Critical assessment
Screening and monitoring
Clinical procedures
Research
Pericardial tamponade
Intraventricular hemorrhage
Thoracocentesis
SVC blood flow
Pleural effusion
Periventricular leukomalacia
Peritoneal tap
Cerebral blood flow
Ascites or hemoperitoneum Intraventricular hemorrhage
Hydrocephalus
Suprapubic tap
Mesenteric blood flow
Patent ductus arteriosus
Confirmation of normal placement
Miscellaneous
Pulmonary hypertension
UVC/UAC
Hemodynamic studies
Central venous line
Necrotizing enterocolitis
ETT
Gastric/jejunal feeding tube
Training Recommendations
Multiple ultrasound applications are available in the NICU for different clinical indications, and each application has unique training requirements. Ultrasound applications in the NICU can be broadly classified into four categories: head ultrasound, targeted neonatal echocardiography (TnECHO), general sonography, and critical imaging. For certain applications, detailed training and practice guidelines are available, e.g., TnECHO [2]. On the other hand, some applications have been adopted less formally into clinical practice over many decades based on local experience and expertise (e.g., general sonography and critical imaging). The Australian Society for Ultrasound in Medicine has developed a standard curriculum for point-of-care ultrasound training and certification for neonatology trainees, accessible online at ASUM’s website: http://www.asum.com.au/newsite/Education.php?p=CCPU
In the United States, formal training or certification for point-of-care ultrasound in NICU is not available. It is of paramount importance to develop local guidelines before adopting this new practice in NICU. To establish a new program, collaboration with an advanced-level user (e.g., a pediatric radiologist or a pediatric cardiologist) is essential to ensure adequate training and supervision of NICU providers. Furthermore, as more advanced competencies are sought by the NICU clinician, the involvement of trained neonatologists becomes increasingly important. Ultimately, in the future the goal of all training programs should be to create and adopt a uniform set of core competencies that should be attained while completing a critical care training program, perhaps through national consensus or specialty organizations like the American Academy of Pediatrics.
Proposed Training Model
The basic training for any ultrasound application begins with an introduction to the required hardware and software, basic ultrasound physics, point-of-care ultrasound indications and limitations. Hands-on training starts in the 2nd phase, followed by the consolidation of skills in the 3rd phase (Fig. 16.1). After demonstrating proficiency with all core competencies, a provider may be upgraded to an advanced level user. Training requirements and duration of each phase are different depending upon the application of point-of-care ultrasound. Proposed training guidelines and suggestions for different applications are summarized in Table 16.2. We recommend to maintain a log book for all trainees during the basic and advanced level training.
Fig. 16.1
Proposed training model for the point-of-care ultrasound in NICU
Table 16.2
Training guidelines and suggestions for different applications of point-of-care ultrasound
Application | Basic training | Advanced training | Maintenance of skill | Remarks |
|---|---|---|---|---|
aEchocardiography (TnECHO) | 150 studies performed | 150 additional studies performed | 100 studies/year | Normal studies should be < 20 % of the total |
150 studies reviewed | 150 additional studies reviewed | CME: 24–48 h/year | ||
Duration: 4–6 months | Duration: additional 4–6 months | Peer review: once/week | ||
Consultant review: once/month | ||||
bHead ultrasound | 25–50 studies performed | 25–50 additional studies performed | 50 studies/year | Normal studies should be 30–40 % of total |
25–50 studies reviewed | 25–50 additional studies reviewed | CME: 6–12 h/year | ||
Duration: 2–4 weeks | Duration: additional 1–2 months | Peer review: once/week | ||
Consultant review: once/month | ||||
bGeneral sonography for placement confirmation of UVC, PICC line, ETT, NGT and for suprapubic tap | 15–25 studies performed | 15–25 additional studies performed | 25 studies/year | Training should separately focus on each skill, e.g., confirming UVC or PICC position |
15–25 studies reviewed | 15–25 additional studies reviewed | CME: 6–12 h/year | ||
Duration: 2–4 weeks | Duration: additional 1–2 months | Peer review: once/week | ||
Consultant review: once/month | ||||
bCritical imaging for cardiac tamponade or pleural effusion | Basic or advanced level training in functional echocardiography or general sonography applications | Peer and consultant review after every incidence in practice | Simulation for lifesaving procedures can also be helpful | |
Maintenance of skill should be ensured for advanced level users by performing a minimum required number of scans for any particular application, continued medical education or CME (courses and workshops), peer review, and quality assurance (review by consultants) of acquired images and interpretation. Requirements and suggestions for maintenance of skills for different applications are also given in Table 16.2.
After basic or advanced training, certain competencies are expected for each application of point-of-care ultrasound. Basic and advanced competencies for different applications are summarized in Table 16.3. Like training guidelines, competencies have thus far only been defined for targeted neonatal echocardiography. For other applications, most institutions depend upon the local guidelines, developed in collaboration with pediatric diagnostic imaging consultants.
Table 16.3
Basic and advanced competencies for different applications of point-of-care ultrasound
Application | Competencies | Remarks | |
|---|---|---|---|
Basic | Advanced | ||
a Echocardiography (TnECHO) | Imaging | Imaging | Functional echocardiography is not recommended in the presence of clinical suspicion for congenital heart disease |
1. Initial comprehensive study | Basic competencies | ||
2. Initial focused study | Interpretation | ||
3. Follow-up comprehensive study | All types of functional echocardiography | ||
4. Follow-up focused study | Initial comprehensive studies should be considered for review by a pediatric cardiologist | ||
Interpretation | |||
No independent interpretation except for follow-up focused studies | |||
b Head ultrasound | Imaging | Imaging | Initial comprehensive studies and all other studies with any clinically significant finding on interpretation by an advanced user should be considered for review by a pediatric radiologist |
1. Initial comprehensive study | Basic competencies | ||
2. Initial focused study | Interpretation | ||
3. Follow-up comprehensive study | All types of head ultrasound | ||
4. Follow-up focused study | |||
Interpretation | |||
No independent interpretation | |||
b General sonography (UVC/PICC line/pericardial or pleural effusion, ascites, and suprapubic tap) | Imaging | Imaging | Studies with any significant finding on interpretation by an advanced user should be considered for review by a pediatric radiologist |
1. Initial focused study | Basic competencies | ||
2. Follow-up focused study | Interpretation | ||
Interpretation | All or few variants of initial or follow-up studies; determined by the training in all or few variants of general sonography | ||
No independent interpretation except for suprapubic tap | |||
b Critical imaging | Basic or advanced level competency in functional echocardiography or general sonography and appropriate clinical training for lifesaving intervention | All images should be considered for review by a pediatric radiologist | |
Part II: Common Applications in Clinical Practice
Neonatal Head Ultrasound
Introduction and Patient Considerations
The diagnosis of severe intraventricular hemorrhage (IVH), especially with extreme prematurity, may impact the decision for redirection of medical care. Due to the significant clinical implications of diagnosing severe IVH in extremely premature infants, their head ultrasounds should be interpreted by a pediatric radiologist. After a diagnosis is made by the radiologist, point-of-care ultrasound can be utilized for follow-up imaging. However, in critical circumstances where imaging by a sonographer or a radiologist is not immediately available, neonatologists may need to evaluate for severe IVH [3] and in this situation a limited head sonography can be performed using point-of-care ultrasound in the NICU. However, all interpretations should be verified either by a pediatric radiologist or an advanced-level user, especially when severe IVH is suspected. This may be facilitated during off-hours by transferring the images via secure email or, in some instances, images can be directly uploaded onto the radiology department’s server.
Post-hemorrhagic hydrocephalus (PHH) is a common complication of IVH. Close monitoring of the ventricular size helps to guide the need for clinical interventions (e.g., serial lumber puncture, ventricular taps, or need for a temporary or permanent ventricular shunt). Daily measurement and plotting of the head circumference on a centile chart is a common practice. However, the increase in head circumference lags behind the development of persistently elevated intracranial pressure. This elevated intracranial pressure can induce brain parenchymal injury before a provider recommends any clinical intervention based on an enlarging head circumference. Point-of-care ultrasound can be adopted to monitor the progress of PHH. Ventricular dimensions can be plotted on a nomogram, and frequent and objective evaluation of ventricular size may better guide timely intervention and may improve the clinical outcome of PHH.
Periventricular leukomalacia (PVL) is a selective white matter injury to the developing brain. Incidence of PVL varies between 1.2 % and 1.5 % [4, 5]. Although magnetic resonance imaging (MRI) brain is indicated to evaluate the presence and severity of white matter injury when the index of suspicion is high, MRI brain is not recommended to screen for white matter injury in all preterm infants. Head ultrasound is a suitable test for evaluation and screening of cystic PVL. Depending upon the timing of brain injury, PVL can be evident at birth or as late as 4–6 weeks of postnatal life. Routine screening for PVL is carried out at 4–6 weeks of age. However, point-of-care head ultrasound can be helpful for more frequent screening and early diagnosis. Additional possible indications for point-of-care head ultrasound may include Doppler studies performed for research on cerebral blood flow changes during transition after delivery or, rarely, for another clinical indication (e.g., middle cerebral artery resistive index for assessing the severity of hypoxic ischemic encephalopathy).
Discussing the clinical status of the infant with the bedside nurse is of utmost importance before imaging. Sick and extremely preterm infants are prone to instantaneous desaturation and bradycardia just by touching them. In such an event, one should stop scanning and wait until the infant is completely recovered from the acute event before resuming the imaging. One should be able to perform head ultrasound in an open crib, radiant warmer, or through the portholes in an isolette. For head ultrasound, ideally an infant should be supine on a flat bed with the head kept in midline position. However, most sonographers are trained to scan in any position and still acquire standard images. This flexibility allows head ultrasound to be performed in critically sick or extremely preterm infants without changing their position in the isolette. One should be careful about the endotracheal tube, arterial and venous lines while performing sonography.
Technical Considerations
The following are technical considerations in point-of-care head ultrasound in neonates:
During the procedure these high-risk infants shall be handled gently. Avoid procedure-related hypothermia, and follow standard asepsis protocol in the unit.
A sector or curved linear probe of appropriate size to fit the anterior fontanelle should be used.
Commonly, the 5–8 MHz transducer is used for best combination of penetration and resolution. For extremely premature infants, the 8–12 MHz transducer also can be used to achieve a higher resolution image.
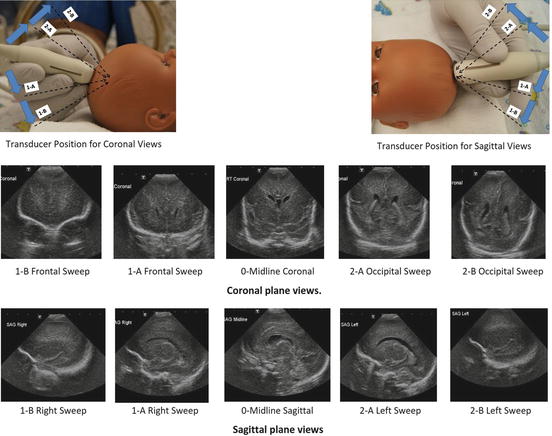
For standard imaging, the reference point on the transducer should be facing right for a coronal view and anteriorly for a sagittal view.
Image orientation: The standard orientation of the coronal image is that the baby’s right side is on the left side as you face the image. For the sagittal plane, anterior or rostral is on the left as you face the image.
Focus point: The focus point should be at the depth of the ventricles or the periventricular region. In individual cases it may be useful to adapt the focus point, aiming at a region of interest (e.g., on PVL or cerebellar hemorrhage). Also, many transducers have multiple focal zones that can be adjusted to examine a larger region of interest.
Compatible software for neonatal head ultrasound should be installed
Doppler studies and additional imaging from posterior, temporal, and mastoid fontanelle are optional depending upon the expertise and indications for the point-of-care ultrasound.
Some experts recommend saving point-of-care ultrasound in a video format. This will facilitate the interpretation of the scan as the frame-by-frame review will be possible in video format.
Image Acquisition and Interpretation
Several windows are used to perform a comprehensive head ultrasound to look into various parts of the brain. The anterior, posterior, mastoid, and temporal fontanelle views are recommended for comprehensive imaging. However, for a point-of-care ultrasound, conventional views via the anterior fontanelle may be sufficient.
Conventional views are obtained through the anterior fontanelle as shown in Fig. 16.2. Start imaging with the coronal planes: the reference point on the transducer should be on the right side for coronal views. Both Sylvian fissures, frontal horns of both lateral ventricles, and the third ventricle should be clearly visible in the midline coronal view. Sweep from orbits to occiput; save 5–6 images in coronal view as shown in Fig. 16.2. Appropriately mark the frontal and occipital views while performing an anteroposterior sweep in the coronal plane.