration and resection of the spleen.
Surgical Change
Splenectomy is performed for lymphoma, myelodysplastic disease, or other hematologic malignancy to obtain total local control. If the spleen is also adjacent to tumors of the pancreas, retroperitoneum, peritoneum, or kidney, it may be removed as well. Occasionally, in the postsurgical bed, small splenules will develop or remain behind.
Pancreas
Chemotherapy Change
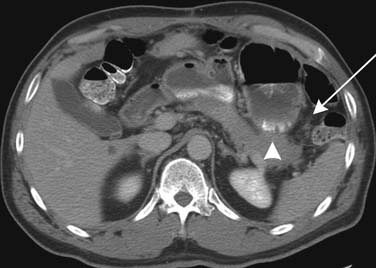
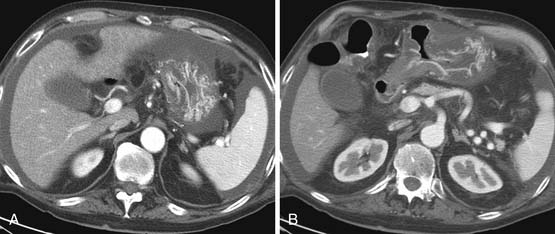
Cytoreductive surgery with intraperitoneal chemotherapy is being used more frequently in order to prolong survival in patients with gastric, ovarian, and pseudomyxoma tumors. Pancreatitis is a complication that occurs approximately 2% to 7% of the time with these procedures.13 Pancreatitis can be focal or diffuse (Figure 40-6).
Surgical Change
CT is frequently used for imaging patients who have undergone pancreaticoduodenectomy. Postoperative changes that are commonly seen are pneumobilia (particularly in the left lobe), normal jejunal loop, and postoperative fluid collections. CT is especially useful for the diagnosis of postoperative abscess, leaks, biloma, biliary obstruction, pancreatitis, and bowel obstruction.14
Key Points Liver, spleen, and pancreas
• Fatty change of liver due to chemotherapy can be diffuse or focal. MRI or ultrasound can be helpful in confirming this diagnosis.
• Radiation change can cause a characteristic appearance in the liver and should not be mistaken for recurrent tumor.
• Enlargement of the spleen can occur with chemotherapeutic agents, and monitoring for portal hypertension should be done.
• Recurrent pancreatic tumor can be distinguished from radiation change with biopsy.
II Digestive System
Chemotherapy Change
Chemotherapeutic agents cause immunosuppression, which can lead to the bowel complications of Clostridium difficile infection, colitis, and typhlitis. C. difficile infection and colitis can present with a spectrum of findings ranging from diarrhea to pseudomembranous colitis to fulminant colitis. Stool culture or endoscopy is used for diagnosis. CT may be helpful, and there is diffuse thickening of the colon on imaging. Treatment is antibiotic therapy with metronidazole or vancomycin.15
Typhlitis or neutropenic colitis can be seen in children and adults being treated for hematologic malignancies or undergoing immunosuppressive therapies. On CT, typhlitis is seen most commonly as bowel wall thickening greater than 3 mm and inflammation of the terminal ileum and cecum, but it can be seen in the entire bowel. Pneumatosis and fluid/abscess can also be seen. Ultrasound may also be a useful imaging tool. Imaging is also helpful in excluding other etiologies of pain such as appendicitis, other forms of colitis, or obstruction.16 Treatment is supportive and consists of intravenous fluids, antibiotics, and if necessary, G-CSF or surgery for bleeding.
Acute GVHD occurs within the first 100 days after transplant, and chronic GVHD occurs within 100 days after transplant. Acute GVHD clinically presents with cramping and diarrhea, which can be bloody. The diagnosis is usually made by endoscopy, but it can be seen on CT as bowel wall thickening (Figure 40-7). Chronic GVHD affects the small bowel and colon less commonly than acute GVHD. Patients can have malabsorption, sclerosis of the intestine, and fibrosis.15
Targeted therapies are increasingly being used for treatment of many cancers. These drugs target the cell receptors, and examples include vascular endothelial growth factors, epithelial growth factors and platelet-derived growth factors. They affect the blood supply adjacent to the tumor and may have a system-wide thrombogenic effect. Perforation and fistulas are complications of treatment with anti-vascular epithelial growth factor (VEGF) agents17 (Figure 40-8).
Radiation Change
Esophagus
Radiation effects on the esophagus occur at doses greater than 45 Gy and can last weeks to months. The earliest sign is abnormal motility, which can be observed at barium examination. Mucosal edema and fistula may occur within the first month after therapy. Strictures can also be seen as smooth narrowing with margins that are tapered.18 At CT, inflammatory change is seen as enhancement in a central ring. On PET/CT, esophageal radiation change can be FDG-avid and can sometimes be difficult to distinguish from residual tumor and radiation change.19
Stomach and Duodenum
Radiation injury to the stomach and duodenum can occur as a result of therapy directly to these organs or owing to irradiation for tumors of the pancreas. Effects can happen after radiation of 50 Gy, and the fixed position of the duodenum and stomach contributes to the susceptibility to injury.20 Diffuse inflammatory change, ulcers that do not heal, fixed narrowing, and deformity are all seen with radiation injury. CT may show wall thickening and perigastric or periduodenal fluid (Figure 40-9).