Contrast-Enhanced Ultrasound: Clinical Applications
Harshawn Malhi, MD
Raymond Azab, MD
Vinay Duddalwar, MD, FRCR
Edward G. Grant, MD, FACR
▪ Introduction
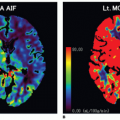
The clinical application of non cardiac contrast-enhanced ultrasound (CEUS) has been steadily gaining traction over the past decade. Traditionally, ultrasound (US) without the use of perfusion agents sufficed given the intrinsically high contrast between blood and solid tissue and the effective ability of color Doppler to quantify hemodynamic parameters such as direction and velocity of blood flow. With the advent of newer and more sophisticated contrast agents, these fundamental capabilities have allowed for superior visualization of the microcirculation, once a domain restricted to angiography, contrast-enhanced computed tomography (CECT) and contrast-enhanced magnetic resonance (CEMR) imaging. Contrast use in US can provide a detailed analysis of vascular structures and allow for imaging of lesions and organs in real time. The advantages of CEUS include a real-time dynamic imaging modality with a good safety profile and a contrast agent that is not nephrotoxic. In addition, it is indispensable in patients with critical renal function that may have contraindications to receiving CECT or CEMR imaging. This chapter will provide a survey of the current clinical applications and potential future uses of CEUS on selected organs.
▪ Contrast Agents
The most common indication for performing a CEUS examination is the characterization of a focal visceral mass. Malignancy induced angiogenesis allows for tumor growth, which in turn can be exploited to aid in diagnosing tumors. The detection of tumoral neovascularization is one of the fundamental aspects of oncologic imaging. It is from this basic principle that several contrast US agents arose.
The US contrast agents in use today consist of second-generation agents composed of tiny bubbles of a perfluorocarbon gas contained within a stabilizing shell made from a lipid or protein, commonly referred to as microbubble contrast agents. These microbubbles are smaller than red blood cells, and thus they avoid filtration in the lungs and the heart. They are true “blood pool” agents in the sense that they do not diffuse through the vascular endothelium (as compared to the contrast agents of CT and MRI).
Microbubble contrast agents are useful in that the perfluorocarbon gas is highly echogenic and provides contrast from the background tissue. These agents also interact with image processing. The major determinant of this interaction is the peak negative pressure of the transmitted US pulse, reflected by the mechanical index (MI). When exposed to a low MI, the agents display stable nonlinear oscillations in the presence of the US beam pulse, which generate harmonics of the transmitted frequency, including a frequency double that of sound emitted by the transducer, the second harmonic. The bubbles can undergo irreversible destruction, if the MI is raised to a sufficient level. This produces a brief but bright US echo.
▪ Breast
The primary utility of CEUS in the breast is oncologic. Angiogenesis plays a key role in the breast cancer growth and metastasis. Vascular morphology varies between benign and malignant lesions. Malignant lesions contain irregular and tortuous vessels that are peripherally based, whereas benign lesions have a smooth contour1,2 (Fig. 34-1). Color and power Doppler US is limited in that it cannot evaluate the microvasculature architecture of breast lesions.3 Compared with Doppler US, CEUS offers better sensitivity in the visualization of pathologic microvessels in neoplastic tissue.4
Several studies have been published demonstrating the effectiveness of CEUS in differentiating malignant from benign breast lesions by capitalizing on tumor angiogenesis. A study by Wan et al.5 using second-generation contrast agents compared both the contrast enhancement pattern (qualitative analysis) and contrast enhancement kinetic analysis (quantitative analysis) of 91 breast lesions with histopathologic correlation. Malignant lesions more often showed heterogeneous and centripetal enhancement, whereas benign lesions mainly showed homogeneous and centrifugal enhancement. For quantitative analysis, malignant lesions showed significantly higher and more rapid enhancement than benign lesions. The time to peak (TTP) was also significantly shorter for malignant lesions. Studies have also shown that, following contrast administration, invasive breast carcinomas exhibit earlier TTP and more rapid washout. These aggressive lesions were associated with established predictors of poor prognosis. Importantly, studies have also demonstrated that CEUS kinetics can discriminate benign from malignant breast lesions similar to CEMRI, which is currently the gold standard imaging modality for evaluating tumor angiogenesis.6,7,8 and 9
Several studies have reported that the potential of CEUS in the evaluation of tumor perfusion before and after neoadjuvant chemotherapy. Traditionally, decrease in tumor volume has been used to evaluate response, but changes in tumor vascularity can also be utilized for assessment.10,11 and 12 Specifically, CEUS can demonstrate decreases in overall tumor perfusion, peak intensity, and size following neoadjuvant therapy (Fig. 34-2). Despite these promising results, CEMRI remains the gold standard for evaluating tumor response following neoadjuvant therapy.13
CEUS may also be of value in depicting tumor recurrence after initial treatment, specifically differentiating tumor recurrence versus postsurgical scar. Scars may appear as suspicious lesions
on conventional US, often hypoechoic with posterior shadowing, similar to many malignant tumors.10 In essence, recurrent tumors will demonstrate angiogenesis (enhancement), whereas scars demonstrate minimal to no enhancement.
on conventional US, often hypoechoic with posterior shadowing, similar to many malignant tumors.10 In essence, recurrent tumors will demonstrate angiogenesis (enhancement), whereas scars demonstrate minimal to no enhancement.
