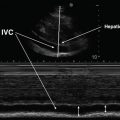
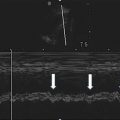
Fig. 2.1
Proposed levels of competence of echocardiography in ICU. TTE transthoracic echocardiography, TEE transesophageal echocardiography, ALS advanced life support, FEEL focused echocardiographic evaluation in life support, FATE focused assessment with transthoracic echocardiography (Reprinted from Price S, Via G, Sloth E, Guarracino F, Breitkreutz R, Catena E, et al. Echocardiography practice, training and accreditation in the intensive care: document for the World Interactive Network Focused on Critical Ultrasound. Cardiovasc Ultrasound. 2008;6:49)
Need for Universal Pathway for Certification and Accreditation
All proponents of critical care ultrasound agree that there should exist a clearly defined universal pathway for training and accreditation [2, 10]. Currently, there is no internationally recognized accreditation in general critical care ultrasound specifically for intensivists. Experts recommend that programs should be tailored specifically to intensivists, not merely replicated from the curricula for sonographers and cardiologists [6].
There are currently efforts to develop standard curriculum and program requirements, especially in the area of echocardiography [5, 11, 12]. Recently developed expert guidelines on training standards for critical care ultrasonography recommend that basic echocardiography and general critical care ultrasound be a required component of all critical care training programs. It is recommended that trainees receive a combination of didactic, computer-based, and hands-on training as part of their educational curriculum and that a logbook be kept to document competence in image acquisition and interpretation [8]. The guidelines recommend that basic training be part of regular critical care education and that physicians who desire advanced skills complete formal advanced certification programs.
Training Requirements
Basic critical care ultrasound education must balance developing an adequate knowledge of image acquisition and interpretation across a variety of organ systems, emphasizing both normal and clinically important pathology. Various educational and certification entities have begun to recognize the importance of incorporating the development of key competencies in goal-directed ultrasound for trainee physicians in emergency and critical care. In the USA, the Accreditation Council for Graduate Medical Education (ACGME) requires that all critical care medicine physicians-in-training receive education in the use of ultrasound. The 2012 guidelines require that all graduating critical care medicine fellows demonstrate competency in the use of ultrasound to place intravascular access, to perform thoracentesis, and to place intra-cavitary tubes and catheters. Graduating critical care fellows are also required to demonstrate knowledge of ultrasound in the evaluation of critically ill patients [13]. For emergency medicine residents, the ACGME requires that residents must be trained in “the use of ultrasound for the bedside diagnostic evaluation of emergency medical conditions and diagnoses, resuscitation of the acutely ill or injured patient, and procedural guidance” [14, 15]. In other countries, there is also a trend towards developing competency in critical care ultrasound as part of the educational curricula for emergency medicine, anesthesia, and critical care [3]. A major challenge is that current training requirements provide few details about how to develop competence and what specific skills are necessary.
Key Components of an Educational Program
Key components of critical care ultrasound education and training include didactic training in ultrasound physics, image acquisition and image interpretation, hands-on training, and the critical review of images and their resulting interpretation by a clinician experienced in critical care ultrasound [8].
Learning Curve
Educational efforts must recognize that there is a learning curve to developing competency in critical care ultrasound that is highly variable, and that is dependent on the specific competency that is being taught [16]. For example, a study of emergency medicine physicians found that with respect to right-upper quadrant ultrasound, image quality and clinical interpretation were significantly increased after performing seven ultrasounds, and that after 25 studies clinicians-in-training had obtained diagnostic accuracy equal to that of highly experienced providers [17]. Some skills have been shown to require little training and time to develop a high level of competency and diagnostic accuracy. In one study, critical care fellows received 4 h of didactic and hands-on training in compression ultrasonography to evaluate critically ill patients for deep venous thrombosis (DVT). The trainees then conducted 128 subsequent compression studies as part of their critical care duties and were found to have a very high level of diagnostic accuracy in diagnosing DVT compared to subsequent formal comprehensive radiology DVT studies [18]. A similar study of physicians-in-training in an academic emergency department found equally high levels of diagnostic accuracy with only a focused 10-min training session [19]. However, the development of many advanced skills, such as the ability to accurately assess subtle cardiac valvular abnormalities, requires very intensive training for an extended period of time [7].
The clinical confidence in interpreting acquired images also increases with time. A study of emergency medicine physicians who obtained certification in ultrasound found that there was a significant association between provider confidence in their image quality and interpretation in the accuracy of their diagnosis [20].
Web-Based/Computer
The use of web-based learning programs to augment hands-on and live didactic teaching in critical care ultrasound is quickly gaining popularity. Web-based education has proven to be particularly useful in helping intensivists to increase accuracy in image interpretation. A strength of web-based curricula is that they offer participants the flexibility to develop skills in image interpretation at their own pace and on their own time. In one recent study, intensivists who had completed a traditional didactic and hands-on course in critical care ultrasound were subsequently given access to a web-based learning program [21]. Completion of the web-based curriculum resulted in significant improvements in diagnostic accuracy. Clinicians also reported a significant increase in their confidence in their diagnoses after completing the web-based curriculum.
Simulation
Simulation-based medical education has the potential to greatly improve clinical knowledge and technical skills related to the use of critical care ultrasound. In one study, first-year anesthesia residents learning basic transesophageal echocardiography were randomized to traditional didactic teaching alone or to a 90-min simulator-based transesophageal echocardiography teaching session with a virtual 3-D model of a heart incorporated into a mannequin. Both groups were given pre- and post-training video-based questions pertaining to image interpretation and probe position and manipulation. While both groups showed an improvement on their post-training test scores, those that received simulation training scored significantly higher than the group that received traditional didactic training [22]. Another recent study found that the use of medical simulation with an ultrasound-compatible mannequin to train internal medicine residents in ultrasound-guided central venous catheter (CVC) placement resulted in significantly reduced rates of CVC complications and much greater reliance on ultrasonography for CVC placement compared to before the development of the medical simulation curriculum [23].
The use of medical simulation to facilitate the learning of critical care echocardiography image acquisition skills has become increasingly sophisticated in recent years. A variety of echocardiography simulators are currently available. One simulator utilizes real echocardiography data combined with a probe tip and an electromagnetic field in a mannequin (EchoCom, Leipzig, Germany) and can be used for TTE and TEE. Another medical simulator uses a digital model incorporated into a mannequin (CAE Healthcare Inc., Montreal, Canada) and can be used with TTE, TEE, and abdominal ultrasound probes. Many other simulators are available or are currently in development with varying levels of fidelity and capabilities [24].
Longitudinal Curriculum and Other Key Components
Longitudinal curricula (ongoing ultrasound education) during medical training have been shown to significantly increase both the quality of image acquisition and interpretation skills, compared to short intensive 1–3-day courses. One study of emergency medicine residents found that there was a significant increase in diagnostic accuracy after an intensive 1-month dedicated ultrasound rotation [25].
Other key components of critical care ultrasound curricula that have been identified in the literature include combining didactic teaching with equal amounts of hands-on time learning image acquisition; ongoing assessment and evaluation; and individualized review of student images by a clinician experienced in critical care ultrasound [8, 12, 26].
Incorporating Ultrasound Into an Educational Curriculum: Our Experience
Over the past several years we have developed a comprehensive ultrasound program for pulmonary and critical care fellows. First-year fellows attend a critical care ultrasound course taught by pulmonary and critical care faculty. A monthly 1-h ultrasound conference includes time for review of relevant critical care journal articles as well as image review and interpretation. Ongoing assessment of the developing skills of all fellows is conducted on an annual basis.
At our institution we also have a collegial relationship with our emergency medicine colleagues which offers further focused educational opportunities. Critical care fellows have a dedicated rotation with the emergency medicine ultrasound team. The program includes daily bedside ultrasound scanning rounds under the supervision of an experienced sonographer for instruction in hands-on skills (image acquisition) as well as recognition of normal anatomy and pathology (image recognition). In conjunction with weekly video review (open to residents, fellows, and attending physicians) there is a weekly ultrasound literature journal club to keep up-to-date with current literature as well as to review seminal articles. The video review allows junior sonographers to interpret and discuss a wide variety of normal and abnormal images with immediate feedback from advanced sonographers.
Based on our own experiences and on a review of the literature, we recommend a comprehensive approach to incorporate ultrasound into an educational training program. Key components include the following:
Introductory Didactic Course: Prior to a 2–3-day introductory course for intensivists, all participants should be given pre-course articles and course materials. Key curriculum components of an introductory critical care course include vascular access, DVT studies, pleural and lung, abdomen, and basic echocardiography. Strong consideration should be made to organizing a regional course with other programs so that resources such as faculty and ultrasound machines and standardized patients/models can be shared. Ideally, hands-on training should utilize a ratio of no greater than four learners to one instructor. Collaborating with other departments in your own institution that have a strong interest in critical care ultrasound (emergency medicine, surgery, pulmonary, anesthesia) can greatly enhance the quality of training and augment the resources available for an introductory course.
Ongoing Assessment: Ongoing assessment and training is essential. This can be initiated at the conclusion of the introductory course but should continue throughout clinical training. To assess basic technical skills at the conclusion of an introductory course, a hands-on assessment utilizing a checklist can be used to assess a trainee’s competence. To evaluate clinical knowledge, a multiple choice test requiring interpretation of ultrasound films can be used. Keep in mind that skills that are used regularly, such as vascular access, will be maintained while skills that are less frequently practiced, such as DVT studies, will be quickly forgotten by most trainees. For continued assessment of trainees throughout their clinical training we recommend assessment of both technical and clinical competence at the bedside. In addition, archiving software such as Q-path™ (Telexy HealthCare, Everett, Washington, USA) can facilitate retrospective review of a trainee’s images offsite and allow ongoing feedback. In addition, establishing a regularly scheduled ultrasound case conference for image review and interpretation of saved films can be very useful for education, ongoing assessment, and quality control.
Faculty Development: There is currently a paucity of clinical faculty in many critical care programs adept at teaching ultrasound [27]. In many programs there may be only one or two intensivists, if any, who utilize critical care ultrasound as a regular part of their clinical practice. Training programs must make a conscious effort to develop the ultrasound skills and competencies of their own faculty. Expert faculty need to focus their educational efforts not only on their trainees but also on their colleagues. Divisional “train-the-trainer” programs and ongoing quality assessment of all images acquired in ICUs can be very helpful in this regard. Most importantly, faculty need to be supported and encouraged to obtain training and utilize critical care ultrasound on a regular basis in their own clinical practice.
Core Competencies
Multiple studies have shown that time-limited and focused ultrasound education in specific targeted areas can result in the attainment of competency. It is recommended that all intensivists develop specific basic competencies in vascular, thoracic, abdominal, and cardiac ultrasound [9].
Vascular (Chap. 3)
The ability to obtain ultrasound-guided vascular access is now an essential skill for all intensivists and should be considered standard of care [9]. Critical care physicians should be educated and trained in evidence-based best practices for ultrasound guided vascular access [28]. Intensivists should also be trained to develop competency in diagnosing DVT and in visualizing the aorta and inferior vena cava (IVC) [8].
Thoracic (Chaps. 9 and 10)
The ability to use ultrasound to diagnose pleuro-pulmonary disease, including pleural effusions, pulmonary edema, and pneumothorax, should be taught to all intensivists [9]. Utilizing ultrasound to safely perform thoracentesis and chest tube placement is an important skill that should be taught to all intensivists. There is growing evidence that basic lung ultrasound can easily and accurately be adopted by providers with limited prior experience. A study of 27 French physicians found that they could accurately diagnose pulmonary edema and pneumothorax with ultrasound after completing a brief training module [29].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree