Fig. 4.1
Transverse ultrasound image of the normal spermatic cord. Echogenic cord contents are seen between calipers
Normally, a few millilitres of fluid are present within the layers of the tunica vaginalis, which may function as a lubricant and should not be considered abnormal.
Swelling of the cord is the most frequent finding of funiculitis on ultrasound (Fig. 4.2).


Fig. 4.2
An enlarged hyperechoic cord due to edema is seen between calipers in a patient with funiculitis
Color Doppler ultrasound demonstrates increased vascularity.
Varicocele
A varicocele is an abnormal dilatation of the veins of the spermatic cord and is usually caused by incompetent valves in the internal spermatic vein.
Varicoceles can be broadly classified as primary or secondary and extratesticular or intratesticular.
Primary Varicoceles (Idiopathic)
Primary or idiopathic varicoceles are present in approximately 15 % of adult men. Patients with idiopathic varicoceles usually present between the ages of 15 and 25 years. Approximately one-third of men undergoing evaluation for infertility present with varicocele; however, not all patients with infertility have a palpable varicocele.
In a study of 1,372 infertile men, varicocele was found at ultrasound in 29 % of patients; of these, only 60 % had a palpable varicocele.
Secondary Varicoceles
Secondary varicoceles result from increased pressure on the spermatic vein produced by disease processes such as hydronephrosis, cirrhosis, or abdominal neoplasm (Fig. 4.3).

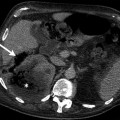
Fig. 4.3
Diffuse retroperitoneal lymphadenopathies in patient with lymphoma (a) and secondary varicocele (white arrow) (b) are demonstrated on axial contrast-enhanced CT
Neoplasm is the most likely cause of sudden onset of varicocele in men over 40 years of age; it is classically caused by a left renal malignancy invading the renal vein.
Varicoceles appear as convoluted intrascrotal masses of soft tissue density, usually located along the spermatic cord.
Extratesticular Varicocele
Diagnosis of palpable varicocele is important, because treatment improves sperm quality in as many as 53 % of the cases. The relationship between nonpalpable (subclinical) varicocele and infertility remains controversial.
Inratesticular Varicoceles
Etiology of intratesticular varicocele is unknown, but their independent existence is more common.
They may exist in association with extratesticular varicocele.
Imaging
Ultrasound
Ultrasound should be performed with the patient in both a supine and a standing position.
The ultrasound appearance of varicocele consists of multiple, hypoechoic, serpiginous, tubular structures of varying sizes larger than 2 mm in diameter that are usually best visualized superior and/or lateral to the testis. When large, a varicocele can extend posteriorly and inferiorly to the testis.
Color flow and duplex Doppler ultrasound optimized for low-flow velocities help to confirm the venous flow pattern, with phasic variation and retrograde filling during a Valsalva maneuver (Fig. 4.4).
Fig. 4.4
Gray-scale longitudinal image of the left testis (a) demonstrates varicocele as dilated cystic structures in the postero–superior location (arrow). (b) Color flow Doppler image confirms the presence of blood flow (arrow)
Computed Tomography
The main indication of CT in a patient with varicocele is for the evaluation of secondary causes, such as renal mass invading the left renal vein and causing obstruction to left gonadal vein.
Magnetic Resonance Imaging
The more common extratesticular varicoceles have a serpiginous course and a varied signal intensity, depending on flow. They enhance on immediate postcontrast images.
Magnetic resonance imaging of an intratesticular varicocele reveals a tortuous tubular structure hypointense on T1- and T2-weighted images; it had the same signal intensity as testicular parenchyma.
Nuclear Scintigraphy
Scintigraphy is not commonly used to evaluate varicoceles. Occasionally detected is retrograde blood flow in the internal spermatic vein. Relative blood-pool activity in each hemiscrotum appears to correlate with the presence of a palpable varicocele, but the relevance of such scintigraphy is not established.
Pathology
Varicocele
Varicocele is composed of tortuous distended veins of the pampiniform plexus of the spermatic cord. It is thought to be related to incompetence of the valves of the internal spermatic vein. It is much more common on the left than on the right (Fig. 4.5).
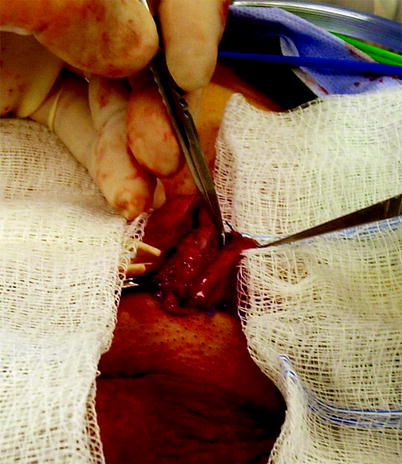
Fig. 4.5
Varicocele. Large veins of the pampiniform plexus of the spermatic cord have been isolated and are about to be divided and ligated in a patient with oligospermia and infertility (Image courtesy of Allen Seftel, M.D.)
The veins show varying degrees of mural thickening, segmental obliteration, smooth muscle hypertrophy, internal elastic degeneration, and sometimes thrombi (Fig. 4.6).
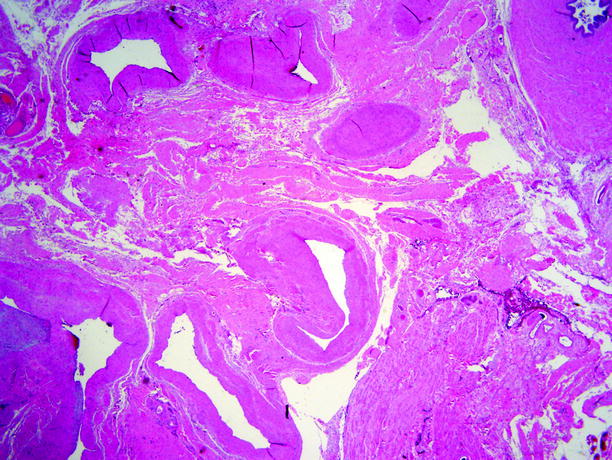
Fig. 4.6
Varicocele. Microscopic section from specimen shown in Fig. 4.5. Markedly dilated veins with eccentric mural fibrosis are present in this section from the spermatic cord. The vas deferens is at upper right. Patient had a varicocele and a testicular germ cell tumor; orchiectomy was done for the latter
The association of varicocele with oligospermia and infertility may be due to disruption and compression of the rete testis cavities and partial obstruction of the tubuli recti by the dilated tortuous veins.
The adverse effects initially involve the ipsilateral testis, but with time, pressure effects develop in the contralateral testis as well.
Hernias
An inguinal hernia is a common paratesticular mass. Hernias are classified as either indirect or direct.
An indirect hernia exits the abdominal cavity through the internal inguinal ring, traversing the inguinal canal into the scrotum. Indirect hernias occur more frequently in children and are associated with a patent processus vaginalis.
A direct hernia is more common in adults, which defines protrusion through the Hesselbach triangle, an area of weakness in the abdominal wall.
Imaging
Plain Film Radiography
Hernias can be diagnosed with plain radiography if the bowel loops contain gas.
Ultrasound
Sonography can be a useful modality to confirm the presence of a scrotal or inguinal hernia or differentiate other etiologies that may simulate hernia. The use of the Valsalva maneuver is critical in demonstrating or defining inguinal hernias, particularly if they are small or contain only omentum.
Hernias are classified as direct or indirect, depending on their relationship to the inferior epigastric artery. The inferior epigastric artery can be demonstrated by using color flow Doppler ultrasound.
Indirect inguinal hernias essentially follow the path of the inguinal contents and therefore begin just lateral to the inferior epigastric vessels.
Direct inguinal hernias protrude through defects in the transversalis fascia that makes up the floor of the inguinal canal; they occur medial to the inferior epigastric vessels.
Colon or small bowel within the inguinal canal appears sonographically as thick-walled, fluid-filled, tubular structures that may demonstrate haustra or valvulae conniventes (Fig. 4.7). Real-time visualization of bowel peristalsis is diagnostic of bowel hernias. Inguinal hernia may be reducible.
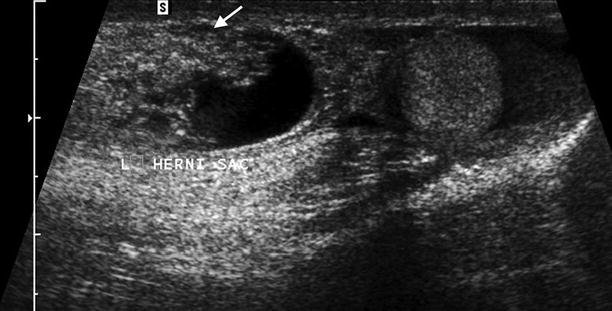
Fig. 4.7
Small bowel is seen as thick-walled, fluid-filled structure (arrow) within the hernial sac
Incarcerated bowel hernias do not demonstrate peristalsis and have peripheral hyperemia. Incarcerated hernias are not reducible.
Computed Tomography
CT is very helpful in large scrotal masses such as large omental hernia or large spermatoceles that cannot be fully visualized with ultrasound. The spermatic cord caudal to the inguinal ligament is clearly visible on CT scans as a structure of soft tissue density surrounded by an elliptical fatty area and by fascia (Fig. 4.8).

Fig. 4.8
Normal spermatic cord is seen as soft tissue density (arrow) on CT
Testicular Appendages and Adnexae
General Information
The testicular adnexae includes the epididymis and the appendages.
Four testicular appendages have been described: the appendix testis (hydatid of Morgagni), the appendix epididymis, the appendix epididymis of the vas aberrans of Haler, and the appendix of the paradidymis (appendix of the cord or organ of Giraldes). Appendix testis is a remnant of the mullerian duct system and the other testicular appendages are remnants of mesonephric duct systems. Appendix testis has been identified unilaterally in 92 % of testes and bilaterally in 69 % in postmortem studies. Appendix epididymis has been identified unilaterally in 34 % of testes and bilaterally in 12 % in postmortem studies. Torsion of the appendix of the testis occurs most commonly around the ages of 6–12 years. It rarely occurs beyond the second decade of life.
The tunica vaginalis invests all but the posterior aspect of the testis and is composed of a visceral portion around the testis and a parietal layer against the scrotal wall. Several pathologic processes can involve this space, predominantly in the form of fluid collections.
Hematoceles (accumulation of blood within the tunica vaginalis) may be either acute or chronic, and they have a more complex heterogeneous appearance with echogenic debris and septations. Possible causes most often include trauma, torsion, tumor, and surgery. A scrotal abscess, or pyocele, is most often a complication of epididymo-orchitis, which has crossed the mesothelial lining of the tunica vaginalis.
Congenital Anomalies
Congenital anomalies affect mostly the vas deferens and the epididymis. Vasal anomalies are the most commonly identified congenital problems affecting the male reproductive tract, often with significant implications for fertility due to the critical normal function of transporting sperm with ejaculation. Congenital bilateral absence of vas deferens (CBAVD) is responsible for 1–2 % of cases of infertility in men. A genetic basis for CBAVD has been provided by its association with cystic fibrosis (CF), with 65–95 % of men with CF demonstrating CBAVD. In the adult, congenital anomalies of the epididymis are most commonly found in association with agenesis of the vas deferens and seminal vesicles because of their common mesonephric origins.
Epididymis
The normal epididymis is homogeneous and well defined. The echotexture of the epididymis is variable and may be hypoechoic, isoechoic, or hyperechoic, relative to the testis (Fig. 4.9).
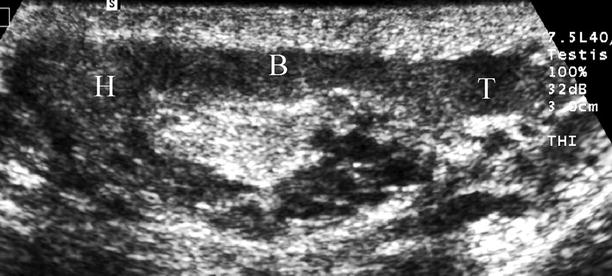
Fig. 4.9
Ultrasound image parallel to the axis of the epididymis. The head (H), body (B), and tail (T) portions are clearly depicted
The appendages of the epididymis are isoechoic structures arising from either the head or the tail. The appendix testis is an isoechoic structure arising from the superior aspect of the testis adjacent to the epididymal head (Fig. 4.10). The appendix epididymis is normally not identified sonographically. The appendix epididymis may, however, swell and distend, forming a cyst-like structure (cyst of Morgagni) that can be seen sonographically and should not be confused with an epididymal cyst (Fig. 4.11).
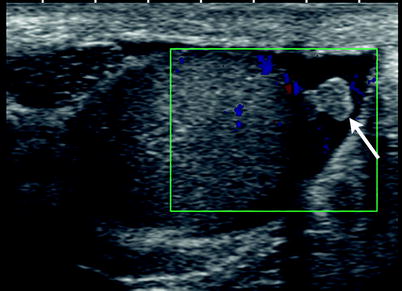
Fig. 4.10
Appendix Testis. Color flow Doppler of the testis reveals a slightly hyperechoic structure directly attached to the testis (arrow). The appendix of testis is torsed as suggested by its hyperechoic appearance, absence of blood flow and minimal fluid surrounding it
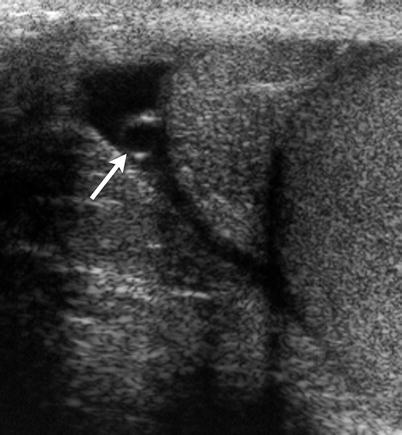
Fig. 4.11
Appendix of epididymis. Gray-scale ultrasound of testis reveals a cystic structure directly attached to the head of the epididymis (arrow). Presence of minimal fluid in tunica vaginalis facilitates its visualization