In summary, the exact role of CEUS in the spectrum of oncologic imaging for breast tumors is still evolving and has yet to be standardized. Currently, CEMRI is the gold standard modality utilized to evaluate tumor vascularity and angiogenesis, response to neoadjuvant therapy, and recurrence after resection. CEUS of breast lesions thus may eventually play a similar or complementary role to CEMRI.10
▪ Liver
The characterization of focal liver lesions has long been a challenging and essential part of medical imaging. CT attenuation, MRI signal, and echogenicity on conventional US taken alone are often nonspecific characteristics. The distinguishing feature of many lesions remains their vascularity and hemodynamic qualities. These unique enhancement characteristics are afforded by the dual blood supply of the liver by the hepatic artery (25% to 30%) and the portal vein (70% to 75%). CEUS has become increasingly accepted as an equally effective and sustainable alternative to multiphase CEMR or CECT while saving both cost and harmful radiation to the patient. Currently, several established indications exist for the clinical use of CEUS in the liver (Table 34.1).
Hemangioma: Cavernous and Flash
Histologically, hemangiomas consist of multiple vascular channels lined by a single layer of endothelium and separated by fibrous septa. Cavernous hemangiomas are the most common benign tumors of the liver, occurring in approximately 4% of the population. The vast majority of hemangiomas are small and asymptomatic, usually discovered incidentally. Potentially malignant lesions such as hypervascular metastases or hepatocellular carcinoma (HCC) can have a similar sonographic appearance to hemangiomas. Sonographically, the typical appearance of a hemangioma is homogeneously hyperechoic, possibly with posterior acoustic enhancement. Of note, echogenicity is relative to the background tissue; thus, in the setting of hepatic steatosis, a hemangioma may appear hypo- or isoechoic relative to the echogenic fatty liver parenchyma.14 Larger hemangiomas may be heterogeneous in appearance with the central hypoechoic foci representing large vascular spaces or fibrous collagen scars.
TABLE 34.1 Uses of Contrast Ultrasound in the Liver | |
|---|---|
|
On CEUS, hemangiomas will initially demonstrate the typical peripheral globular nodular enhancement. This is followed by the centripetal progression of the enhancement until the entire lesion is enhancing and hyperechoic compared to the background liver parenchyma (Fig. 34-3). This enhancement usually persists into the portal venous phase and may last for several minutes.15 Smaller “flash” hemangiomas will demonstrate diffuse immediate arterial enhancement that will often persist on the later phases.16
Focal Nodular Hyperplasia
Focal nodular hyperplasia (FNH) is the second most common benign liver mass and does not carry malignant potential. They are most common in women of childbearing age. Histologically, these lesions represent developmental hyperplastic lesions thought to be
related to a focal congenital vascular malformation.17 This results in a histologic mix of abnormally arranged non neoplastic hepatocytes, Kupffer cells, biliary ducts, and components of portal triads. Similarly to hemangiomas, FNH is usually asymptomatic and discovered incidentally.
related to a focal congenital vascular malformation.17 This results in a histologic mix of abnormally arranged non neoplastic hepatocytes, Kupffer cells, biliary ducts, and components of portal triads. Similarly to hemangiomas, FNH is usually asymptomatic and discovered incidentally.
Sonographically, FNH can be very subtle, often referred to as the “stealth lesion.” This is in large part because histologically, FNH is essentially hyperplastic normal liver tissue; and therefore, shares similar echogenicity to the normal hepatic parenchyma. If seen, a FNH will be typically made apparent by the displacement of normal surrounding vasculature and subtle contour abnormalities rather than an inherent difference in the echogenicity of the lesion. The typical linear or stellar central scar seen in FNH is usually hypoechoic, though occasionally hyperechoic.18 On Doppler US, well-developed peripheral and central blood vessels may be seen coursing through a well-circumscribed central scar.
