Timing
Diagnostic task
Suggested procedure
Injection rate
Dose
Typical sequences
Timing not critical
Standard contrast-enhanced imaging
Internal standards to ensure comparability with single-step examinations
Not critical
0.1–0.2 mmol/kg BW
T1w (fs) post CM
Accurate timing essential
MRA
Test bolus for determining individual circulation time
1–3 mL/s by automatic injector
Test bolus of 1–2 mL
MRA
Scan at 0.1–0.2 mmol/kg BW
T1w FLASH 3D
Timing important
Tissue perfusion
Standardized delay
1–4 mL/s by automatic injector
0.1–0.2 mmol/kg BW
T1w FLASH 3D
VIBE
Delay important (specific tissues)
Late imaging
Internal standards to ensure comparability with single-step examinations
Not critical
Depends on CM used
Liver: T1w post CM (delay ≥20 min)
Heart: late enhancement (delay 10–15 min)
Brain: T1w post CM (delay >5 min)
4.1.3 Spasmolytic Medication
The diagnostic quality of MRI of the gastrointestinal tract can be improved by administration of a spasmolytic agent such as butylscopolamine bromide (Buscopan™, Boehringer Ingelheim GmbH, Germany; single adult dose of 20–40 mg, or 1–2 ampoules). Buscopan is contraindicated in subjects with allergies, mechanical obstruction of the gastrointestinal tract, megacolon, prostate hypertrophy with urinary retention, narrow angle glaucoma, tachycardia, and myasthenia gravis. Subjects should be advised not to drive due to possible transient disturbance of accommodation. Alternatively, glucagon can be given as a spasmolytic agent.
4.2 Pulse Sequence Protocols
There are so many potential protocol variations that anything but the most general of recommendations is impossible. In the following, we offer some general guidance, along with some examples of proven protocols.
It is important to plan multistation imaging with enough overlap between adjacent stations (up to 6 cm, depending on the pulse sequence used). This ensures adequate diagnostic evaluation even if wraparound artifacts occur at the seams of adjacent images.
Major whole-body MRI protocol variants, which focus on cardiovascular, oncologic, and musculoskeletal imaging, are discussed in more detail below. In individual cases, these variants can be combined.
4.2.1 Cardiovascular Protocol
Because atherosclerosis is a systemic disease, existing MRI protocols permit assessment of the entire vascular system and at the same time include options for imaging the most important target organs affected by atherosclerotic conditions – the brain, the heart, and the kidneys. Early detection of stenosis (e.g., of the renal or carotid arteries) may have crucial clinical implications. Robust clinical protocols for a comprehensive routine evaluation of the coronary arteries are not yet available. In individual cases, however, imaging approaches that are still under investigation can be used.
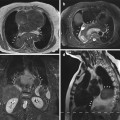
In whole-body MRA, adequate timing is important to capture the first pass of the contrast medium bolus and to sample central k-space data during bolus passage. Since the optimal moment for image acquisition after contrast medium administration is influenced by many different factors (e.g., cardiac output, injection rate, saline chaser), it is recommended that individual circulation time after administration of a test bolus be estimated (1–2 mL of contrast medium administered at a defined flow rate of 1–3 mL/s).
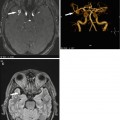
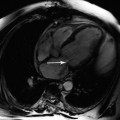
MRA lends itself to combination with pulse sequences aimed at identifying postischemic changes in the brain and heart (Kramer et al. 2005; Fenchel et al. 2005). For the brain, we recommend a TOF MRA sequence, a precontrast FLAIR sequence, and postcontrast T1-weighted imaging. Postinfarction myocardial scars are best identified by hyperenhancement on delayed enhancement images acquired 10–15 min after administration of Gd-based contrast medium for MRA. If deemed useful for the diagnostic question to be answered, the interval between MRA and delayed enhancement imaging may be used for acquiring functional sequences (2D cine TrueFISP) for a full cardiovascular evaluation.
Table 4.2 presents an example of an established protocol for whole-body cardiovascular imaging using two contrast medium injections (Seeger et al. 2008).
Table 4.2
Cardiovascular protocol/whole-body MR angiography: suggested protocol for imaging with two contrast medium injections
Body region/task | Sequence type | Estimated duration |
|---|---|---|
Brain | FLAIR | 2:40 min |
Intracranial vessels | TOF-MRA | 4:00 min |
Determination of circulation time | Test bolus | 1:00 min |
Vessels: abdomen/pelvis, thigh, calfa (pre-CM) | FLASH 3D | 0:50 min |
First contrast bolus | ||
Vessels: abdomen/pelvis, thigh, calfa (arterial) | FLASH 3D (start scan based on circulation time of test bolus) | 0:50 min |
Cardiac function | Cine TrueFISP | 6 × 0:15 min |
Brain | T1w post CM | 4:00 min |
Myocardial viability | IR T1w TurboFLASH (late enhancement) | 6 × 0:15 min |
Vessels: thorax/neck, calfa (pre-CM) | FLASH 3D | 0:17 min |
Second contrast bolus | ||
Vessels: thorax/neck, calfa (arterial) | FLASH 3D (start scan based on circulation time of test bolus) | 0:17 min |
Several alternative protocols have been proposed. These variants include protocols with single-dose contrast medium administration followed by rapid imaging of the neck/chest/abdomen/pelvis (Fenchel et al. 2009), use of a rolling table platform (AngioSURF™, see Chap. 3 (Ruehm et al. 2000)) or a continuously moving table (TIM-CT™, Siemens (Kramer et al. 2008)), and combinations of different techniques (Koziel et al. 2011). Recently, the application of high-resolution time-resolved four-dimensional MRA sequences with a triple injection protocol has been proposed (Kinner et al. 2013) and has shown good diagnostic quality without venous overlay.
4.2.2 Oncologic Protocol
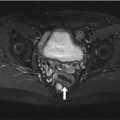
The imaging strategy, including selection of pulse sequences and contrast medium administration, is largely determined by the patient’s primary tumor (Goyen and Schlemmer 2007). When imaging involves a body region for which an established dynamic MRI protocol exists, contrast medium administration is timed for optimized imaging of that region. Examples include dynamic liver MRI and late hepatocyte-phase imaging following administration of a hepatocellular contrast agent.
When whole-body MRI is performed for cancer screening, the protocol is planned according to the individual risk profile. Table 4.3 provides an overview of commonly used pulse sequences, introducing the abbreviations that will be used in the following. Table 4.4 presents examples of oncologic protocols for imaging patients with different primary malignancies. The tables have been modified from Schaefer and Schlemmer (2006).
Table 4.3
Commonly used pulse sequences for whole-body MRI grouped by body region
Body region | Sequence ID | Sequence | Contrast medium | Plane | Breathing mode | Estimated acquisition time (min:s) | Spatial resolution (mm3) |
|---|---|---|---|---|---|---|---|
Whole body | WB1 | T2w STIR TSE | Unenhanced | Coronal | Free | 15:00 | 1.8 × 1.3 × 5.0 |
WB2 | T1w TSE | Unenhanced | Coronal | Free | 10:00 | 1.7 × 1.3 × 5.0 | |
WB3 | T1w TSE fs | Post CM | Coronal | Free | 12:00 | 2.0 × 1.5 × 5.0 | |
WB4 | FLASH 3D | Dynamic CM series | Coronal | Free | 4× (0:15–0:22) | 1.4 × 1.4 × 1.4 | |
Brain | B1 | FLAIR | Unenhanced | Axial | Free | 2:40 | 1.2 × 0.9 × 4.0 |
B2 | T1w SE | Unenhanced | Axial | Free | 3:50 | 0.9 × 0.9 × 4.0 | |
B3 | T1w SE | Post CM | Axial | Free | 3:50 | 0.9 × 0.9 × 4.0 | |
B4 | T1w SE | Post CM | Coronal | Free | 4:20 | 0.9 × 0.9 × 4.0 | |
B5 | TOF 3D | Unenhanced | Axial | Free | 4:00 | 0.8 × 0.8 × 0.8 | |
Neck | N1 | T2w TSE | Unenhanced | Coronal | Free | 2:30 | 1.2 × 0.9 × 5.0 |
N2 | T1w FLASH 2D | Unenhanced | Axial | Free | 0:50 | 1.1 × 0.8 × 5.0 | |
N3 | T1w FLASH 2D fs | Post CM | Axial | Free | 1:20 | 1.1 × 0.8 × 5.0 | |
Thorax | T1 | T2w STIR TSE | Unenhanced | Axial | Breath hold | 0:46 | 1.8 × 1.2 × 6.0 |
T2 | PD VIBE 3D | Unenhanced | Axial | Breath hold | 2× 0:18 | 2.0 × 2.0 × 2.0 | |
T3 | T1w VIBE 3D | Post CM | Axial | Breath hold |