17 | Diagnostic and Clinical Significance of Doppler Ultrasound in Obstetrics |
Doppler ultrasound is a noninvasive method of examining blood flows. In obstetrics Doppler ultrasound is used chiefly to study the uteroplacental and feto-placental vessels, but it is also used to examine the vessels of the fetus itself. The examination in these cases is applied to flow patterns and to Doppler indices that are derived from the flow curve and are not dependent on the insonation angle (Evans et al. 1989, Gonser 1989, Vetter and Gonser 1992). In cardiac anomalies and disturbances of cardiac rhythm in particular, quantitative studies of ongoing aortic perfusion and Doppler echocardiography may be performed.
In recent years numerous studies have shown a significant link between an abnormal Doppler finding and an abnormal outcome of a pregnancy. Consequently, Doppler ultrasound has been increasingly integrated, but perhaps prematurely, into the diagnostic workup of the condition of the fetus and clinical management (Divon et al. 1989, Dornan and Harper 1994, Low 1991, Visser et al. 1991). Two questions should be asked before making a major commitment to Doppler ultrasound in pregnancy: firstly, whether Doppler ultrasound will provide additional information about the condition of mother and infant, and secondly, whether the outcome of the pregnancy can be improved if the Doppler finding is integrated into clinical management. The question concerning the additional information relates to diagnostic significance; the question concerning the expectation of improved outcome relates to the clinical significance of the procedure.
Diagnostic significance describes the diagnostic power of a clinical procedure (efficiency). By contrast clinical significance describes its usefulness in clinical management (effectiveness), taking into account its attendant risks. To examine diagnostic significance an adequate procedure would be a purely observational study, while the ideal procedure to test clinical significance is a prospective randomized management or intervention study (Altman 1991, Thornton and Lilford 1993).
It seems unrealistic to think that a new procedure that is used especially in late pregnancy would improve the outcome of the pregnancy materially. Previously introduced procedures leave little room for further improvement by the addition of newer methods. Moreover, there are indications that the development of pathology in a pregnancy begins as early as conception or in early pregnancy, and that perinatal events contribute less to long-term morbidity than previously assumed (Newnham et al. 1991). Cerebral palsy seems to be at least one instance of this, but other, less severe neonatal defects may belong in this category (Blair and Stanley 1988, Longo 1992, Melone et al. 1991, Naeye et al. 1989). Hence introducing Doppler ultrasound late in pregnancy cannot be expected to bring dramatic improvements in morbidity statistics.
Studies of Diagnostic Significance
The diagnostic significance of Doppler ultrasound in obstetrics is measured by the reliability with which an abnormal Doppler finding is associated or correlated with a negative pregnancy outcome. Criteria for the evaluation of diagnostic significance are among others sensitivity (sens.) and specificity (spec.) together with positive and negative predictive value. These parameters are determined in an observational study, i. e., the Doppler finding is only observed and at this stage must not be integrated in the clinical management (Maršál 1991, Thornton and Lilford 1993). While positive and negative predictive values depend on the clinical population being studied, sensitivity and specificity are independent of this factor (Buekens and Kaminski 1988, Grant and Mohide 1982).
The literature is full of studies addressing diagnostic significance. Hence in what follows we can only present a selection. The studies find a significant association between abnormal Doppler readings and the following pathological conditions in obstetrics: growth restriction, dystocia, and premature delivery (Trudinger et al. 1991), acidosis on cordocentesis (Ni-colaides et al. 1988, Weiner 1990), abnormal cardiotocogram (CTG) before delivery (Dempster et al 1989), depression and acidosis of the newborn (Bekedam et al. 1990, Gudmundsson et al. 1990, Reuwer et al. 1987, Soothill et al. 1993), cerebral hemorrhage, neonatal intensive care (Trudinger et al. 1991, Weiss et al. 1992), and histopathological changes in the placenta (Giles et al. 1985, Hitschold et al. 1992, McCowan et al. 1987) and the placental bed (Voigt and Becker 1992).
Uteroplacental Arteries
A postsystolic notch in the uteroplacental waveform in the second trimester is due to an abnormal reflection of the pulse wave in the spiral aa. (Adamson et al. 1989), which is presumably the result of impaired trophoblast invasion during placentation in the first half of pregnancy (Brosens et al. 1972). According to Campbell et al. (1983) a notch is the characteristic Doppler sonographic correlate of preeclampsia, defined as hypertension with proteinuria, and according to Fleischer et al. (1986) the association of such a notch with dysto-cia or premature delivery is highly significant in hypertensive pregnant women (sens.: 87%; spec.: 95%). This suggests that as an indicator of hypertensive complications of pregnancy the finding of a notch is clearly superior to creatinine clearance or uric acid level.
With unilateral implantation of the placenta the incidence of preeclampsia and intrauterine maldevelopment is significantly higher than with central implantation (Kofinas et al. 1989). Our own studies show that, if preeclampsia is already established when a unilateral placental implantation is discovered, the contralateral Doppler findings in the uteroplacental bed are significantly associated with the clinical and metabolic condition of the newborn (sens.: 70%; spec.: 75% for a 5-minute Apgar <7, pH[umbilical a. (UA)] <7.15, or base excess (BE)[UA] <-8 mmol/L). According to Thaler et al. (1992) pregnancies with hypertension > 140/90 that also show a contralateral notch lead with significantly increased frequency to fetal maldevelopment, cesarean section for an abnormal CTG, and long-lasting neonatal intensive care.
In contrast to these studies performed on high-risk pregnancies, Steel et al. (1990) conducted screening examinations of the uteroplacental circulation at 18 and 24 weeks of gestation. Abnormal Doppler findings on both occasions were followed by an increase in risk for subsequent hypertensive complications of the pregnancy, for example, the risk for hypertension increased from 5 % to 25 %, for preeclampsia from 1 % to 10%, and for intrauterine growth restriction (IUGR) from 7% to 27%. Harrington et al. (1991) in a screening study using a comparable protocol found preeclampsia as a sequela with a sensitivity of 76% and a specificity of 96%. These studies suggest that it would be reasonable to screen patients with a clinically unremarkable pregnancy for the risk of later hypertensive complications of pregnancy.
Umbilical Arteries and Other Fetal Vessels
Umbilical Arteries and Fetal Aorta
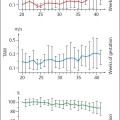
According to Trudinger et al. (1986) the prenatal Doppler findings are associated with dystocia and depression of the newborn more strongly than the prenatal CTG (CTG-NST [nonstress test]: sens.: 36%; spec.: 88%; Doppler: sens.: 60%; spec.: 85%). The results of Schulman et al. (1989) were even more significant for an association with later decelerations of the CTG, acidosis, low 5-minute Apgar scores and neonatal intensive care (CTG- NST: sens.: 7.6%; spec.: 97%; Doppler: sens.: 50%; spec.: 96%). Yoon et al. (1992) compared Doppler ultrasound of the umbilical aa. with a biophysical profile in a high-risk population who had an elective primary cesarean section. Both methods were highly significantly associated with the pH in the umbilical aa., and Doppler ultrasound achieved a somewhat higher proportion of hits (sens.: 86% vs. 64%; spec.: 96 vs. 90%). However, this conclusion has been questioned by other authors. Weiss et al. (1989) compared Doppler sonography of the umbilical aa. with the oxytocin challenge test (OCT) in IUGR, looking at their association with the frequency of cesarean section for abnormal CTG changes and the frequency of low Apgar scores and low pH values in the neonate. Doppler ultrasound detected the indicated risks before the OCT, sensitivity and specificity being high in both methods.
End-diastolic block in the umbilical aa. of a growth-restricted fetus is one of the most reliable warning signs of threatened hypoxemia, defined by subsequent intrauterine fetal death or pathological CTG changes followed by cesarean section (sens.: 77%; spec.: 100%) (Reuwer et al. 1987). This finding is confirmed by the fact that in a high-risk pregnancy end-diastolic block is significantly associated with prenatal hypoxia and acidosis despite primary cesarean section (sens.: 78% vs. 90%; spec.: 98% vs. 92%) (Tyrrell et al. 1992).
Doppler ultrasound is suitable for perinatal prognosis of IUGR and other risks of pregnancy, but it is not suitable for screening to detect IUGR. For this fetometry is a far superior routine procedure (Beattie and Dornan 1989, Bekedam et al. 1990, Berkowitz et al. 1988, Bruinse et al. 1989, Burke et al. 1990, Dempster et al. 1989, Maršál 1991, Reuwer et al. 1987, Soothill et al. 1993).
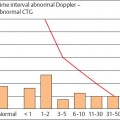
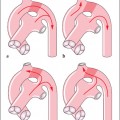
The Umbilical Vein in Arterial Diastolic Block or Reverse Flow
An abnormal Doppler finding in the umbilical a. precedes abnormal CTG changes by a few days to weeks (Schmidt et al. 1993). This interval appears to diminish with increasing gestational age (Bekedam et al. 1990) and when an end-diastolic block is already present (Arabin et al. 1988, Reuwer et al. 1987, Rochelson et al. 1992, Schmidt et al. 1991). When pulsations in the umbilical v. then supervene, sporadic late decelerations can be demonstrated just a few days later (Arduini et al. 1993).
Pulsations in the umbilical v. are an expression of pathological changes in the central hemodynamics of the fetal heart and in the inferior vena cava (IVC) (Ling-man et al. 1986, Reed et al. 1990, Rizzo et al. 1992). They are associated with greater mortality than end-diastolic block by itself (Indik et al. 1991). Pulsations in the umbilical v. presage imminent conversion of an end-diastolic block into reverse flow in just zero to three days (Gonser 1992). Diastolic reverse flow is the most extreme pathology in the flow pattern of the umbilical a. and when compared with end-diastolic block is associated with a distinctly higher perinatal mortality of about 40% to 75% (Brar and Platt 1988, Gonser et al. 1993, Mandruzzato et al. 1991, Schmidt et al. 1991).
Cerebral Arteries and Redistribution of the Circulation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree