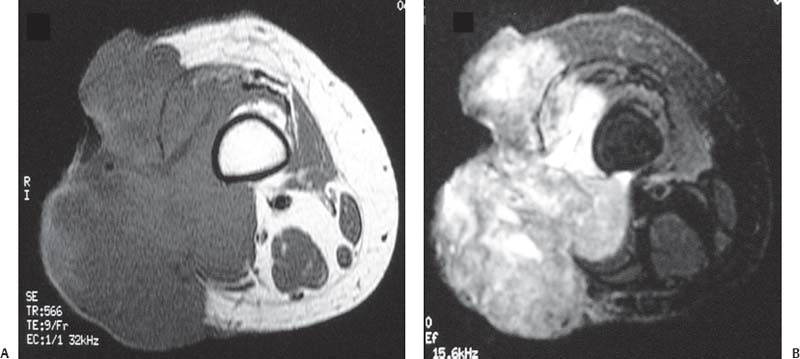
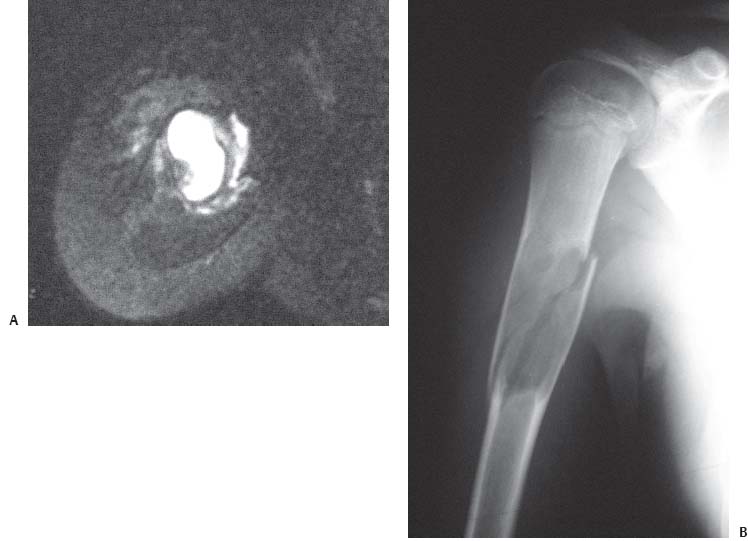
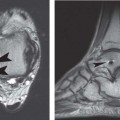
17 Correlation of MRI with Other Imaging Studies Although the preceding chapters have focused on MRI of the musculoskeletal system, it is important for the clinician to recognize that other imaging modalities play an important role in the evaluation of patients with musculoskeletal disorders. These other commonly used imaging modalities include conventional radiography, CT, nuclear scintigraphy studies, and positron emission tomography. When the clinician is evaluating the patient for a particular disease process, a basic understanding of the strengths and weaknesses of these modalities is important in deciding which imaging study to request and evaluate for the patient. For many patients, one or more imaging modalities will be superior to MRI alone. In addition, after the patient has been evaluated with an MRI study, the other imaging modalities may provide additional anatomic or physiologic information that can help narrow the differential diagnosis and guide treatment. MRI provides excellent visualization of the tissues in the musculoskeletal system in multiple planes because of its high contrast resolution compared with other modalities. One of its major advantages is that the multiple pulse sequences (see Chapter 1) enable the detection of soft-tissue and bone-marrow pathology with great sensitivity (Fig. 17.1). In general terms, an MRI study is often obtained to evaluate the water content of tissues because most acute and subacute pathology results in free extracellular fluid. MR pulse sequences use the magnetization and relaxation properties of protons to assess and differentiate various tissue types. Tissues that contain larger amounts of water (e.g., CSF or joint fluid) are bright on fluid-sensitive sequences, and tissues that contain lesser amounts of water (e.g., cortical bone or physeal scar) are dark on all pulse sequences. Structures that contain little or no water are not well assessed by MRI. For example, the lungs have a large amount of air; therefore, although MRI is an advanced technique, it is rarely, if ever, used for the evaluation of tumors and other pathology of the lung parenchyma. Cortical bone also has a low water content, and therefore MRI is relatively limited (compared with CT, for example) for the evaluation of cortical osseous structures. The preceding chapters discuss specific indications for MRI and the conditions that can be effectively evaluated using this imaging modality. As most clinicians have learned throughout their training, conventional radiographs are often the initial step in the evaluation of a patient who has (or is suspected of having) a musculoskeletal disorder. Conventional radiographs are obtained via the use of ionizing irradiation. The radiation beam is attenuated by structures between the image intensifier and the cassette. Structures with high density (e.g., cortical bone, metallic implants) block a larger amount of the radiation and thus leave a white region on the film. Structures with lower density (e.g., air, subcutaneous tissues) block less radiation and thus leave a dark or gray region on the film. Conventional radiographs are easily available and are good for the evaluation of osseous detail. This modality is also exceptionally time- and cost-effective, and the large field of view it affords allows for the study of global deformities, for example, in a patient with a spine deformity such as scoliosis or deformity or malalignment of the lower extremities. For these reasons, conventional radiography is frequently used in musculoskeletal imaging to evaluate the joints and spine (Fig. 17.2). On the other hand, conventional radiographs do not provide optimal visualization of the soft-tissue structures such as ligaments, menisci, and the spinal cord. Radiographs are also less sensitive than CT or MRI for the evaluation of osseous destruction and involvement of the bone marrow. As an example, a 30% decrease in bone mass is often required before osteoporosis can be appreciated on radiographs.1,2 Conventional radiography is the study of choice for the initial evaluation of a patient with a traumatic injury to a joint, a long bone, or the spine. Radiography is also required as an adjunct to MRI in the evaluation of skeletal masses (Fig. 17.3) and of arthritis. However, conventional radiographs are less valuable in the evaluation of a patient with low back pain, neck pain, or spinal stenosis. As a first-line imaging modality, conventional radiographs help the clinician determine the need for radiographic studies in other anatomic locations or for more advanced imaging studies of the local region. For example, a patient complaining of arm pain after trauma may be initially evaluated with humerus and elbow radiographs. Findings of an elbow fracture would then necessitate imaging of the forearm with conventional radiography to rule out associated injuries. If the fracture appeared to be intraarticular and comminuted, CT imaging may be used to study the elbow further, to delineate the fracture pattern, and to assist with preoperative planning. In another example, a patient presenting with a history of thigh pain may undergo conventional radiography to evaluate the hip, femur, and knee. If a lytic lesion were found in the proximal femur, CT would then be required to determine, more precisely, the degree of osseous destruction and to aid in characterizing the mass. MRI would also be indicated to evaluate the extent of marrow and soft-tissue involvement. Fig. 17.1 MRI: excellent soft-tissue contrast. Axial T1-weighted (A) and fat-suppressed T2-weighted (B) images of the left distal femur show a large mass involving the bone marrow and adjacent soft tissues. Note the exquisite contrast between the soft tissues provided by MRI that allows for an accurate and detailed assessment of the extracompartmental involvement of the tissues. Fig. 17.2 Conventional radiographs: visualization of local and global deformity. (A) A lateral view of the foot shows a pes planus deformity and midfoot fault in an elderly woman. This deformity may indicate the presence of posterior tibial dys-function, although assessment of the actual posterior tibial tendon is not possible by conventional radiography alone. (B) A posteroanterior radiograph of the spine shows a large right thoracic scoliosis. Fig. 17.3 Pathologic fracture through a unicameral bone cyst. (A) An axial fat-suppressed T2-weighted MR image of the right mid-humerus of a young woman shows a nodule at the periphery of a lesion occupying the humerus. The lesion is indeterminate by MRI. The diagnosis of a unicameral bone cyst with a pathologic fracture would not be possible with MRI alone; that diagnosis requires (B) a radiograph showing the specific features. Conventional radiographs are also extremely useful for the preoperative evaluation of patients undergoing orthopedic surgery. For example, in spine surgery, preoperative radiographs facilitate evaluation of spinal alignment and localization of the level of pathology. This information can then be used intraoperatively and correlated with intraoperative radiographs or fluoroscopy to confirm the operative level. CT images, which are acquired based on principles similar to those used for conventional radiography, can be considered multiplanar high-resolution conventional radiography because the radiation is transmitted through the patient in multiple planes, which permits the acquisition of a large-volume data set. Unlike conventional radiography, in which the images are acquired in one plane, this data set can be manipulated using computer software algorithms to provide images in any plane. In addition, current-generation multi-detector CT-scanning devices allow for the acquisition of very large volumes of data in incredibly small amounts of time. For example, with the development of multidetector CT, most studies can be completed in 10 seconds or less, a particularly valuable asset in the pediatric and trauma patient populations.3 With regard to its use in orthopedic surgery, CT is most valuable in the assessment of osseous detail where radiography is limited (Fig. 17.4). CT is also used secondarily to assist in characterizing disease processes in areas where the use of conventional radiography is limited, such as the sacrum and pelvic structures. Although CT does not provide physiologic information about the status of the various tissues (except for limited cases in which an intravenous contrast is used), it does provide excellent spatial resolution. This modality is particularly useful for imaging the axial skeleton and for evaluating the extent of osseous lesions.4–6
 MRI
MRI
 Conventional Radiography
Conventional Radiography
 CT
CT
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree