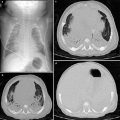
Fig. 1
Normal ventilation and perfusion scan. There is a very close match in the distribution of the tracer between the ventilation and the perfusion images. ANT anterior, POST posterior, LAO left anterior oblique, RAO right anterior oblique, LLAT left lateral, RLAT right lateral, LPO left posterior oblique, RPO right posterior oblique
2.4 Quantitative Lung Perfusion Scintigraphy
This procedure is carried out on patients with pulmonary artery stenosis to assess pulmonary arterial perfusion to each lung (Glass et al. 1991). Follow-up studies are also performed after surgery or balloon dilatation to assess perfusion. A quantitative perfusion study may also be useful after unifocalization or Fontan procedures (Fukuda et al. 2010).
The radiopharmaceutical is injected into the patient using the technique previously described. The amount of 99mTc MAA is reduced for this technique, and in infants and patients with right to left shunts, the number of particles injected should be significantly reduced (Gelfand 1978). Immediately following injection, anterior and posterior projections are acquired. The relative perfusion to each lung is calculated using comparable regions of interest on both the anterior and posterior images, using a geometric mean of the values determined from the two images. Additional oblique and lateral images are acquired as needed.
2.5 Salivagram
Initial nuclear medicine attempts to detect aspiration were accomplished by imaging the chest after administering a radiotracer labeled drink (usually milk or formula) (McVeagh et al. 1987). Although this did detect some cases of aspiration secondary to reflux, it was unable to do so if reflux was not present. The salivagram was introduced as a means of detecting aspiration secondary to disordered pharyngeal motility (Heyman 1989; Heyman and Respondek 1989).
The patient is placed in a supine position on the imaging table, beneath which the camera is positioned. The infant or child must be well restrained to minimize motion during the study acquisition. A small dosage of 99mTc sulfur colloid is placed under the patient’s tongue or in each buccal pouch and allowed to mix with the saliva. Sequential images are acquired until the activity clears from the mouth. The imaging sequence may be repeated to optimize the chance of detecting aspiration. If activity is seen anywhere in the chest area, the patient’s clothing may be removed and repeat images acquired to ensure that there is no external contamination. If activity is still seen, a lateral image of the appropriate side is acquired.
3 Clinical Interpretation: Planar Imaging and SPECT
Ventilation perfusion scintigraphy continues to be useful in the evaluation of children for the presence of pulmonary emboli. CT angiography (CTA) supplanted V/Q scintigraphy for this purpose in many institutions, in both adults and children. Evidence subsequently emerged that adult patients, who have a normal chest radiograph and no history of chronic lung disease, have a low incidence of indeterminate V/Q studies, only slightly higher than the incidence of indeterminate CTA studies (Daftary et al. 2005; Forbes et al. 2001; Jones and Wittram 2005; Eyer et al. 2005). This was also demonstrated to be true in pediatric patients as well (Gelfand et al. 2008). Depending on the CTA technique, V/Q imaging can have a lower effective radiation dose than CTA and a much lower dose to the female breast (Studler et al. 2005; Parker et al. 2005; Stabin and Gelfand 1998). For this reason, it may be preferred as the first test for evaluating suspected pulmonary embolism in children and adolescents, as long as there is no prior history of lung disease and the chest radiograph is normal or nearly normal.
Although not nearly as common in children as in adults, pulmonary embolism is increasing in incidence. This is in part due to better recognition that pulmonary embolism occurs in childhood, but, even more importantly, due to increased use of therapies that can predispose to pulmonary embolism, including the increased use of central venous access catheters. The main indication for V/Q imaging is to determine whether pulmonary embolism is present. The diagnosis is usually made according to PIOPED II and PISAPED criteria (Sostman et al. 2008; Miniati et al. 2008). However, these criteria were established for adults and have not been validated in a pediatric population (Fig. 2).
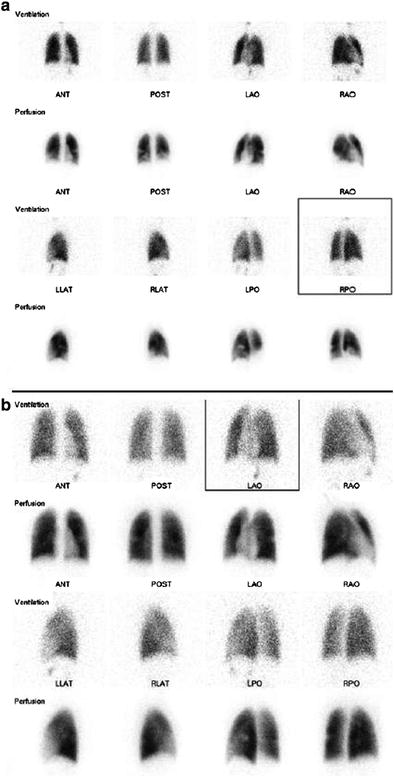
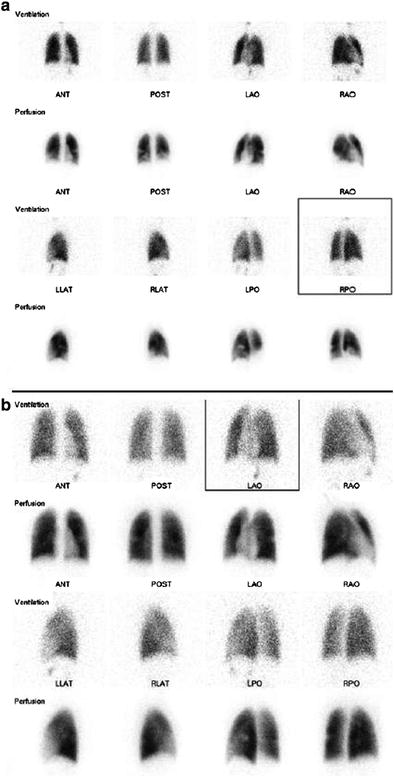
Fig. 2
Pulmonary embolism. a In the initial study, there are perfusion defects present in both lower lobes that are not present in the ventilation images. b In the follow-up study, the perfusion defects have decreased in size. ANT anterior, POST posterior, LAO left anterior oblique, RAO right anterior oblique, LLAT left lateral, RLAT right lateral, LPO left posterior oblique, RPO right posterior oblique
Lung scintigraphy can also be used to map those portions of the lung that function well. V/Q imaging may be used for this purpose, and when ventilation imaging cannot be performed, perfusion imaging alone may be adequate. With rare exceptions, in patients who do not have a history of pulmonary emboli, who are not wheezing and who are relatively free of secretions in their bronchi, ventilation and perfusion imaging are nearly identical (Hayward et al. 2007). SPECT perfusion imaging can be used to demonstrate functioning lung tissue in a tomographic format, and may demonstrate significantly more extensive perfusion abnormalities than are appreciated on planar perfusion scintigraphy, as has been shown in cystic fibrosis patients (Donnelly et al. 1997).
Quantitative perfusion imaging alone can be used to evaluate the relative perfusion to each lung or lobe due to pulmonary artery stenosis (Fig. 3) (Glass et al. 1991). The technique is especially valuable in following up the effects of intervention for the correction of pulmonary arterial narrowing. In some children’s hospitals, this is the most common indication for nuclear medicine imaging in pediatric lung disease. It should be remembered that only pulmonary arterial perfusion is evaluated after intravenous injection with 99mTc MAA. In children with a history of cyanotic heart disease, nonsegmental perfusion defects may also be due to predominant bronchial arterial perfusion to a volume of lung.
Fig. 3
Quantitative lung perfusion. Each lung is quantitated in both the anterior and posterior images
In same way that perfusion abnormalities can be evaluated in patients with pulmonary stenosis, patients with lung disease may be evaluated with ventilation perfusion or perfusion imaging to determine regional lung function after lung injury. This approach has been used in patients with bronchopulmonary dysplasia and cystic fibrosis (Soler et al. 1997). Perfusion and ventilation to each lung can also be evaluated in patients with severe scoliosis, pectus excavatum, and after repair of congenital diaphragmatic hernia (Blickman et al. 1985; Jeandot et al. 1989; Hayward et al. 2007). Congenital diaphragmatic hernia is one of the few conditions in which a patient may have a ventilation perfusion mismatch in the absence of pulmonary arterial or airway obstruction.
The diagnosis of aspiration in infants is difficult. Gastroesophageal (GE) reflux imaging and pH probe studies are done to determine whether GE reflux is present. The “milk scan” was invented to try to document aspiration after reflux (McVeagh et al. 1987). A limitation of this study is that the only aspiration detectable is that secondary to GE reflux. The salivagram is a simple study that was devised to see if saliva was being aspirated in children with pharyngeal dysfunction (Heyman 1989; Heyman and Respondek 1989). It has proved to be a very sensitive and specific study (Fig. 4).
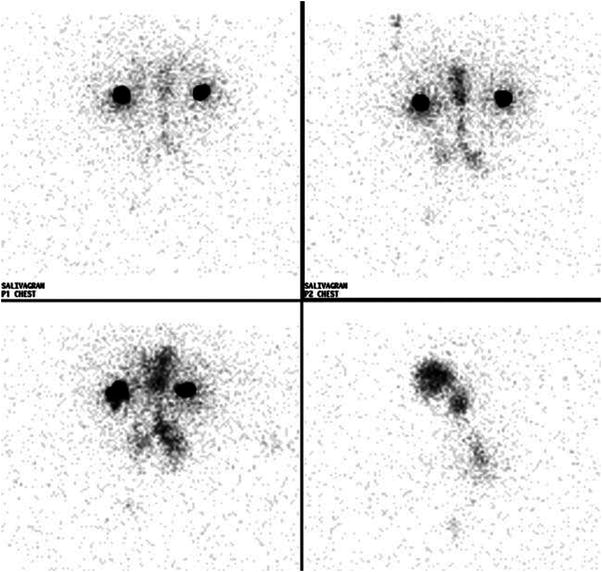
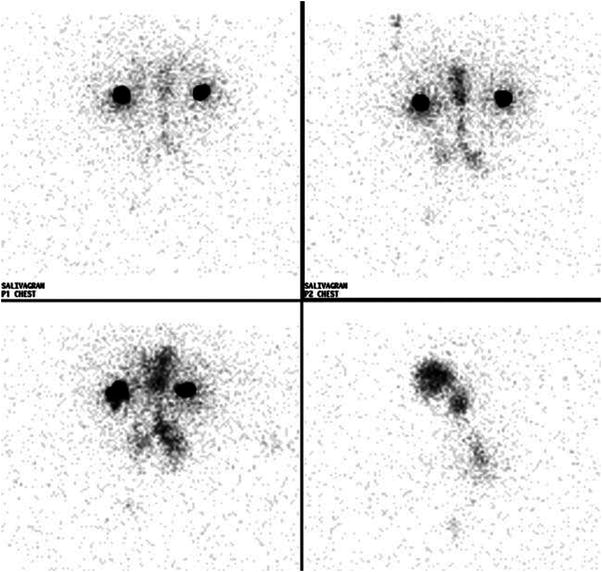
Fig. 4
Tracheal and bronchial aspiration. After swallowing of the radiolabeled saliva, some tracer entered the trachea and then entered the bronchi
4 Technique: PET and PET/CT Imaging
PET imaging is performed at a minimum of 40 min and preferably at 60 min after intravenous injection of FDG. The patient should be kept quiet at rest between the time of FDG injection and the beginning of imaging to prevent uptake in skeletal muscles that have been actively used during the FDG absorption period. All PET studies should be attenuation-corrected to avoid artifactual low grade uptake in the lungs and more prominent artifactual uptake near the skin surface; this is accomplished in older PET-only studies by measuring attenuation of the 511 keV photons using an isotopic source, and in PET/CT scanners by using the absorption data generated by the CT scan. The CT portion of the PET/CT study also provides accurate co-localization information, as long as the patient does not move between the CT and PET acquisitions. Depending on the CT acquisition parameters, the effective dose to the patient from the CT portion of a PET/CT study may be significantly less than, equal to, or greater than the effective dose from the PET portion of the study.
The techniques used for PET and PET/CT imaging of the chest are usually identical to those used for PET imaging of the rest of the body. In most cases, the PET examination of the chest is part of a study that may extend from the base of the brain either to the thighs or ankles. Key technical factors in PET imaging of the chest are mostly related to the CT portion of the PET/CT examination.
CT chest radiation exposure is typically lower than that used for the abdomen and pelvis. If the PET examination is limited to the chest, the CT exposure parameters should be appropriate for chest imaging, and lower than those used for imaging of abdomen and pelvis (with a saving in radiation dose attributable to the CT portion of the study).
The optimum position of the diaphragm for detection of pulmonary nodules on CT is during full inspiration. The PET portion of the study must be performed during tidal respiration because of the much longer duration of the PET imaging phase of the study. The best anatomic match of diaphragmatic position during a PET/CT study occurs when the CT is performed during end tidal respiration or quiet tidal respiration (Goerres et al. 2003). Pulmonary nodules are best detected when the CT is acquired at full inspiration, but there will be a significant anatomic mismatch with PET images acquired during tidal respiration (Allen-Auerbach et al. 2006; Sharp et al. 2007). It may be impossible to acquire both an optimal diagnostic CT study and an accurately co-registered PET examination at the same time. At the diaphragm, co-registration errors may be as great as 3 cm. When there is a significant anatomic mismatch between PET and CT, attenuation-corrected PET images will have artifacts that will likely adversely affect image interpretation and/or mask FDG uptake abnormalities.
Brown adipose tissue is present in children and adolescents. Exposure to a cold environment will activate sympathetically mediated nonshivering thermogenesis in brown adipose tissue, and activated brown adipose tissue utilizes not only fatty acids, but also large amounts of glucose. The cold exposure may be as subtle as a mild chill from hospital air conditioning. Avid glucose uptake in brown adipose tissue may be seen in 15–30 % of children and adolescents undergoing FDG-PET imaging. Brown adipose tissue in the neck, supraclavicular regions, axillae, and mediastinum is found immediately adjacent to many lymph node groups (Gelfand et al. 2005). Uptake in brown adipose tissue is sometimes present adjacent to costovertebral junctions and may also occasionally be seen in the upper abdomen near the kidneys. Although PET/CT should permit localization of FDG uptake to fat, this is not always possible because of small amounts of patient movement. In addition, the added sensitivity of FDG-PET in identifying tumor in some lymph nodes smaller than 1 cm is compromised when there are multiple foci of brown adipose tissue uptake in the region of the same lymph nodes (Fig. 5).