where r is the radius of aperture of the probe and f is the frequency of the beam, i.e., the wider the aperture and the higher the frequency, the longer the near field (within limits as described later).
This is important because the lateral resolution, or the ability to distinguish as separate two objects lying side by side perpendicular to the incident beam, depends on the thickness of the beam. Higher frequency beams are thinner; therefore, the image sharpness and resolution improves with higher frequency beams and in the near field rather than the far field. The divergence in the beam with increased depth causes the increased blurring of deeper structures, as two point structures appear to meld together rather than appearing distinct.
Ultrasound beams can also be focused to direct the maximum energy of the beam to the focal zone of the beam either by using an acoustic lens or by electronically shaping the beam as described below.
Types of Ultrasound Beams and Probes
A single beam of ultrasound can only image a very thin cylinder of tissue (1-D mode). If a larger rectangular section of tissue (2-D mode) is to be imaged, then multiple ultrasound beams originating sequentially from side-by-side piezoelectric elements in a linear transducer will create a parallel array of beams in a single plane. This type of transducer is typically used in vascular imaging. The width of the section imaged using a linear transducer is limited by the width or “footprint” of the linear array transducer. A curvilinear array has a curved surface with beams sent out in a diverging array allowing imaging of a larger “sector” of tissue than the linear probe, but with attendant image distortion and loss of lateral resolution for the reasons described above.
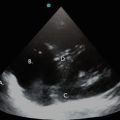
However, the need to image large sections of the thorax while retaining a footprint small enough to fit between the ribs requires a narrow array of beams originating from the center of a tiny probe being swept electronically from side to side as in conventional radar (phased array scanning). In this method, the sequential firing of the individual piezoelectric elements is infinitesimally separated in time so that Huygens’ wave interference between these individual beams deflects the entire wave front. Varying the firing sequence of these piezoelectric elements accomplishes steering of the beam from side-to-side across a sector. These are the typical probes used in thoracic and cardiac imaging. Examples of these probes are shown in Fig. 1.1.
Fig. 1.1
(a) Linear probe: typically used for imaging vascular structures. (b) Curvilinear or convex probe: this is the standard abdominal probe and scans a wide sector allowing imaging of abdominal viscera including the uterus
Electronic focusing of a beam uses the same principle by triggering outer beams before more central beams thus creating a concave, focused ultrasound front.
Ultrasound probes may be (a) moved to a different position on the surface of the body; (b) rotated along the long axis in the same position, in a clockwise or anticlockwise direction; (c) angled from side to side to obtain images in the same plane on either side; or (d) tilted back and forth to point towards or away from a deeper structure. By convention, the transducer position is on the top of the screen so that structures closer to the skin are on the top of the screen and those further from the transducer are positioned lower on the screen. Also, left-right orientation is ensured by confirming that the location of the physical ridge or button on the side of the probe corresponds to the green dot at the top of the sector scan on the image screen.
Tissue Transmission of Ultrasound Waves
Sound is a vibration propagating through a medium in longitudinal waves of compression and rarefaction. Audible sound waves in air have a frequency ranging from 20 to 20,000 cycles per second, or Hertz (Hz), whereas ultrasound waves used in clinical devices have an “ultra” high frequency of 1–10 million, or mega, Hz (MHz). Unlike lower frequency audible sounds that can be heard around corners, for example, these ultrasonic waves travel through tissue in straight lines.
Sound waves are defined by frequency (f), wavelength (λ), and velocity (v) of travel in a medium, such that v = fλ.
Thus, frequency and wavelength are inversely related to each other. The amplitude of a wave is an expression of its energy, and together with frequency, wavelength, and velocity, these four characteristics define the most important properties of sound waves.
The velocity, v, of sound in a medium is given by the equation: v = (B/D)1/2,
where B is the modulus of elasticity of the medium and D is the density. Therefore, sound generally travels faster through stiffer materials, such as bone, compared with muscle. The average velocity of sound in body tissue is 1,540 m/s, which is approximately equal to the velocity of sound in saline, or seawater. On the other hand, the resistance a material offers to the passage of sound waves through it is called its acoustic impedance, Z, and is the product of the material density and the sound velocity. Again, bone will resist the passage of ultrasound much more than soft tissue or muscle. Table 1.1 shows comparative propagation velocities of sound waves through media of different densities.
Table 1.1
Propagation velocities of sound waves in material of different densities
Medium | Velocity (m/s) |
|---|---|
Air | 330 |
Water | 1,500 |
Fat | 1,440 |
Soft tissue | 1,540 |
Muscle | 1,565 |
Blood | 1,570 |
Bone | 4,080 |
Metal | 5,090 |
When traversing tissue, sound waves can be affected in the following ways:
1.
Absorption: This is the deposition of sound energy within tissue, where it is converted to heat, diminishing any return signal back to the transducer to generate an image. Absorption is proportional to the distance of travel (path of the interrogating beam + the return path of the echo) so that deeper tissues are more difficult to image. Absorption also varies with the square of the wave frequency. This explains why low frequency waves penetrate deeper into tissue (e.g., you can “feel” the deep vibrations of a bass drum in your “bones”), but high frequency waves are only available to image superficial tissues. However, the longer the wavelength (i.e., the lower the frequency), the less spatial resolution that can be provided in a resulting image, which explains why intracellular structural detail is resolved by electron microscopes which use electron beams with an effective wavelength in the order of nanometers. Herein lies the trade-off in the use of US to interrogate biological structures—higher frequencies provide better resolution of smaller structures but can only do so relatively close to the surface of tissue, but imaging of deeper structures requires a penetrating lower frequency with resultant loss of spatial resolution and more scatter and poorer image quality (see below). Generally, frequencies of 5–10 MHz are used in clinical applications such as catheter placement in vascular structures close to the skin, whereas frequencies of 1–4 Mz are better suited to display images of heart, liver, kidneys, and other deeper structures.
Absorption is dependent too on the density of the tissue, with denser tissues absorbing more energy, and this is expressed in terms of the attenuation coefficient (in decibels/cm) of the tissue. In general [1], cortical bone (attenuation coefficient 13–26 dB/cm) absorbs more energy than muscle(attenuation coefficient 2.5 dB/cm) which in turn absorbs more energy than fat (attenuation coefficient 0.5–1.8 dB/cm), and water absorbs the least energy of the preceding structures (attenuation coefficient 0.002 dB/cm). Air has an absorption coefficient 100× that of tissue so it does not allow any transfer of energy (e.g., lung has an attenuation coefficient of 40 dB/cm). Application of a transducer over bone will prevent any sound energy reaching underlying structures, as will any air that comes between the surface of the probe and the skin. Liberal application of gel on the skin reduces reflection of sound energy at the air-tissue interface and enhances transmission of sound into the body for the imaging of viscera.
2.
Refraction: Bending of sound waves when obliquely crossing an interface of two media differing only slightly in acoustic impedance. Image brightness suffers when sound waves are bent away from the transducer, and this can also create artifacts.
3.
Diffraction: Interference patterns produced by sound waves when they encounter an obstacle.
4.
Get Clinical Tree app for offline access

Reflection: This occurs at a boundary between structures with very different acoustic impedances, such as the interface between myocardium and blood in the heart or the interface between soft tissue and bone or between solid liver tissue and bile in the gallbladder. This property of reflection is the basis for the generation of all ultrasound images.
Several factors affect how sound is reflected:
(a)
The fraction of energy reflected is proportional to the square of the difference in impedance, and is called the reflection coefficient; the remaining fraction is transmitted or absorbed. The greater the difference in the impedance between tissues, the more incident sound energy is reflected back to the transducer for image production. The acoustic impedance of various body tissues is listed Table 1.2 [2].
(b)
The amount of energy reflected back to the transducer also depends on the angle of incidence of the sound beam at the tissue boundary. Structures that lie perpendicular to the ultrasound beam will reflect the most energy back to the transducer—the greater the inclination of the beam away from the perpendicular, the more the echo will be reflected away from the transducer. This explains drop-out artifacts when imaging moving structures, e.g., cardiac valves, and also why a valve leaflet may appear bright white when it moves into view at right angles to the interrogating beam. This must not be confused with calcification of the leaflet!
(c)




Size and surface properties of the boundary: reflection from a smooth or specular interface sends most echoes back to the transducer giving a bright image, whereas scattering from rough surfaces sends echoes in all directions, reducing the energy returning to the probe for image acquisition (Fig. 1.2). Specular reflections arise from objects much larger than the wavelength of the incident beam, and are useful in delineating tissue boundaries such as the surface of the gallbladder or the outline of cardiac chambers. Objects that are smaller than the wavelength of the interrogating beam produce scattered waves (particularly prominent with low frequency probes) that are subsequently reflected by surrounding tissue back to the probe and provide the granular “background noise” or “speckles” on the image. Scatter provides information about the structure of the tissue rather than the interface or boundary and so this property of “speckling” is harnessed in tissue harmonic imaging of the myocardial tissue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree