Protocol Management and Optimization
Protocols are the turn-by-turn instructions that allow the computed tomography (CT) operator to get from point A—registering the patient on the scanner from the order in the radiology information system (RIS)—to point B—sending a complete set of images to the picture archiving and communication system (PACS) for a radiologist to interpret. To comply with the National Electrical Manufacturers Association (NEMA) XR-29 standard, all CT systems must be equipped with a set of reference adult and pediatric scan protocols. Although these default protocols are typically very reasonable for clinical use, many practices prefer to customize scanning protocols to best match radiologist preferences and scanning workflows.
The term protocol can be used in many different contexts in radiology, so it is important to take a moment and offer several refinements to the broader term. These refinements are intended to be consistent with the anticipated definitions in the forthcoming (at time of publication) Digital Imaging and Communications in Medicine (DICOM) Supplement 121 on CT Procedure Plan and Protocol Storage SOP Class. The procedure referred to in all the listed refinements is the imaging procedure that is indicated by the order placed by a physician:
Defined procedure protocol: a description of the parameters and settings for CT image acquisition and reconstruction for a requested procedure. The defined procedure protocol is not patient specific and may not even be scanner specific insofar as a defined procedure protocol may include scanning and reconstruction instructions for a variety of scanners. The defined procedure protocol is equivalent to what some institutions may call their “master protocol.”
Planned procedure protocol: contains patient-specific acquisition parameters and scan settings. The planned procedure protocol is developed by applying the defined procedure protocol to a specific patient and taking into account any patient or imaging task-specific requirements.
Performed procedure protocol: the set of imaging parameters actually used to scan the patient. The performed procedure protocol is inextricably linked with the patient the exam was performed on.
Scanner protocol: not part of the anticipated DICOM protocol SOP class, but a term useful to define. The scanner protocol is the protocol defined and named on a specific CT scanner that matches the defined procedure protocol. Scanners may have different naming conventions or requirements and different technical specifications, so not all scanner protocols may match in name or imaging parameters, but they should be within the specifications described in the matching defined procedure protocol.
Use of Protocols in an Imaging Operation
Under normal clinical operations—excluding exams ordered and performed in an emergency setting—a referring physician (primary care or specialist) orders a radiology imaging procedure for a patient. This order may be printed out at the clinic and given to patients to take to a radiology service provider of their choice. Alternatively, if the referring physician has a relationship with a radiology group or is part of a hospital or healthcare network, the order may be entered into the patient’s electronic medical record (EMR), and the radiology practice may contact the patient directly to schedule the imaging procedure. An order may appear in one of many forms. It may be as sophisticated as an electronic order entered through a radiology order entry software interface with decision support incorporated or as low tech as a faxed handwritten order with the patient’s history and indications for the exam.
The United States passed and enacted the Protecting Access to Medicare Act of 2014, which requires use of physician-developed appropriateness criteria when ordering advanced imaging exams (including CT) for full reimbursement of studies completed on patients covered by Medicare starting in 2017. The implementation and use of clinical decision support tools (including appropriateness criteria) by physicians ordering advanced imaging exams (including CT) is a key challenge hospitals and imaging centers will need to address. The goal of linking Medicare reimbursement rates to the use of appropriateness criteria is to increase adoption of decision support systems that aid clinicians in selecting the most appropriate exam for a patient’s medical history; this can reduce the instances of unnecessary or repeated scans. As shown in Figure 2-1 , clinical decision support tools can guide physicians in selecting the appropriate imaging exam when integrated with an electronic order entry system.

Defined Procedure Protocol Selection.
The order placed by the referring physician for the patient to be imaged must be translated from the order to a procedure code as defined by DICOM and eventually to a defined procedure protocol specific to the radiology service provider. This translation can be done manually or by using lookup tables that are included in a software program.
Radiology service providers maintain some sort of master procedure book that includes the practice-specific procedure code long and short names and the Current Procedural Terminology (CPT) codes associated with that procedure code. When an order comes in from a referring physician, it may or may not conform to the naming conventions of the master procedure book of the radiology practice. If the radiology practice uses, and the ordering physician has access to, an electronic order entry system, then the received order will contain the practice’s procedure code. However, if the radiology practice does not use such software or the physician does not have access to it, the requested order may not match directly with the procedure codes the practice uses. For example, a physician may order “CT Head” but the radiology practice’s long name for this procedure code may be “CT Brain Without Contrast” with a short name of “CTHDWO.” Examples of radiology orderable exams and procedure codes along with translations to a standardized nomenclature (Radlex Playbook) are presented in Table 2-1 . The Radlex Playbook is being used by the American College of Radiology (ACR) Dose Index Registry (DIR) as the common nomenclature for protocol naming for exams submitted to the registry. Using a common nomenclature and Radlex Playbook ID (RPID) facilitates comparison of dose indices for similar protocols across multiple institutions.
| Procedure Code | Procedure Name | Protocol Name | Playbook Long Name | Playbook Short Name | RPID |
|---|---|---|---|---|---|
| CTABDWO | CT ABDOMEN W/O CONTRAST | CT ABDOMEN | CT ABDOMEN WITHOUT IV CONTRAST | CT ABD WO IVCON | RPID3 |
| CTENTERO | CT ABDOMEN, PELVIS W CONTRAST | ABDOMEN AND PELVIS (ENTEROGRAPHY) | CT ABDOMEN PELVIS ENTEROGRAPHY WITH IV CONTRAST | CT ABD PELVIS ENTERO W IVCON | RPID152 |
| CTFACWO | CT MAXILLOFACIAL WO CONTRAST | SINUS/MAXILLOFACIAL | CT MAXILLOFACIAL WO IV CONTRAST | CT MAXILLOFACIAL WO | RPID34 |
| CTSINWO | CT SINUSES WO CONTRAST | SINUS/MAXILLOFACIAL | CT HEAD PARANASAL SINUSES WITHOUT IV CONTRAST | CT HEAD SINUSES WO IVCON | RPID62 |
| CTAABDRUNW | CTA ABD AORTA W BILAT ILIOFEMORAL W CONTRAST | CTA RUNOFF | CT ABDOMINAL AORTA/ILIOFEMORAL RUNOFF ANGIO W AND WO IV CONTRAST BILATERAL | CT ABD RUNOFF ANGIO W/WO BILAT | RPID5995 |
* Examples of different naming conventions for radiology procedure codes, order names, and different names for the protocols are shown. Columns 1 and 2 present the radiology orderable in both short name and long name format. Column 3 is a defined procedure protocol associated with the radiology orderable in the same row. Columns 4 and 5 are the long and short Radlex Playbook names generated by converting the protocol name to a standardized nomenclature using the Radlex Playbook. The final column is the Radlex Playbook ID (RPID) assigned to the Playbook name.
If the order was placed without the use of electronic order entry, an individual must manually review the order and determine which of the practice’s procedure codes best matches the order. This step may be done by a customer service representative, a CT operator, or a radiologist. If there is any doubt whatsoever about which procedure code best matches the order, the referring physician should be contacted to verify the correct procedure code is selected so the required exam can be completed.
Following identification of the correct radiology service provider–specific procedure code, the next step in translating the order is identification of the defined procedure protocol. Some practices may have a one-to-one correspondence between the procedure code and the defined procedure protocol. However, it is common for more advanced imaging studies to have multiple defined procedure protocols matched to a signal procedure code. Selection of the defined procedure protocol then will depend upon the indications for the exam and the patient history. For example, a physician’s order may be translated to the procedure code “CT Abdomen and Pelvis Without and With Contrast,” but the radiology practice may have multiple defined procedure protocols that can be used with that procedure code. One defined procedure protocol may require a precontrast CT of the entire abdomen and pelvis with a single delayed acquisition following injection of an iodinated contrast agent. Another defined procedure protocol matched to that procedure code may be a precontrast abdomen and pelvis study followed by a contrast injection with scans of just the abdomen at the arterial and venous and phases and a delayed abdomen and pelvis scan. Both the indications and information obtained for those two defined procedure protocols are very different, but they carry the same procedure code.
If there is not a one-to-one match between the procedure codes used by a radiology service provider and the defined procedure protocols, a radiologist must review the patient history, the indications for the exam, and the requested procedure to assign a defined procedure protocol to the patient and the procedure code. This step is typically referred to as protocoling and is an important quality assurance check to ensure that the correct protocol with the correct parameters and timing of the acquisitions are used. Additionally, for radiology service providers operating in the United States and accredited by The Joint Commission, the 2015 revision to the Diagnostic Imaging Standards requires that the facility verify that the correct protocol is used to perform CT imaging exams. One way to demonstrate compliance for exams without a one-to-one correspondence between the procedure code and defined procedure protocol is to have a radiologist “protocol” the exam by selecting the appropriate defined procedure protocol.
Preimaging Protocol Verification.
Once the order for the imaging study arrives at the radiology service provider, a number of steps must be followed after the appropriate defined procedure protocol is assigned to the imaging study. The steps that follow may not be carried out in the particular order listed, but each one should be addressed before the patient arrives to have the imaging study performed.
Prior to any of the steps, a “step zero” may occur in which a radiologist protocols the procedure requested for the patient. At this step, as described earlier, the radiologist reviews the order, patient history, indications for the exam, and appropriateness of the requested procedure and assigns a defined procedure protocol to the order. If a radiologist does not protocol the order, there is typically a lookup table of some sort that matches the requested procedure to the defined procedure protocol of the radiology service provider:
- 1.
Exam verification. The customer service representative or CT operator scheduling the exam must first verify that the practice is able to perform the requested service. For example, a physician may order a CT of the abdomen for a patient with a history of kidney stones and include in the comments for the order the request that the exam be performed using a dual-energy acquisition with postprocessing to assess the composition of the kidney stone. If the practice does not have a dual-energy CT scanner or only has it at a certain location, that information must be taken into account when scheduling the exam.
- 2.
Insurance check. The radiology service provider will typically check with the patient’s insurer(s) to see if the imaging study needs preapproval or is automatically covered.
- 3.
Scheduling. The imaging study is scheduled on the appropriate imaging modality and on a system that is able to perform the requested procedure.
- 4.
Patient preparation. Instructions are relayed to the patient on how to prepare for the exam and could include how early to arrive for the exam or whether or not eating or drinking in a certain time period before the exam is allowed.
- 5.
Patient screening. The patient may be asked questions and the patient’s medical record reviewed, depending upon the ordered exam, to ensure that performing the requested procedure is safe. Screening questions for CT exams are used to ensure that allergies or sensitivities to contrast agents are taken into account and to ensure that any medications the patient may require before the exam will be taken.
Patient Arrival and Preparation.
Many CT examinations require specific patient preparation steps before the study can proceed. Examples include consumption of contrast material or water several hours prior to an exam of the abdomen and pelvis to fill the bowels, placement of an intravenous (IV) line, or lab tests to confirm the patient is not pregnant or can tolerate the contrast agent used in the exam. Some of these preparations may require the patient to arrive at the clinic well before the scheduled scan start time or for the results of lab tests to be communicated in a timely manner to the facility performing the examination.
Once the patient is at the clinic and has gone through the necessary preparation steps, they may be asked to change out of some or all of their clothes. A key requirement is that any metal objects the patient is wearing that will be in the scan field of view (FOV) be removed if possible. Objects including necklaces, earrings, belts, and even eyeglasses should be removed and placed nearby to return to the patient after the scan. There is some debate as to whether or not removal of brassieres is required for examinations of the thorax area. Image quality and breast tissue radiation dose may be improved by keeping the brassiere on—even if it has a metal underwire—especially on scanners using organ dose modulation techniques.
An additional preparation requirement for studies using iodinated contrast agents is that the patient has a patent IV line of sufficient size to support the flow rate and pressure of the contrast injection. Alternatively, placement of an IV line can be skipped if the patient has a functioning port for the infusion of chemotherapy agents that can be used. Verification that the line used for the contrast injection is well positioned, has proper flow, and is large enough to tolerate the flow rate is key because poor placement or preparation of an IV line can result in contrast extravasation at the IV site, which can have significant negative patient outcomes.
If the exam requires use of an iodinated contrast agent, the proper concentration of iodine must be loaded into the power injector by the CT operator, and the injection protocol for the indicated exam must be entered and confirmed at the power injector interface. Many institutions prescribe different amounts of contrast and contrast injection rates based on body habitus for adults. As with radiation dose, contrast injection protocols for pediatric patients should be correctly sized, and for infants may require use of a manual injection technique.
Once the patient has gone through all the required preparation steps, including verification of the correct patient identity according to the policy and procedure at the facility performing the exam, the final preparation step of positioning the patient in the scanner may occur. The patient must either be transferred or place him/herself on the CT scan table in the correct orientation for the exam. Body examinations may require the patient to be positioned feet first toward the scanner, whereas head examinations may call for a head-first orientation. Most CT scans are performed with the patient in the supine position. However, some exams may call for the patient to be prone, such as certain acquisitions for virtual colonoscopies or for high-resolution chest CTs. Positioning aids such as head holders, knee pillows, Velcro body fasteners, or breast straps may also be used to ensure patient comfort and optimal scan outcome. Additionally, if the examination calls for the patient’s arms to be above his/her head, an arm rest may be added for patient comfort and to limit movement during the exam.
For examinations of the thorax and the abdomen, moving the arms to a position above the head ensures optimal image quality and radiation dose utilization. Some patients may not be able to move one or both arms above the head, and if that is the case, reconstruction artifacts and increased radiation dose should be expected. Limited patient arm movement may also affect proper vertical centering of the patient. For example, if the patient is only able to raise his or her arms so that the elbows are bent next to the ears, the table height may be limited because the elbows may touch the top of the gantry.
Once positioned properly, the patient table is advanced toward the CT gantry, and laser lights to aid in the centering of the patient are turned on ( Fig. 2-2 ). Correct vertical centering of the patient is vital to ensure that the anatomy of interest is as close to the scanner isocenter as possible. There are two main reasons proper vertical centering is key. The first is that by keeping the anatomy of interest as close to the isocenter as possible, the reconstructed FOV can be kept as small as possible. This will ensure that the best possible in-plane spatial resolution is achieved. The second is that proper vertical centering is vital for the automatic exposure control (AEC) system of the CT scanner to work properly.

Care must be taken to ensure that the patient is well centered laterally with respect to the gantry isocenter. The patient’s midline should be as close as possible to the middle of the scanner, because a patient mispositioned to the right or left of center will also interfere with the optimal functioning of the AEC. Mispositioning in this direction may also result in some anatomy at the extreme sides of the body not being included in the reconstructed image sets. The most extreme impact of lateral mispositioning is introduction of truncation artifacts if portions of the patient are outside the CT scan FOV.
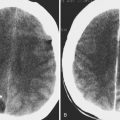
Proper functioning of the AEC is an important driver of proper patient positioning vertically and laterally. This is in part because AEC systems are designed with the assumption that the patient is well centered, and situations in which assumptions are not met in CT scanning typically lead either to nonoptimal image quality or nonoptimal radiation dose. A vertically mispositioned patient will result in a CT localizer radiograph that either magnifies (if positioned above isocenter) or shrinks (if positioned below isocenter) the apparent size of the patient (assuming the tube is positioned above the patient for the localizer radiograph; the resulting magnification/minification scenarios are reversed if the tube is below the patient). Figure 2-3 shows an example of the change in apparent size of a patient due to vertical mispositioning. Many CT scanners use the size of the patient as determined by the CT localizer radiograph to inform the operation of the AEC system. If the patient is positioned below isocenter, the AEC system may adjust the planned radiation dose to fit the smaller apparent patient size of the localizer radiograph instead of matching the dose to the actual patient size. The result of this vertical centering error can be an increase in image of noise of 20% for a positioning error of 6 cm. A clinical example of the result of a patient positioned too low in the gantry is shown in Figure 2-4 . Positioning the patient above isocenter can lead to significant increases in patient radiation dose because the AEC system may adjust the dose modulation pan to fit the larger apparent size of the patient from the radiograph. Figure 2-5 presents an example of the result of a phantom purposely positioned too high in the gantry; the radiation dose used for the scans increased by 50% when the phantom was positioned above the gantry isocenter.