Fig. 14.1
(a) Curvilinear probe, (b) phased array probe
The target patient population for the eFAST exam is any patient with a history of blunt or penetrating thoracoabdominal trauma and/or any patient with unexplained hypotension or shortness of breath in a known or suspected trauma. Other accurate modalities exist for detecting pathologic thoracoabdominal free fluid, such as computed tomography, but ultrasound is ideal in that it may be performed at the bedside of the unstable patient for whom transport to radiology poses too great a risk. Previous gold standard diagnostic methods, such as peritoneal lavage, have an extremely high sensitivity for detecting abdominal free fluid (98 %) [8], but pose the risk of exposing the patient to a nontherapeutic laparotomy [9]. For this reason, their use in practice has waned in favor of less invasive methods [10]. Both morbid obesity and the presence of subcutaneous air dramatically reduce the sensitivity of the FAST exam. Patients with these conditions should be approached with caution when the suspicion for the presence of abdominal or pericardial free fluid is high. One method of increasing the sensitivity of the FAST exam is placing the patient in the Trendelenburg position, a feasible maneuver as most trauma patients arrive supine with cervical spine immobilization [11]. Further limitations of the FAST exam will be discussed later in the chapter.
Image Acquisition and Interpretation
The traditional FAST exam is performed with a goal of obtaining three views of the abdomen and a single view of the pericardial space, or four views in total:
1.
Right upper quadrant (RUQ) or Morison’s pouch/hepatorenal space
2.
Left upper quadrant (LUQ) or splenorenal space
3.
Pelvic view
4.
Subxiphoid or other pericardial view
The exam addresses the focused question of whether free fluid is present in the abdomen and/or pericardium. Some authors have traditionally taught that the first view acquired is the subxiphoid or other pericardial view, with a goal of allowing the operator to adjust the gain based on the appearance of intracardiac fluid. Our current discussion will focus on the patient with blunt or penetrating abdominal trauma, for whom the first view obtained should be that of the most dependent space in the peritoneum, known as Morison’s pouch.
A discussion of orientation is important, as this component of ultrasonography may be difficult for the novice and is crucial for accurate image interpretation. Figure 14.2 illustrates the relationship between the probe marker, the orientation mark on the screen, and the operator. Understanding that the probe uses a credit card thin beam to create a two-dimensional image from three-dimensional structures takes some practice; one analogy used is that of “shining a flashlight in a dark room.” What is visible on the screen is only that which is present in the probe beam’s path; once the beam moves beyond the object, the image is no longer visible, but it does not mean that the object does not exist.


Fig. 14.2
The yellow star denotes the corresponding direction between the screen, the probe, and the operator
Varying clinical circumstances and space availability hinder the practice of performing the FAST exam on a dedicated side of the patient and require flexibility on the part of the operator. Therefore, while the exam may be performed from either side of the patient and with either hand, depending on the operator’s comfort, the image planes should remain consistent. Images will then be dutifully replicated with attention to marker consistency and operator orientation to patient. We recommend one-handed scanning, whether right or left, with the operator’s other hand free to adjust the gain, depth, and other components of the image. All images should be obtained by the operator from the same side of the patient, with skilled ultrasonographers dividing their attention among the screen, the probe, and the patient as needed.
Due to its higher specificity than sensitivity the FAST exam is suited for use only as a screening tool for thoracoabdominal free fluid, and should be interpreted accordingly – negative exams should be regarded with caution. Trauma patients with abdominal pain and an absence of abdominal free fluid on ultrasound should be observed with serial exams and undergo a repeat ultrasound or be further evaluated with an additional imaging modality such as CT scan [12].
RUQ View
Each patient will bring unique anatomic characteristics to the clinical scenario; thus, accurate images will be obtained using slightly different movements each time. A starting point for the RUQ view begins at the intersection of the anterior- to mid-axillary line and the horizontal subxiphoid line or at the seventh to tenth intercostal rib spaces on most patients (Fig. 14.3). The probe marker is oriented toward the patient’s head, and the image created is a coronal plane. The lateral aspect of the body correlates with the near field of the image, while the far field of the image demonstrates medial structures. In other words, Images at the top of the screen represent structures closest to the skin’s surface, and images at the bottom of the screen represent structures deeper in the body. Recognizing that the ribs run obliquely across the body, the probe may be rotated slightly so that the thin ultrasound beam is able to penetrate through the narrow rib space. Figure 14.4 demonstrates the normal RUQ FAST view. Visible here is the normal homogenous, echogenic liver, the hyperechoic (compared to liver, which serves as the reference for echogenicity) renal medulla, the hypoechoic renal cortex, and the hyperechoic diaphragm. Morison’s pouch, the most dependent space in the peritoneum and the potential space between the liver and the right kidney, is the visual zone on which the operator should focus, searching for a hypo- or anechoic area between the two organs which represents free fluid (Fig. 14.5). Vigilance must be maintained to ensure that the entirety of Morison’s pouch is evaluated, lest a small amount of free fluid “hide” near the inferior portion of the liver. Visualization of the inferior pole of the right kidney is an effective way to do this. After the liver, the superior pole of the right kidney, and the bright respirophasic diaphragm are visualized, the probe may be slid caudally to reveal the kidney’s inferior pole. Figure 14.6 demonstrates how free fluid may be missed in absence of attention to this fact.

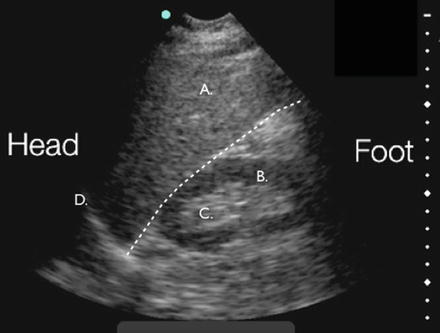
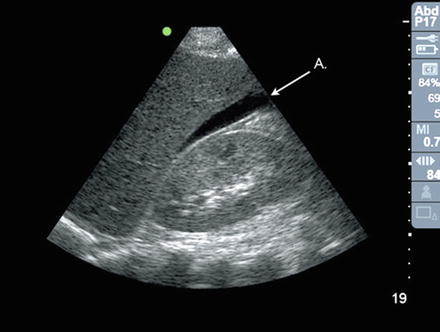
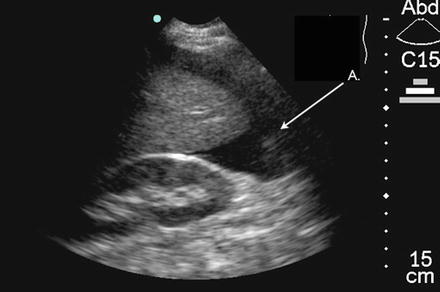

Fig. 14.3
Probe position for RUQ view. The marker is oriented toward the patient’s head
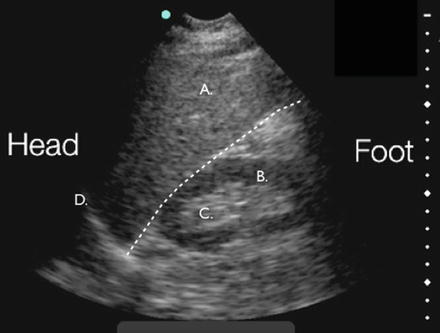
Fig. 14.4
A normal RUQ view. A liver, B renal cortex, C renal medulla, D diaphragm. Note the dashed line indicating the potential space between the echogenic liver and hypoechoic renal cortex, or Morison’s pouch
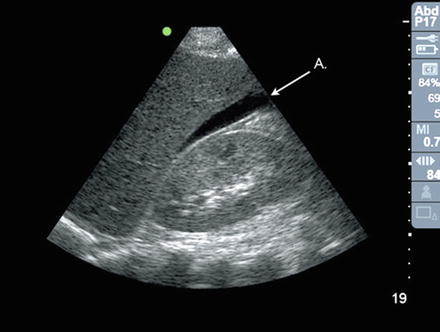
Fig. 14.5
A Free fluid in Morison’s pouch, indicated by the black, or anechoic stripe of fluid in the hepatorenal space
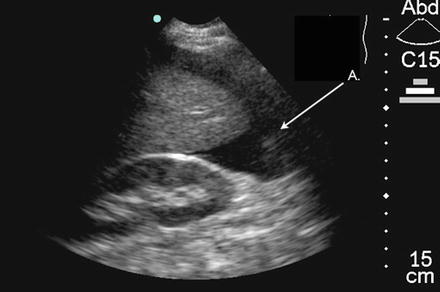
Fig. 14.6
A Free fluid in the RUQ at the inferior kidney pole, which may be missed without a complete survey of the right kidney
LUQ View
The splenorenal space is visualized in similar fashion to Morison’s pouch, with the probe marker toward the patient’s head and the probe placed in the horizontal subxiphoid line, with the corresponding intersecting line as the middle to posterior axillary line (Fig. 14.7). The smaller size of the spleen provides less of an acoustic window than the liver, and the more posterior position of the left kidney requires positioning adjustment. A direction frequently given to trainees standing on the right side of the patient performing this component of the FAST exam is to put their “knuckles on the stretcher,” extending the probe-holding hand posteriorly enough to orient the probe beam in a retroperitoneal direction, which will adequately visualize the splenorenal space. Figure 14.8 demonstrates the normal LUQ view; note the echogenic spleen, left kidney, and diaphragm. Because the phrenicocolic ligament creates a barrier to the splenorenal space, fluid generally accumulates in the subphrenic space prior to the splenorenal space. For this reason, attention should be paid to adequately visualize the border of the spleen and diaphragm, where free fluid may be missed (Fig. 14.9). After this, the search for free fluid continues to the splenorenal space (Fig. 14.10).

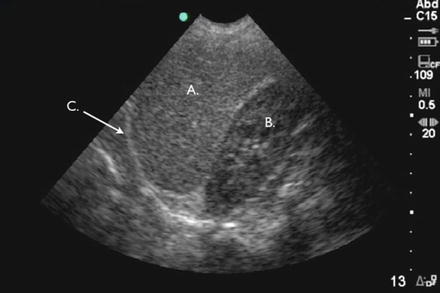

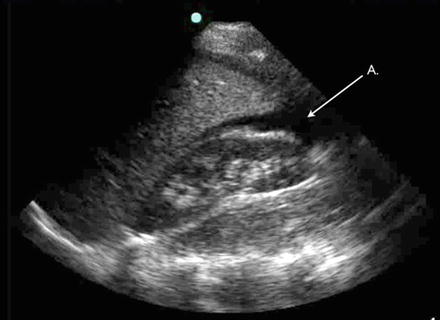

Fig. 14.7
Probe position for the LUQ view. The probe marker is oriented toward the patient’s head
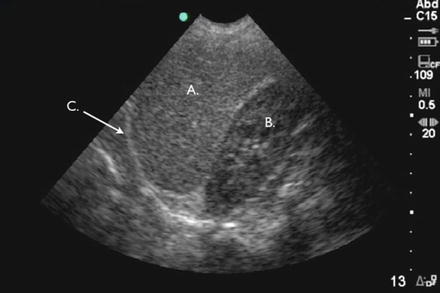
Fig. 14.8
Normal LUQ view. A spleen, B left kidney, C diaphragm

Fig. 14.9
A Free fluid in LUQ in subdiaphragmatic space, B spleen, C diaphragm. Fluid accumulates here before the splenorenal recess due to the phrenicocolic ligament
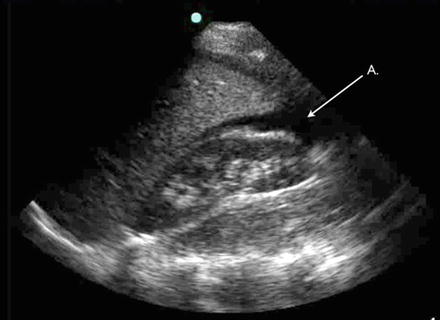
Fig. 14.10
A Free fluid in splenorenal recess
Pericardial View
Due to the anatomic position of the heart, penetrating trauma to the chest wall often injures the right ventricle. The classic pericardial image obtained in a FAST exam is that of a subxiphoid image. On initial positioning, the probe marker is on the patient’s right, and the probe itself is aimed toward the patient’s head or slightly toward the patient’s left shoulder (Fig. 14.11). An overhand grip of the probe is encouraged here, as the probe must be angled closely to the body to provide an adequate view into the thoracic space, and an underhand grip may inhibit this. The normal subxiphoid view of the heart uses the liver as an acoustic window and demonstrates the hyperechoic pericardium and cardiac septum and the four anechoic chambers of the heart (Fig. 14.12). The border of the liver and the right side of the heart, found in the near field of the image, is the focal zone in the search for anechoic fluid (Fig. 14.13). In some cases, the subxiphoid view may not be attainable either due to cutaneous abdominal or chest trauma or patient anatomy (e.g., those with a long thoracic cage or narrow subxiphoid space). An alternative view in the search for pericardial free fluid is the parasternal long view. Teaching varies in regard to screen and probe marker orientation, but probe placement is consistent in that it is placed in the left mid-clavicular line at the second through fourth intercostal space, in plane with a sagittal cut through the heart. Care should be taken to decrease the depth of the image, as the parasternal long heart is much more shallow than the subxiphoid image previously described. Obtained is the image seen in Fig. 14.14; visible is the left atrium and ventricle, the aortic outflow tract, the right ventricle, and the descending thoracic aorta in cross section. This last structure is crucial, as the anechoic stripe seen in Fig. 14.15 between the descending thoracic aorta and the posterior pericardium represents pericardial fluid, whereas Fig. 14.16 also shows an anechoic stripe of fluid, but its location behind the descending thoracic aorta indicates that this is a pleural effusion or hemothorax. Further discussion of echocardiography is available in Chaps. 5, 6, and 7. We will discuss the search for fluid above the diaphragm in the description of the eFAST exam in the “advanced competencies” section of this chapter.

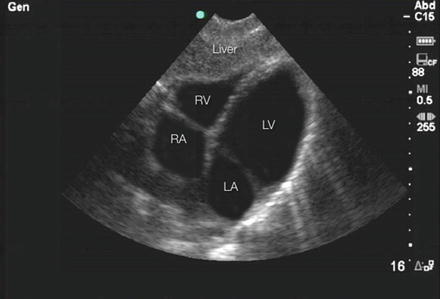
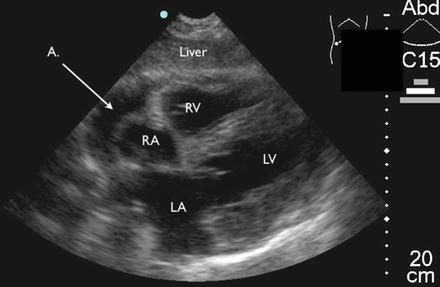
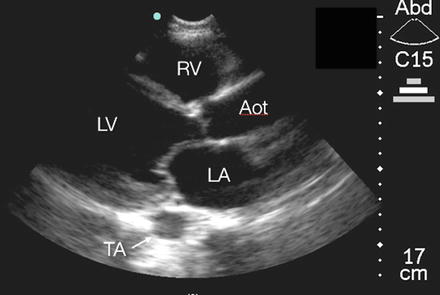
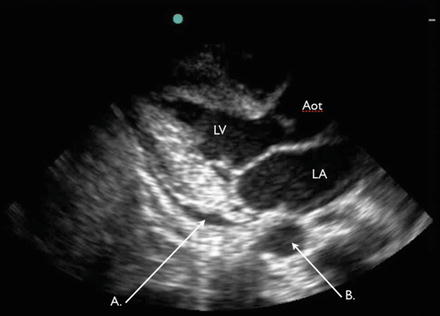
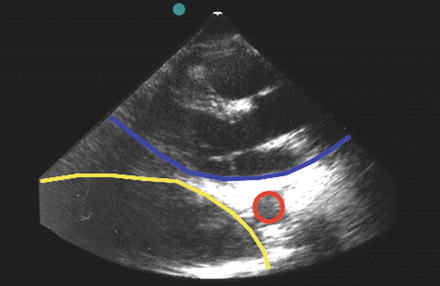

Fig. 14.11
Probe position for the subxiphoid view. The probe marker is toward the patient’s right side. An overhand grip is used to flatten the probe against the xiphoid process
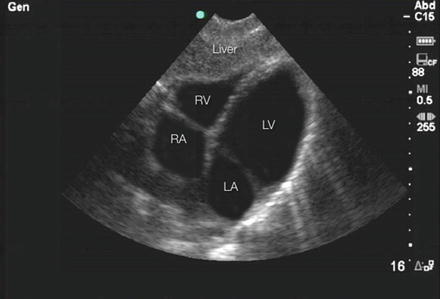
Fig. 14.12
Normal subxiphoid view of the heart. RA right atrium, RV right ventricle, LA left atrium, LV left ventricle
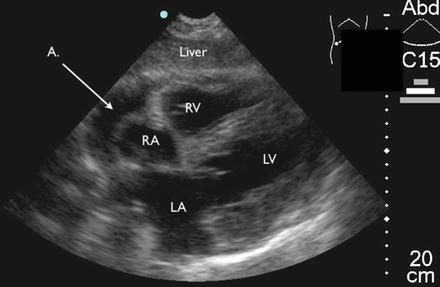
Fig. 14.13
Subxiphoid view of fluid in pericardium. The liver is used as an acoustic window to visualize the echo-free stripe of fluid (A) shown between the liver and right side of the heart
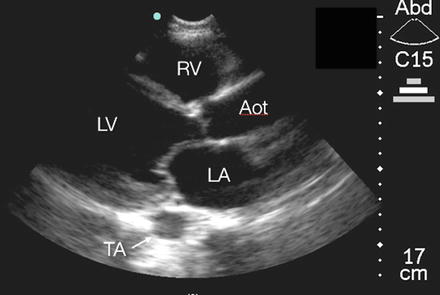
Fig. 14.14
Normal parasternal long view. LA left atrium, LV right ventricle, RV right ventricle, Aot aortic outflow tract, TA descending thoracic aorta in cross section
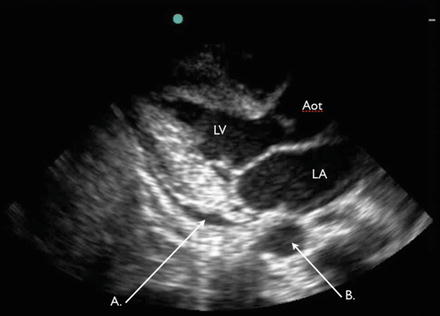
Fig. 14.15
Parasternal long view with pericardial fluid. Note the location of fluid (A) between the descending thoracic aorta (B) and the posterior pericardium, indicating that the effusion is pericardial
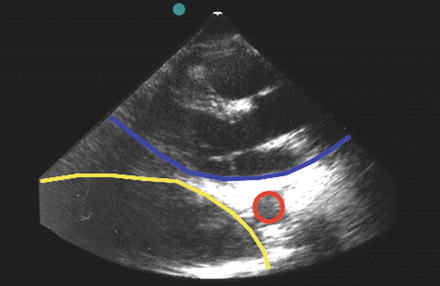
Fig. 14.16
Parasternal long view with pleural fluid. Note the location of fluid (yellow) behind the descending thoracic aorta (red), rather than the pericardium (blue), indicating that the effusion is pleural
Pelvic View
The pelvic view is obtained by placing the probe in the midline just superior to the symphysis pubis, angled 30° caudal with the probe marker toward the patient’s right side; this provides an axial view of the bladder. An additional view is obtained by placing the probe in the same location and position with the probe marker oriented toward the patient’s head; this provides a sagittal view (Fig. 14.17). In the axial view, the probe is fanned cranially and caudally, visualizing the superior and inferior portions of the bladder and, in women, the uterus in cross section (Fig. 14.18). In the sagittal view, the bladder and uterus are visualized in sagittal or long-view (Fig. 14.19). In women, the search for fluid should include the space posterior to the bladder and uterus, and among loops of bowel. In men, views should include the posterior bladder and anterior rectal space. The paired, hypoechoic seminal vesicles may be noted posteriorly to the bladder. In contrast to the pericardial view just obtained, adjustments of both gain and depth are often necessary to obtain a satisfactory search for pelvic free fluid. If the preceding view obtained was of the subxiphoid heart, minimal depth increase may be needed. However, if the image obtained was that of the parasternal long heart, a depth increase will likely be required to properly search for pelvic free fluid. A full urinary bladder provides an excellent acoustic window through which pelvic free fluid may be visible (Fig. 14.20). Posterior enhancement, an artifactual phenomenon which causes structures deep to an area of anechogenicity to appear bright, may result in a need for gain adjustment. A greater challenge is the patient with an empty bladder who lacks an acoustic window through which free fluid may be visible. Gain adjustment may be necessary in this scenario to find small pockets of anechogenicity among the surrounding structures. Free fluid located adjacent to the bladder may also be indicative of traumatic bladder rupture, especially in the patient with gross hematuria and suprapubic abdominal trauma or a high clinical likelihood of pelvic fractures [13].

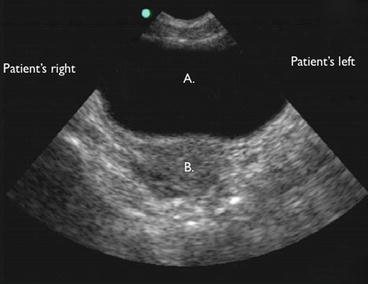
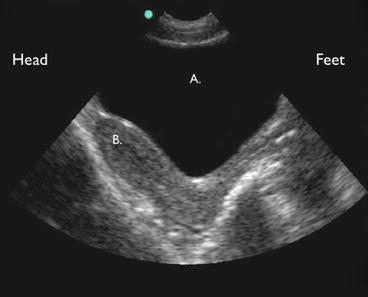
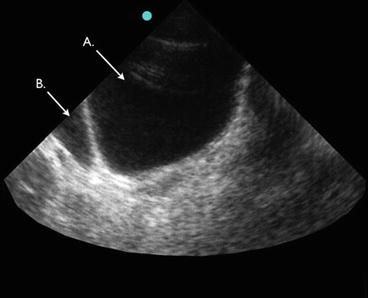

Fig. 14.17
Probe position for pelvic view. The left image shows the probe marker oriented toward the patient’s head, producing a sagittal pelvic view. The right image shows the probe marker oriented toward the patient’s right side, producing an axial pelvic view
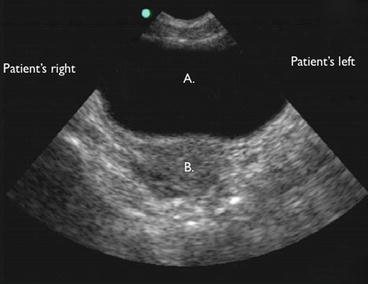
Fig. 14.18
Normal transverse view of the female pelvis with the anechoic bladder in the near field (A) and the uterus in the far field (B). The probe is oriented so that the marker is pointed toward the patient’s right
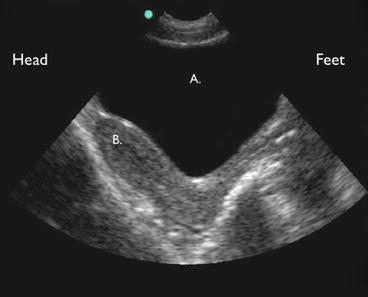
Fig. 14.19
Normal sagittal view of the female pelvis. Again seen is the anechoic bladder in the near field (A) and the uterus in the far field (B). The probe is oriented so that the marker is toward the patient’s head
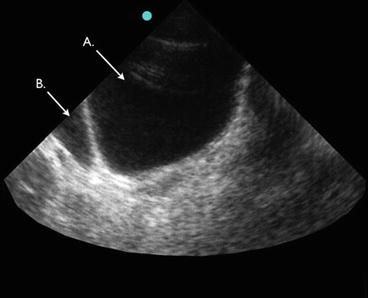
Fig. 14.20
This transverse view of the bladder (A) shows a small area of free fluid (B) on the left side of this image, which is the patient’s right side
Basic Competencies
The FAST exam is approached from the standpoint of whether or not free fluid is present in the peritoneal or pericardial space. As described above, while free fluid in Morison’s pouch may be easily noted by an experienced sonographer, free fluid in other locations such as the pelvis or LUQ may be more difficult to visualize and will require careful technique. Once the exam is performed, the appropriate use of the information gained is crucial. Figure 14.21 illustrates an algorithm for use of the FAST exam in the setting of blunt abdominal trauma, with the hinge point for action resting on hemodynamic stability. In the hemodynamically unstable patient with a history of trauma and free fluid visible on FAST exam, operative management is indicated. A notable and complex exception here is the patient with a past medical history significant for ascites (e.g., patients with a history of liver disease, cancer, or dialysis). These patients may also have a baseline low blood pressure, and this clinical information must be integrated into their management. One solution is a brief and small volume diagnostic paracentesis, using ultrasound in real time or for marking the fluid’s location. If straw-colored fluid is retrieved, clinical management may be redirected accordingly; if blood is obtained, the pathway described above stands [14].
Fig. 14.21
Blunt abdominal trauma algorithm
In the hemodynamically stable patient, some trauma and critical care providers may elect to perform a FAST exam; others may not. However, as systemic hypotension has been validated as a late marker of shock [15], we recommend the FAST exam for all patients with a history of blunt abdominal trauma as long as it does not interfere with the primary/secondary survey. The stable patient with a positive FAST exam may be directed for expedited CT; the stable patient with a negative FAST exam may be managed with serial exams, CT as indicated, or observation. The unstable patient with a negative FAST exam and a history of blunt abdominal trauma is one who requires clinical problem solving on the part of the providers. Has the patient suffered a long bone injury and lost blood into an extremity? Was blood loss significant enough on the scene of the event that tachycardia and/or hypotension has resulted? Is there another cause of shock that must be considered given the patient’s medical history? In these cases, resuscitation is continued and the FAST exam may be repeated as needed. A trauma patient for whom immediate operative management is indicated based on primary/secondary survey alone is a patient for whom management should never be delayed for purposes of ultrasound examination. In such cases, the FAST exam does not add any information that will help guide patient management further, and therefore should not be performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree