Osmolality
Ionic
Nonionic
High-osmolar contrast materials
Monomers:
Iothalamate: Conray
Diatrizoate: Renovist, Hypaque, all others
Low-osmolar contrast materials
Dimer:
Monomers:
Ioxaglate: Hexabrix
Iohexol: Omnipaque
Iopamidol: Isovue
Ioversol: Optiray
Iopromide: Ultravist
Ioxilan: Oxilan
Dimer: Iodixanol(Visipaque)
(a)
High–osmolar ionic monomers: These contrast materials are monomers and have a single benzene ring in their chemical structure. Cations attached to the benzene ring may be either sodium or meglumine. Each benzene ring binds three iodine atoms. The osmolality value of this group (1,570 mOsm/kg H2O) is significantly higher than that of serum (290 mOsm/kg H2O). Iodine/particle (I/P) value of this group is 0.5.
(b)
Low–osmolar nonionic monomers: Contrast materials of this group are composed of nonionic compounds. They are soluble in water. This group also includes three iodine atoms bound to each benzene ring. No dissociation occurs in water. The osmolality value of this group is 518 mOsm/kg H2O. These contrast materials have an I/P value of 3.
(c)
Iso–osmolar nonionic dimers: These contrast materials are the most recently introduced iodinated contrast agents. Their structure includes two benzene rings; three iodine atoms are bound to each benzene ring. They do not dissociate in water. The osmolality value of this group is the same as that of serum. These contrast materials have an I/P value of 6.
Physiology of Side Effects
The side effects of iodinated contrast materials (CM) are related to their osmolality. Low-osmolar contrast materials (LOCM) are less often associated with severe CM reactions in comparison to high-osmolar contrast materials (HOCM), but no significant difference in the incidence of fatal reactions associated with the two types of agents has been identified.
Adverse effects of contrast materials can be dose dependent or nondose dependent. Serious adverse effects are usually nondose dependent.
Contrast material reactions are classified as nonallergenic anaphylactic reactions, since no antigen-antibody interaction has been identified in these reactions.
Serious contrast reactions begin within minutes of exposure to the contrast agent. Various types of chemotactic, vasoactive, and spasmogenic agents contribute to contrast reactions. The mechanisms by which contrast materials induce activation of these mediators are not well understood. Suggested mechanisms include direct effects of CM particles on basophils and mast cells, activation of immunological mechanisms involving IgE antibodies, stimulation of thymus-derived lymphocytes (T cells), or activation of the complement system.
The most important agent in the reaction cascade is histamine. Histamine resides within basophils and mast cells and is released from these cells in response to stimuli. Other mediators involved in contrast reactions include leukotrienes, prostaglandins, enzymes, and cytokines. These substances induce vasodilatation, contraction of smooth muscle cells, and increased mucus secretion in airways. Vasodilatation causes edema and contraction of smooth muscles results in bronchospasm.
Contrast materials can also activate factor XII (Hageman factor) of the clotting system, which results in activation of the kinin system. Bradykinin can induce vasodilatation, bronchospasm, and increased vascular permeability. It is also a potent activator of factor XII, prompting autocatalytic amplification of the initial stimulus. Bradykinin may also activate arachidonic acid, which causes increased production of prostaglandins and leukotrienes.
Patient anxiety has been suggested as a contributory factor in CM reactions, but no definite mediator-related mechanisms have been shown to be involved in anxiety-associated CM reactions.
Low-osmolality contrast materials are less active in stimulating these mechanisms in comparison to high-osmolality contrast materials.
The hydrophilicity or protein-binding characteristics of contrast materials do not seem to influence histamine release reactions.
There is positive correlation between the size and complexity of the CM and histamine release reactions.
Contrast materials may also cause chemotoxic effects which result from direct molecular toxicity and physiologic properties of CM. Debilitated and medically unstable patients are more susceptible to these adverse effects.
Contrast-Induced Nephrotoxicity
Contrast-induced nephrotoxicity (CIN) is defined as deterioration in renal status secondary to the administration of contrast material.
Preexisting renal disease and inadequate hydration increase the likelihood of nephrotoxicity.
Contrast-induced nephrotoxicity can be quantitatively defined as a 20–50 % rise in serum creatinine and absolute elevation from baseline (increase of 0.5–2.0 mg/dl) within 48 h of injection of contrast material.
Serum creatinine usually begins to rise within the first 24 h following IV contrast medium administration, peaks within 96 h (4 days), and usually returns to baseline within 7–10 days (Fig. 1.1).
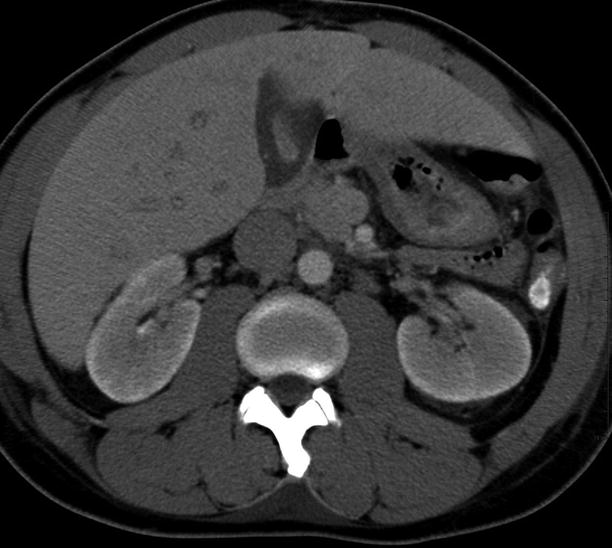
Fig. 1.1
Contrast-induced nephrotoxicity. Axial contrast-enhanced CT demonstrates bilateral persistent nephrogram at 20 min of delay after contrast administration suggestive of renal excretion dysfunction
Since the serum creatinine level can vary widely in healthy people unexposed to contrast agents, the estimated glomerular filtration rate (eGFR) has been accepted as a more reliable parameter in evaluating a patient’s risk for CIN.
The risk of CIN is about 0.6 % in patients with an eGFR greater than 40 ml/min, 4.6 % in patients with an eGFR less than 40 ml/min but greater than 30 ml/min, and 7.8 % in patients with an eGFR < 30 ml/min. No data exists on the risk of CIN in children.
In the follow-up of patients, renal insufficiency is defined by a creatinine clearance of less than 60 ml/min, and the term “renal failure” is invoked if creatinine clearance is less than 30 ml/min.
Pathogenesis
CIN may result from administration of high-osmolality ionic contrast media (HOCM), low-osmolality contrast media (LOCM), and iso-osmolality contrast media (IOCM). The incidence of CIN increases with the amount of CM administered. The causative mechanisms in CIN are classified as follows:
(a)
Renal hemodynamic changes (vasoconstriction)
(b)
Direct tubular toxicity of contrast material
Risk factors
The risk factors for CIN are summarized in Table 1.2. It is unusual for patients with normal renal function to experience CIN. The risk of developing CIN is a relative contraindication for contrast administration. The highest risk factors for development of acute renal failure are diabetes mellitus and preexisting renal insufficiency.
Table 1.2
The risk factors for CIN
Preexisting renal insufficiency (serum creatinine level > 1.5 mg/dl)
Diabetes mellitus
Dehydration
Cardiovascular disease
Use of diuretics
Advanced age (>70 years)
Multiple myeloma
Hypertension
Hyperuricemia
In patients with no history, signs, or symptoms of renal disease, the risk of contrast-induced alteration in renal function is below 1 %.
The reported risks of contrast-induced alteration in renal function in the presence of preexisting renal impairment and diabetic nephropathy are 12–27 and 50 %, respectively. Since elimination of contrast material from the body takes 24 h, repeat contrast administration within this time period may increase the risk of CIN.
Low-osmolality iodinated CM are less nephrotoxic than HOCM. The nephrotoxic effects of LOCM and IOCM appear to be same in large clinical trials.
Dehydration causes decreased renal blood flow and glomerular filtration rate and prolonged tubular exposure to contrast media, all of which accentuate the effects of contrast media on the kidney.
Metformin does not directly induce CIN, but metformin-related lactic acidosis may be severe in patients with CIN because of decreased excretion of metformin.
Metformin stimulates lactic acidosis by increasing intestinal lactic acid production. In order to avoid lactic acidosis associated with acute renal failure, metformin should be withheld at the time iodinated contrast is used. It may be resumed 48 h after a contrast study, provided that renal function is shown to be normal.
Prevention
Close attention to renal function and adequate hydration are essential in preventing CIN. If the patient cannot be hydrated orally, IV infusion of 0.9 % saline at 100 ml/h in adults beginning 6–12 h before and continuing 4–12 h after the administration of contrast media should be performed.
Although N-acetylcysteine can decrease the serum creatinine levels, its role in preventing renal damage is controversial. The popular regimen of oral acetylcysteine, 600 mg twice daily on the day before and on the day of administration of iodinated contrast media, is simple, inexpensive, and has few contraindications (although allergic reactions have been rarely reported).
For all patients with suspected renal dysfunction or those considered at risk for contrast nephrotoxicity for other reasons, a baseline serum creatinine level should be obtained before the injection of contrast media.
If renal dysfunction is identified, discussion of possible alternative imaging approaches with the patient’s attending physician should be carried out. Increasing the interval between contrast media examinations and reducing the contrast dose are other protective recommendations.
Indications for serum creatinine measurement before intravascular administration of iodinated contrast media are summarized in (Table 1.3).
Table 1.3
Indications for serum creatinine measurement before intravascular administration of iodinated contrast media
History of kidney disease including tumor and transplant
Family history of kidney failure
Diabetes treated with insulin or other medications
Paraproteinemia syndromes or diseases (e.g., multiple myeloma)
Collagen vascular disease (e.g., scleroderma, systemic lupus erythematosus)
Prior renal surgery
Certain medications: metformin or metformin-containing drug combinations, chronic or high dose use of nonsteroidal anti-inflammatory drugs
Regular use of nephrotoxic medications, such as aminoglycosides
Types of Reactions
Contrast material reactions may be physiologic (nonidiosyncratic) or nonphysiologic (idiosyncratic).
Physiologic (nonidiosyncratic): Common nonidiosyncratic reactions include warmth, flushing, nausea, and a metallic taste in the mouth. Uncommon nonidiosyncratic reactions include neurotoxicity (seizure), cardiac depression, arrhythmias, renal damage, and onset of increased airway resistance.
Nonphysiologic (idiosyncratic): The cause of idiosyncratic reactions is not well known; they may possibly be related to the release of various vasoactive substances. They are not dose or concentration dependant.
Immediate and delayed anaphylactoid reactions have been reported after hysterosalpingography (HSG), secondary to resorption of contrast material from the peritoneal cavity.
CM reactions are summarized in Table 1.4 and can be classified as:
Table 1.4
Types of iodinated CM reactions
Mild
Moderate
Severe
Nausea
Tachycardia, bradycardia
Laryngeal edema
Vomiting
Hypertension
Clinically manifest arrhythmias
Cough
Pronounced cutaneous reaction
Profound hypotension
Limited urticaria
Hypotension
Convulsions
Warmth
Extensive urticaria
Headache
Dyspnea
Unresponsiveness
Dizziness
Pulmonary edema
Cardiopulmonary arrest
Shaking
Bronchospasm
Altered taste
Wheezing
Itching
Laryngeal edema
Pallor
Flushing
Chills
Sweats
Rash, hives
Nasal stuffiness
Swelling: eyes, face
Anxiety
Mild
Moderate
Severe
Organ specific