On CEUS, FNH is hypervascular in the arterial phase (predominately within the central scar) and enhances more than the background liver parenchyma. Additionally, a large feeding vessel can often be seen on the arterial phase. This is followed by the centrifugal filling direction in the portal venous phase (in contrast to the centripedal filling seen in hemangiomas). Enhancement is sustained in the portal venous phase with equal or greater enhancement than the background liver tissue (Fig. 34-4). Occasionally, an unenhanced scar may be seen in both the arterial and portal venous phases. Usually, the conventional US and CEUS findings of FNH are fairly specific, and no further imaging is needed. If further clarification is required, a sulfur colloid scan or biopsy may be performed to confirm the diagnosis.
Adenoma
Adenomas are tumors consisting of normal to slightly atypical hepatocytes, which occasionally contain bile ducts, Kupffer cells, calcification, and fat, thus making their appearance highly variable on imaging. They can range in size from 8 to 15 cm and are associated with females using oral contraceptives. Although typically asymptomatic, adenomas are known to present with severe pain in the setting of hemorrhage or infarction. This complication can ultimately result in rupture, hemoperitoneum, and shock, making the management of incidentally detected adenomas slightly more complicated. Small adenomas are often managed conservatively, whereas large or growing adenomas may be resected to avoid the potential complications of rupture.
As mentioned above, the histologic variability of adenomas makes their imaging characteristics equally varied and their sonographic appearance nonspecific. They may be hyperechoic, hypoechoic, isoechoic, or heterogeneous. In regards to their vascularity, adenomas can demonstrate well-defined intralesional blood vessels (usually venous), and can therefore be indistinguishable from FNH based on their conventional US and Doppler appearance.19 Sulfur colloid studies are often used to differentiate between the two given the characteristic cold appearance of adenomas (due to the relative lack of Kupffer cells) in opposition to FNH that appears hot.
CEUS is a useful tool in helping discriminate between these two hypervascular lesions that are managed differently. Adenomas will typically be hypervascular on the arterial phase just as FNH, though usually to a lesser extent20 (Fig. 34-5). The distinguishing factor, however, is the centripetal filling pattern seen on the subsequent phases with adenomas. This is in contrast to the centrifugal filling pattern of FNH.
Regenerative/Dysplastic Nodules
Regenerative and dysplastic nodules both occur in the setting of cirrhosis. Regenerative nodules represent benign localized proliferation of liver parenchyma (with normal hepatocellular function and Kupffer cells) within a cirrhotic liver in response to liver injury. These nodules may progress to become dysplastic nodules, which are premalignant and classified further as low or high grade based on degree of dysplasia.
Regenerative and dysplastic nodules are often sonographically occult. When seen, they can have any degree of echogenicity. On CEUS, regenerative nodules will usually show similar arterial phase and portal venous phase vascularity and enhancement to the remainder of the cirrhotic liver. Dysplastic nodules may demonstrate transient arterial phase hypovascularity followed by isovascularity.21 Both regenerative and dysplastic nodules are usually supplied by the portal venous system.
Hepatocellular Carcinoma
HCC is the most common primary visceral malignancy in the world, accounting for 80% to 90% of all primary liver malignancies. It is predominantly seen in males (5:1) and in the setting of cirrhosis (alcoholic and viral).18 Although usually solitary tumors, HCCs may also be multifocal or infiltrative in nature. Particular evaluation of the portal venous system is necessary as tumor thrombus is a common complication. Sonographically, HCC is variable in appearance. When larger in size, they often have mixed echogenicity due to tumor necrosis and hypervascularity. Conversely, smaller lesions are usually solid and appear hypoechoic. HCCs can also be hyperechoic, if there is fatty metamorphosis or sinusoidal dilation. Small hyperechoic HCCs can therefore simulate hemangiomas, hypervascular metastases, or lipomas. On color Doppler, HCCs usually show hypervascularity and tumor shunting.
 Figure 34-6. Hepatocellular carcinoma (HCC) demonstrating arterial enhancement and washout (arrows). A: Intense early arterial enhancement. B: Contrast washout of HCC on later phase (4-minute delay). |
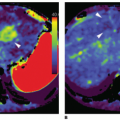
On CEUS, HCCs demonstrate the classic and characteristic arterial enhancement owing to arterial neovascularity (Fig. 34-6). This is followed by decreased portal venous flow (“washout”) as also seen on four-phase CEMRIs and CECTs. The arterial phase may exhibit dysmorphic vessels with intervening regions of necrosis or scarring. The portal venous phase demonstrates washout with the lesion appearing hypoechoic compared to the background liver parenchyma. Given the unique and easily identifiable enhancement pattern of HCC, CEUS may contribute to the surveillance of suspicious lesions detected in patients with known predisposing factors. Of note, several atypical variations of enhancement patterns of HCCs have been described, including arterial phase hypovascularity with delayed or no enhancement and arterial enhancement without washout.21
Tumor thrombus in the portal or hepatic veins contains malignant neovascularity that can also be demonstrated with CEUS.
The enhancement patterns should be similar to the tumor from which it originated and will have a different appearance than a normally enhancing vessel (an arterial tumor blush rather than discrete vessels)22 (Fig. 34-7). A marked washout in the portal and late phases may occur in metastatic portal vein thrombosis, up to an anechoic appearance, resembling bland thrombus in this vascular phase (Fig. 34-8).
The enhancement patterns should be similar to the tumor from which it originated and will have a different appearance than a normally enhancing vessel (an arterial tumor blush rather than discrete vessels)22 (Fig. 34-7). A marked washout in the portal and late phases may occur in metastatic portal vein thrombosis, up to an anechoic appearance, resembling bland thrombus in this vascular phase (Fig. 34-8).
Fibrolamellar HCC is a histologic subtype of HCC, which is often seen in younger patients and is not associated with chronic liver disease. These tumors are usually solitary and well encapsulated. Similar to HCC, fibrolamellar HCCs can have variable sonographic appearances. Common findings include punctate calcifications and a hyperechoic central scar. On CEUS, fibrolamellar HCCs will typically demonstrate heterogeneous arterial enhancement secondary to necrosis with washout on the portal venous phase.
Cholangiocarcinoma
Cholangiocarcinomas are the second most common primary hepatic tumor after HCC. They are highly malignant and occur primarily in the sixth and seventh decades of life. Histologically, cholangiocarcinomas are usually adenocarcinomas arising from the bile duct epithelium. They can arise peripherally or centrally in the liver with the hilar variant known as a Klatskin tumor. Given their biliary origin, both variants may cause proximal biliary ductal dilation secondary to luminal obstruction.
Sonographically, cholangiocarcinomas usually appear as a mixed echogenicity mass with associated biliary ductal dilatation. On CEUS, most cholangiocarcinomas show peripheral irregular rim-like enhancement with heterogeneous central hypoenhancement during the arterial phase, followed by characteristic
washout on portal and late phases. Minimal enhancement of irregularly thickened bile ducts may be seen on the portal venous phase.
washout on portal and late phases. Minimal enhancement of irregularly thickened bile ducts may be seen on the portal venous phase.
Angiosarcoma
Angiosarcomas are extremely rare malignant tumors typically occurring in the 6th and 7th decades. There is a reported association with certain carcinogens (thoratrast, arsenic, and polyvinyl chloride).23 There are several morphologic types including a single mass, multifocal hypervascular masses, or diffuse infiltration of the liver. Early metastatic spread to the spleen and lung are common. Sonographically, these tumors are almost always heterogeneous in appearance and demonstrate diffuse arterial enhancement with CEUS, given their moderately hypervascular nature, which persists into the venous phase. They are typically fed by large peripheral vessels with centripetal flow, similar to the enhancement pattern of hemangiomas on CEUS.
Cystadenocarcinoma
Cystadenocarcinomas are rare malignant or premalignant cystic tumors that likely arise from the ectopic nests of primitive biliary tissue. They are typically complex, multilocular cystic masses with septations and mural calcifications. Sonographically, cystadenocarcinomas appear as large, well-defined multiloculated anechoic masses with highly echogenic septa. Nodular components may or may not be present, because they are largely avascular, minimal enhancement is seen with CEUS; however, abnormal enhancing vessels may be seen peripherally or within the septa.
Metastases
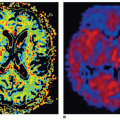
Metastases are the most common liver tumor in the United States, up to 20 times more common than HCC.18 Metastatic lesions to the liver most commonly originate from primary tumors of the gallbladder, colon, stomach, pancreas, breast, and lung. Sonographically, they may be hypo-, iso-, or hyperechoic depending on their vascularity. They may or may not have a hypoechoic halo representing surrounding edema, as can also be seen with HCC. Many metastatic lesions are of similar echogenicity to the background liver, making their detection difficult or impossible. CEUS is an effective method to help combat this problem and improve lesion visibility on US. On CEUS, the appearance of metastatic disease on the arterial phase is variable depending on the vascularity of the lesion. Hypovascular metastases (i.e., gastrointestinal tumors, lung) are hypoenhancing on the arterial phase, whereas hypervascular metastases (i.e., neuroendocrine tumors, thyroid, renal) are hyperenhancing on the arterial phase (Fig. 34-9). The portal venous and late phases are often more useful in detecting and characterizing metastases. On these phases, metastases often become more apparent as hypoenhancing defects. Taken together, this means that hypervascular metastases may have a similar enhancement pattern to HCC, with hyperenhancement on the arterial phase and washout on the portal venous and delayed phases. When detected initially on US, the diagnosis can be confirmed with tissue sampling.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree