Regional
Immediate
Inadvertent arterial puncture
Hematoma
Pneumothorax
Hemothorax
Catheter malposition
Air embolism
Arrhythmias
Thoracic duct injury (left neck)
Brachial plexus nerve injury
Late
Lumen occlusion
Venous thrombosis
Arteriovenous fistula
Exit-site infection
Systemic
Catheter-related bloodstream infection (CRBSI)
Table 3.2
Advantages of ultrasound-guided central venous access
Increased cannulation success rate |
Increased first-attempt success |
Decreased complication rate |
Detection of anatomical variation |
Detection of thrombosis |
Optimal vessel selection (e.g., internal jugular, subclavian, femoral vein) |
Confirmation of catheter site |
Rule out complications (e.g., pneumothorax) |
Traditional sites for central venous access are the internal jugular, subclavian, and femoral veins. Additionally, over the past decade, peripherally inserted central catheters (PICC) have gained popularity and have been increasingly used in patients needing prolonged central venous access. Ultrasound guidance has been used to augment successful placement of peripheral intravenous lines and arterial catheters – especially in patients with difficult anatomic landmarks or in the very young.
Technical and Patient Considerations
Vein Selection
A pre-procedural scan is strongly recommended to guide the selection of an optimal target vessel [6]. Criteria that favor the selection of a vein are:
1.
Vessel patency (venous collapse during breathing or compression without signs of thrombosis)
2.
Easy accessibility (measure the distance between the skin surface and the vessel wall)
3.
Diameter (vessel size less than three times the caliber of catheter may carry a greater risk for thrombosis) [7].
4.
Anatomical variation
5.
Intended purpose (i.e., neck surgery often requires infra-clavicular vascular access)
6.
Intended duration for catheter placement
Complication rates after the implementation of landmark techniques differ between sites. The internal jugular vein carries the highest risk of accidental arterial puncture and hematoma, the subclavian carries the highest risk for pneumothorax, hemothorax, and catheter malposition, while the femoral vein carries the highest risk for thrombosis and infection (Table 3.3) [1, 5, 8]. The 2011 Guidelines for the Prevention of Intravascular Catheter-Related Infections recommends the use of the subclavian vein site (rather than internal jugular or femoral veins) in adult patients to minimize the risk of infection. However, the aforementioned guidelines were based on data obtained prior to the introduction of standardized insertion bundles and modern anti-infective techniques such as the use of chlorhexidine gluconate (CHG) dressing devices. Recent studies show that CHG-impregnated sponge dressing when used with the standard care decreases the incidence of major catheter-related infections from 1.4 to 0.6 per 1,000 catheter-days [9].
Table 3.3
Complication rates in different central veinsa
Complication | Internal jugular [1] | Subclavian [8] | Femoral [5] |
|---|---|---|---|
Arterial puncture % | 10.6 | 5.4 | 6.25 |
Hematoma % | 8.4 | 5.4 | – |
Pneumothorax % | 2.4 | 4.9 | – |
Hemothorax % | 1.7 | 4.4 | – |
Malposition % | – | 11 | – |
Infection (rate per 1,000 catheter-days) [5] | 8.6 | 4 | 15.3 |
Thrombosis (rate per 1,000 catheter-days) [5] | 1.2–3 | 0–13 | 8–34 |
Pre-procedural Preparations
Selection of probe: a high-frequency (10–15 MHz) linear probe (Fig. 3.1) is commonly used for UGVA, while low frequency curved-array probes (Fig. 3.2) are reserved for vessels that might be located deeper than expected for various reasons (i.e., obese patients, subcutaneous edema, anatomical anomalies, etc.). Hockey-stick probes bearing smaller footprints are oftentimes used in pediatric patients and in neonates (Fig. 3.3).

Fig. 3.1
A high-frequency linear probe is commonly used for vascular scanning

Fig. 3.2
A low-frequency convex probe can be used to scan vessels located at greater depth from the skin surface as low-frequency enhances the deeper penetration of the ultrasound beam

Fig. 3.3
A hockey-stick probe combines high-frequency scanning with a smaller footprint and is commonly used in pediatric patients
Sterile techniques should be followed in all cases: hand washing, full sterile barrier protection, sterile probe cover and gel (Figs. 3.4) [6].

Fig. 3.4
A standard central venous access kit and ultrasound probe with a sterile cover
The ultrasound machine should be positioned opposite to the operator to facilitate direct and straightforward visualization of the screen (Fig. 3.5).

Fig. 3.5
The ultrasound machine is positioned opposite to the operator to facilitate direct and straightforward visualization of the screen in this supraclavicular cannulation of the right subclavian vein
Tips to Differentiate Veins from Arteries
Shape: arteries tend to be circular and veins elliptical.
Size: the vein is usually larger than the adjacent artery and increases in size with Trendelenburg positioning.
Compressibility: veins are easily compressible.
Color flow fills venous lumen completely (color mode).
Normal central venous flow on Doppler mode demonstrates spontaneity, phasicity, and augmentation.
Procedure Checklist and Bundle
The American Society of Anesthesiologists Task Force on Central Venous Access recommends the use of a central line insertion work and safety checklist and bundling of required equipment to minimize errors, risk of infection, and complications [10]. These simple measures (Pronovost’s checklist) have shown tremendous reduction (up to 66 %) in central line-associated bloodstream infections (CLABSIs) [11].
Image Acquisition and Interpretation
A few practical tips when performing an ultrasound-guided central venous cannulation for the first time include:
Always adhere to a strict sterilization process by implementing a sterile probe cover and sterile gel as previously mentioned.
Initially, avoid pressing too hard with the probe on the cannulation site as normal veins are collapsible vessels (Fig. 3.6).
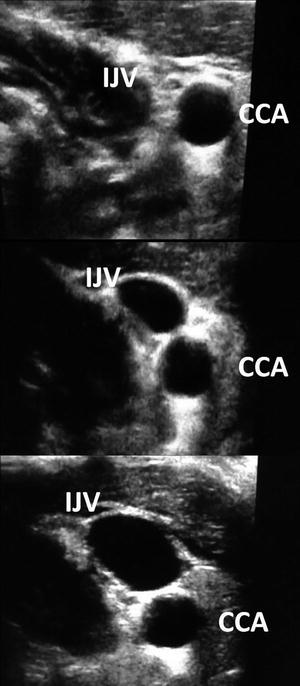
Fig. 3.6
Applying full probe pressure this patent internal jugular vein (IJV) which accompanies the common carotid artery (CCA) in the left lateral neck fully collapses and vanishes (top) while using less (middle) and light (bottom) probe pressure the vein gradually reappears until it reaches its full size (bottom)
Optimize the two-dimensional image: center the image on the screen and adjust depth, gain, and focus, while obtaining the proper orientation of anatomy with standardization of the dot on the left.
Once the two-dimensional image of the vein is obtained, check its patency by applying probe pressure to exclude thrombosis (Video 3.1).
Two-dimensional ultrasound can demonstrate either a short-axis view (a transverse view of the vessels) or a long-axis view (a longitudinal view of the vessels). The longitudinal axis view allows for continuous visualization of the needle trajectory and reduces the risk of posterior wall puncture. However, it requires advanced procedural skill and experience to synchronize the needle trajectory within the real-time ultrasound image. When using color-Doppler mode, operators should interpret the generated color (blue or red) dependent on probe orientation. Flow directed towards the probe will generate a red shift and flow directed away from the probe will generate a blue shift. Thus, red and blue shades in color flow do not necessarily represent the respective artery and vein but the direction of flow towards or away from the probe.
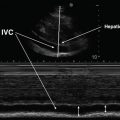
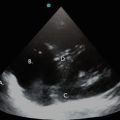
Pre-procedural scanning: detection of vessel size and patency and exclusion of possible thrombosis (Fig. 3.7). Notably, pre-procedural lung ultrasound should also be performed to exclude pneumothorax (Fig. 3.8) and thus confirm the presence of a normal aeration pattern.
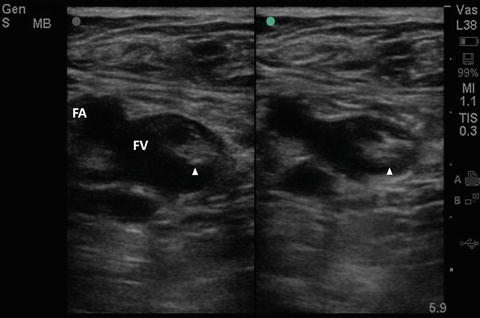

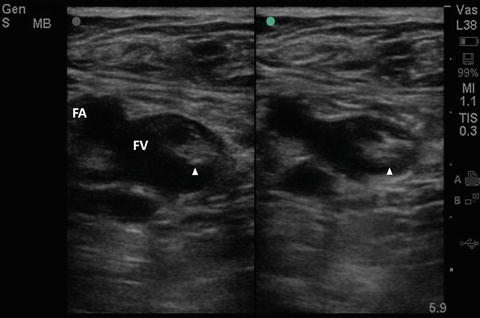
Fig. 3.7
Femoral vein thrombosis: Compression with the probe fails to collapse the vessel. FA femoral artery, FV femoral vein, Arrow head denotes thrombus

Fig. 3.8
Depiction of the barcode sign (indicative of pneumothorax) on M-mode in a patient’s left anterior chest (mid-clavicular line) prior to cannulation
For obvious reasons, catheter insertion should not be attempted when a preexisting clot exists in the target vessel. It is essential to scan the latter prior to catheterization to exclude thrombosis, especially in ICU patients. Notably, 90 % of potential thrombi originate from the femoral-popliteal system; however, upper extremity deep venous thrombosis may also occur in ICU patients. In a cohort of critical care patients, Blaivas et al. reported an incidence of upper extremity deep vein thrombosis around 11.25 % [12]. Risk factors included central venous catheter-associated thrombosis, malignancy, total parenteral nutrition, hypercoagulable states, and obesity (body mass index or BMI ≥35 kg/m2).
Ultrasound signs of venous thrombosis include lack of complete vein compression, presence of intraluminal echoes (although acute thrombus can be echolucent), decrease or absence of color flow. Also, venous Doppler demonstrates decreased or absent spontaneity, phasicity or augmentation and either dilated or contracted veins (Fig. 3.9). The sonographic detection of thrombosis aids in the diagnosis of catheter-related infections [13].
Fig. 3.9
Normal venous flow is spontaneous (automatically heard with Doppler), phasic (flow increases and decreased with respiration), and augmented (increased with distal compression). Although normal Doppler signs may be present with partially occlusive thrombosis, the usual Doppler findings include: absence of spontaneity (no venous flow) indicating venous obstruction, continuous flow indicating proximal obstruction or extrinsic compression, while distal compression does not produce augmentation. Note the flow augmentation in a normal brachial vein that has been compressed distally (a) and the spontaneous, phasic flow occurring in a normal subclavian vein (b). Observe the absence of flow in a totally thrombosed internal jugular vein (c) and continuous flow in an extrinsically compressed internal jugular vein (d)
Basic Competencies
Operators who perform ultrasound-guided placement of central venous catheters should be familiar with the sonoanatomy of the cannulation site and possess basic ultrasound skills such as the ability to differentiate between arteries and veins, detect venous thrombosis, and select the optimal vessel for cannulation. We recommend using real-time techniques where the operator moves the probe and needle slowly, in a simultaneous fashion, to ensure that the needle tip is visualized continuously [6]. This technique can be performed by a freehand approach or by the implementation of needle guides which keep the needle attached to the plane of the probe at all times. The former approach is technically demanding as it depends largely on the fine coordination of probe positioning and needle movement; however, it allows a great degree of freedom in maneuvers and adjustments of the penetrating needle trajectory (Figs. 3.10 and 3.11).



Fig. 3.10
Freehand access cannulation of the internal jugular vein on the long axis requires fine coordination of movements (note that the plane and trajectory of the needle follows the plane of the probe)

Fig. 3.11
Freehand access cannulation of the internal jugular vein on the short axis is relatively easier compared to the long-axis approach. However, needle visualization on the short-axis approach is more problematic (note that the angle of the penetrating needle is around 40–45°)
Internal Jugular Vein Cannulation
Anatomy
The internal jugular vein drains blood from the brain, face, and neck. It begins at the jugular foramen in the skull, merges through the carotid sheath (along with the common carotid artery medially and vagus nerve posteriorly), and joins the subclavian vein behind the medial end of the clavicle to form the brachiocephalic vein. Rotating the head will lead to overlapping of internal jugular vein with the common carotid artery. The thoracic duct ascends on the left side of the neck along the left margin of the esophagus until C-7, where it bends laterally behind the carotid sheath and then turns down again to drain into the left brachiocephalic vein [14].
Procedure
A high-frequency linear transducer is placed over the groove between the sternal and clavicular head of the sternocleidomastoid muscle at the lateral side of the neck (Figs. 3.10 and 3.11). Pre-procedural scanning is performed to identify the adjacent structures and evaluate the vein’s depth, caliber, and patency (Figs. 3.12, 3.13, and 3.14). Electrocardiogram monitoring is necessary to evaluate the occurrence of possible dysrhythmias during guide wire insertion. Strict sterility is achieved by means of a sterile probe cover and sterile single-use gel as previously described. The internal jugular vein can be cannulated using either the long-axis or short-axis techniques. When using the short-axis technique the penetration angle of the needle is usually around 45 ° to the skin (Fig. 3.11).

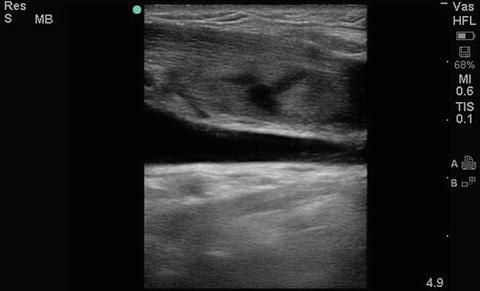

Fig. 3.12
Transverse view of the internal jugular vein and carotid artery. CA carotid artery, IJ internal jugular vein
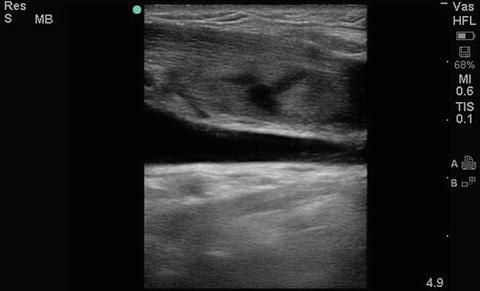
Fig. 3.13




Longitudinal view of the internal jugular vein
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree