Prevalence
Approx. 0.5 % below age 60, approx. 10 % over age 80; 28 % in patients with PAOD
Location
Extracranial carotid stenosis
Signs and symptoms
Approx. 2 % stroke rate per year when asymptomatic and detected incidentally
Clinical Management
All subjects with asymptomatic stenosis of the carotid artery, the vertebral arteries, or the intracranial circulation should see a neurologist to determine whether other risk factors for cerebrovascular events exist and whether drug therapy or interventional/surgical management is necessary.
9.1.3 Stenosis of Lower Extremity Arteries
Peripheral arterial occlusive disease (PAOD) is an umbrella term for all forms of impaired arterial circulation caused by stenotic or obstructive vascular processes including lesions of the aorta and arteries supplying the extremities (Spengel et al. 2001). Chronic arterial occlusive disease, unlike acute disease, is characterized by slow development of single or multiple stenotic lesions, which in over 90 % of cases affect the arteries of the pelvic region and legs. Steno-occlusive disease of the leg arteries leads to intermittent claudication due to muscle ischemia and increasingly limits the pain-free walking distance. About 20 % of patients with poor circulation of the legs have PAOD (Alexander 1992).
Three types of occlusive disease of the lower extremities can be distinguished by level of involvement: (1) aortoiliac disease with steno-occlusive lesions in the aorta and/or iliac arteries, (2) femoropopliteal PAOD, and (3) PAOD of more distal arteries (calf and foot). Only about one third of PAOD patients have ischemic symptoms (McDermott et al. 2002). Many patients limit their activities to reduce PAOD-related symptoms. Initially, they report feeling well but when questioned admit that they can only walk a short distance (Table 9.2).
Table 9.2
Stenosis of lower extremity arteries
Prevalence | Age related |
2.5 % < 60 years | |
18.8 % > 70 years | |
Location | 1. Aortoiliac PAOD |
2. Femoropopliteal PAOD | |
3. Calf and foot (anterior tibial artery > posterior tibial artery > fibular artery) | |
Signs and symptoms | Asymptomatic incidental finding, reduced walking distance, rest pain, necrosis, gangrene |
The prevalence of stenotic and occlusive lesions of the distal leg varies with age and sex and also depends on the presence of risk factors (Kannel et al. 1970). The leading risk factors are smoking, diabetes mellitus, arterial hypertension, hyperlipoproteinemia, hypercholesterolemia, and hyperfibrinogenemia. The prevalence is 2.5 % before age 60 and as high as 18.8 % in those over 70 (Kannel 1996). Half of patients with lower leg occlusion have diabetes mellitus (Albers et al. 2005; Hirsch et al. 2005; Schneider et al. 1993).
PAOD patients have an increased risk of cerebrovascular and cardiovascular events (Criqui et al. 1997; Ness and Aronow 1999); the risk is the same regardless of whether they are symptomatic or asymptomatic (Hooi et al. 1998, 2001). Hence, the traditional concept of asymptomatic PAOD seems to downplay the risk. Patients with chronic PAOD have a mortality rate of over 20 % in the first year after diagnosis (Hirsch et al. 2005). Atherosclerotic occlusion most commonly affects the anterior tibial artery, followed by the posterior tibial artery and the fibular artery. Occlusion of a single calf artery with patency of the other branches is clinically silent. MR angiography with administration of gadolinium-based contrast medium is comparable to digital subtraction angiography (DSA) in terms of specificity and sensitivity for anatomic localization and grading of stenosis severity (Fig. 9.1).


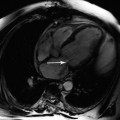
Fig. 9.1
Stenosis (arrow) of the left superficial femoral artery on MIP image
Evaluation of vascular disease of the upper extremities was not part of the whole-body MRI protocol used.
Clinical Management
Multiple occlusions of lower leg arteries can be treated medically, interventionally, or surgically. The best treatment should be determined by interdisciplinary consensus on the basis of clinical parameters.
When no symptoms are present or when the subject feels well, management focuses on identifying and reducing risk factors such as smoking, diabetes mellitus, hypertension, and hyperlipoproteinemia. These risk factors should be screened for in a thorough history and brought to the subject’s attention.
An inexpensive and simple test for evaluating arterial insufficiency is to determine the ratio of ankle systolic pressure to brachial systolic pressure, the ankle-brachial index (ABI). An ABI of 1.00–1.29 is considered normal, while values between 0.5 and 1.0 indicate moderate PAOD. Values below 0.4 suggest an increased risk of developing rest pain and ischemic necrosis (Hirsch et al. 2005). Another measure of disease severity is the distance an individual can walk without pain.
Treatment of Fontaine stage 2 disease is primarily physical and medical and aims at reducing or eliminating risk factors.
Chronic stage 3 and 4 occlusions require interventional or surgical revascularization but are unlikely to be encountered as incidental findings in the screening situation or in epidemiologic studies of healthy subjects.
9.1.4 Renal Artery Stenosis
A prevalence of renal artery stenosis (RAS) of 6.8 % has been reported by Hansen et al. (2002), but in high-risk groups, it may be as high as 50–70 % (Schwartz and White 1964; Harding et al. 1992; Weber-Mzell et al. 2002; Jean et al. 1994). Roughly two thirds of renal artery stenoses are due to atherosclerotic plaques, and one third of these are bilateral. Fibromuscular dysplasia accounts for the other third. Uni- or bilateral RAS underlies the development of arterial hypertension in 1–5 % of cases. Fibromuscular dysplasia is the predominant cause of RAS in young patients, usually women aged 20–40, and tends to affect the distal renal arteries. New-onset hypertension or progression of known hypertension in older individuals is mostly attributable to atherosclerotic stenosis, which typically involves the proximal renal arteries (Fig. 9.2).
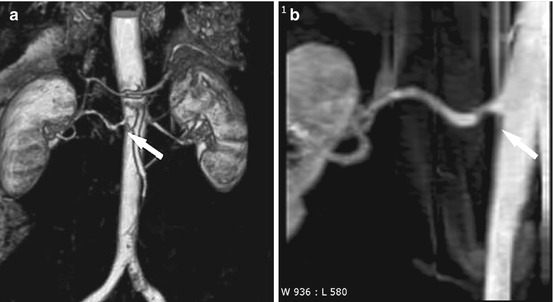
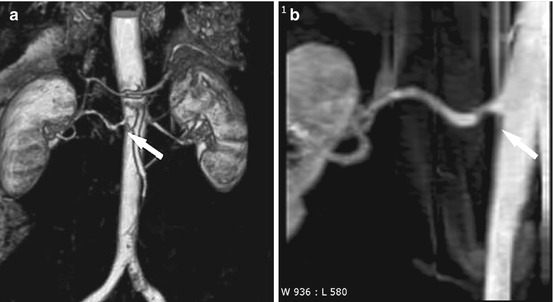
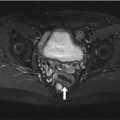
Fig. 9.2
Right-sided RAS (arrow) on VRT (a) and MIP (b) images
Clinically, RAS may be asymptomatic or may present with renovascular hypertension or renal dysfunction. Mixed forms are also possible (Balk et al. 2006; Safian and Textor 2001). RAS greater than 70 % is considered hemodynamically relevant.
Clinical Management
In the routine diagnostic setting, mild hypocalcemia, which indicates activation of the renin-angiotensin-aldosterone system, can alert the physician to the diagnosis of renal artery stenosis. Several tests are available to assess renin release. The sensitivity and specificity of plasma renin activity measurement can be improved by furosemide stimulation. When renin in renal vein blood is determined separately for each side, a ratio of renin levels ≥1.5 (stenotic versus nonstenotic side) is considered abnormal. An abnormal ratio and an absolute increase in plasma renin activity reliably predict RAS as the underlying cause of hypertension – a condition that is potentially curable by surgery or angioplasty.
9.1.5 Mesenteric Artery Stenosis
An acute ischemic event is not likely to be encountered in the classic screening situation. It is more likely to incidentally detect chronic mesenteric stenosis promoting or maintaining ischemia of upper abdominal organs and of the small and large intestines (abdominal angina).
The incidence of chronic occlusive disease of a mesenteric artery is approx. 5 % in patients presenting with abdominal pain of unknown cause. Because chronic occlusion progresses slowly and collaterals provide compensatory blood supply, the imaging appearance or autopsy findings do not tend to correlate with the clinical picture. Mesenteric stenosis is present in 80 % of individuals over 60 but rarely becomes clinically apparent. Symptoms do not develop unless there is appreciable ischemia in a target organ, which in turn requires a high-grade stenosis of at least 70 % (Luther 2001).
Clinical Management
There are four clinical stages of chronic mesenteric ischemia:
1.
Asymptomatic stage
2.
Intermittent abdominal complaints (abdominal angina, recurrent organ insufficiency)
3.
Abdominal pain at rest
4.
Ischemic organ lesion (infarct)
A typical manifestation is postprandial abdominal pain persisting for 3–4 h after eating. Chronic visceral artery occlusion is characterized by the classic triad of abdominal pain, weight loss, and paraumbilical murmur.
An asymptomatic individual (stage 1) needs no treatment. Stage 2 and 3 disease is an absolute indication for treatment, and stage 4 is an emergency.
9.2 Aneurysm
9.2.1 Intracranial Aneurysm
Time-of-flight MR angiography (TOF-MRA) of the intracranial arteries is a suitable screening tool for intracranial aneurysms (Raaymakers et al. 1999) (Fig. 9.3). The wide range of sensitivities (74–100 %) reported for aneurysm detection by MRA is in part attributable to the investigation of different patient populations (ruptured versus nonruptured aneurysm) and technical advances. The TOF-MRA technique used here offers better resolution than contrast-enhanced MRA (CE-MRA). Unlike CE-MRA, TOF-MRA is not limited by a narrow imaging window (which requires careful bolus timing) and thus avoids the problem of venous overlay in aneurysm imaging (Ozsarlak et al. 2004).
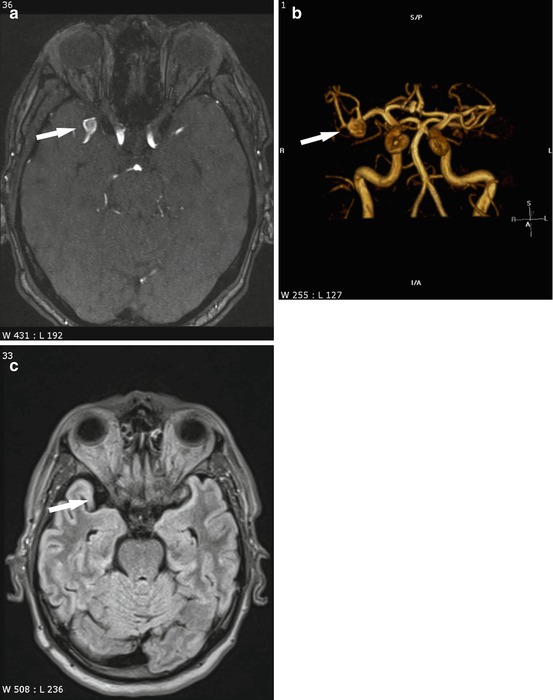
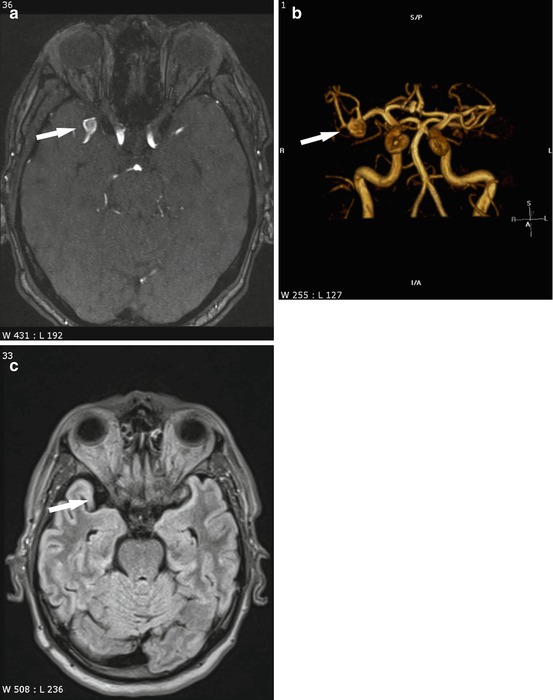
Fig. 9.3
Right-sided middle cerebral artery bifurcation aneurysm (arrow) on TOF (a) and VRT (b) images. The FLAIR image (c) shows normal flow void
Intracranial aneurysm is the most common cause of acute subarachnoid hemorrhage (SAH) and/or intracerebral bleeding, accounting for about 75 % of cases. Aneurysmal bleeding is estimated to occur in approx. 5–10 cases/100,000 population per year (Rinkel et al. 1998). The estimated prevalence of cerebral aneurysm is approx. 2.3 % in the adult population (Rinkel 2008). Most cerebral aneurysms are small and are located in the anterior circulation. In Germany, it is assumed that approx. 1.5–2 million individuals have aneurysms, among them 30 % with multiple aneurysms (Table 9.3).




Table 9.3
Intracranial aneurysm
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree