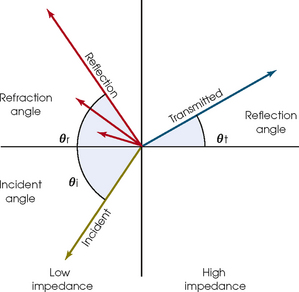
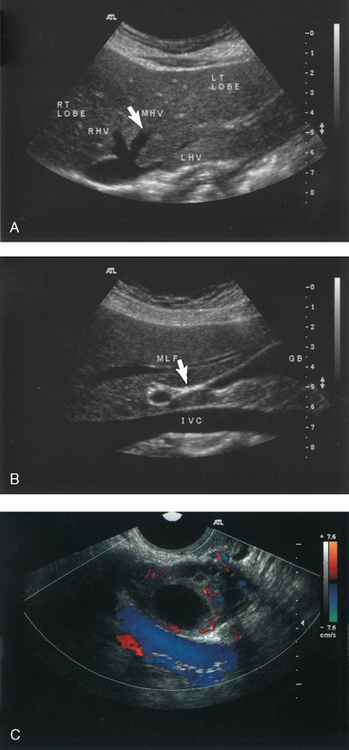
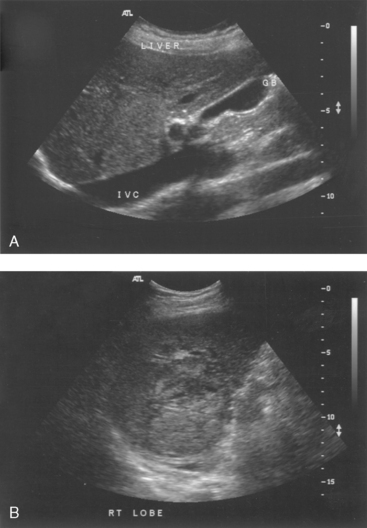
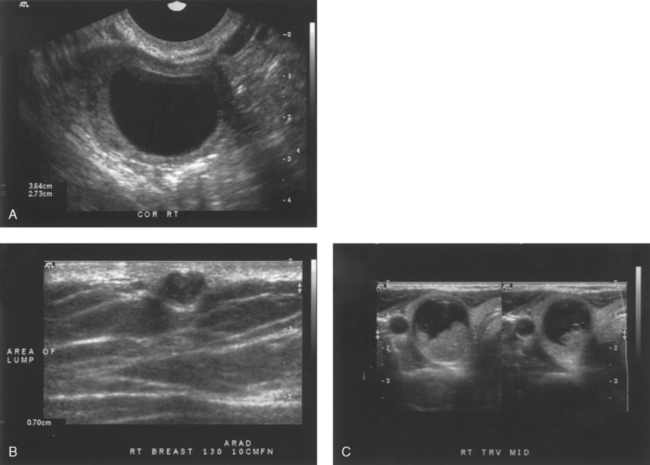
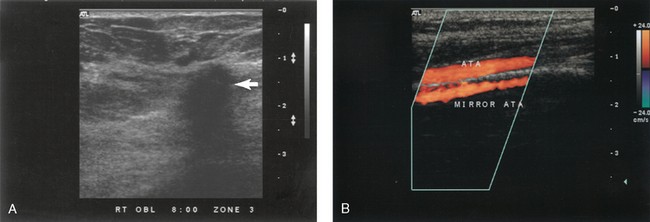
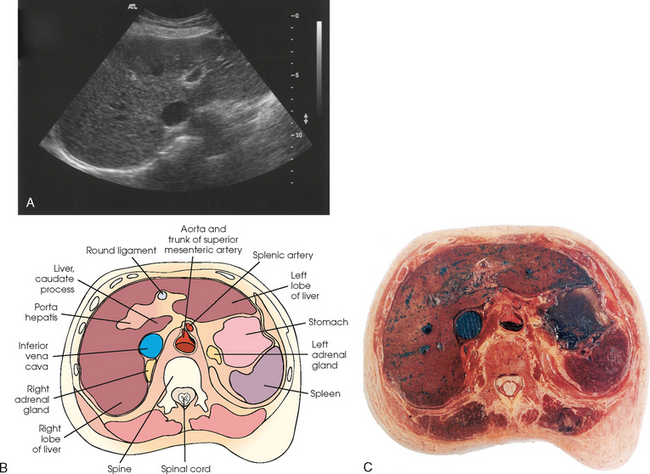
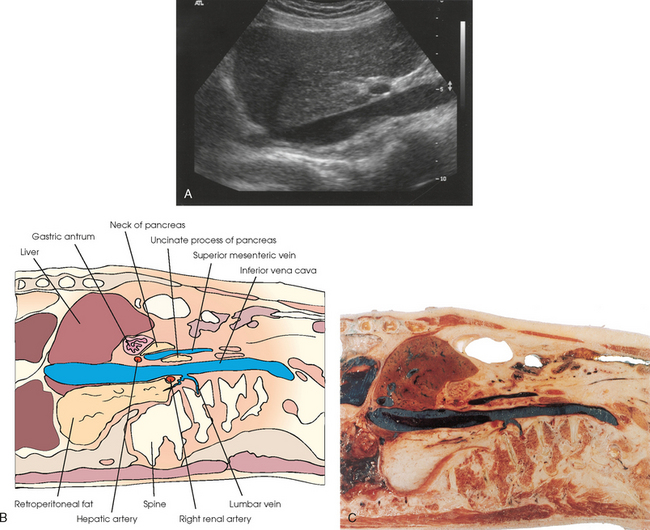
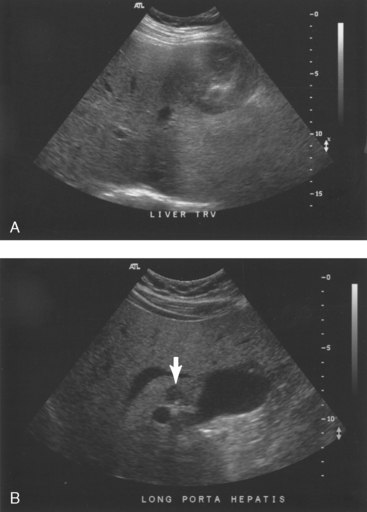
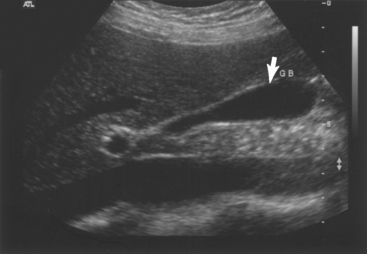
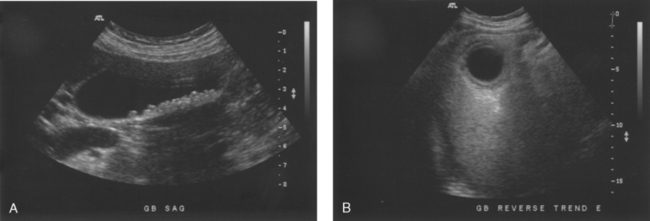
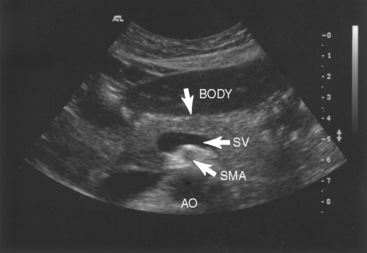
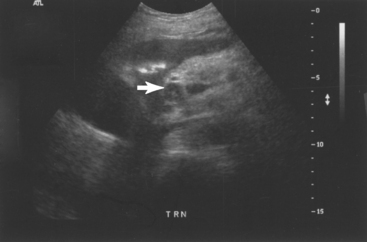
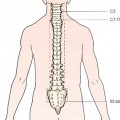
33 Physical requirements play an additional role in sonography. Sonographers must be able to aid in moving patients and medical equipment. Attention to the use of proper body mechanics is essential (Fig. 33-1). Repetitive usage injury or syndrome of the neck, shoulder, elbow, wrist, and back have been documented. The sonographer should be in good physical, emotional, and nutritional health and possess a dedication to continual learning. The career can be exciting and rewarding as well as stressful, demanding, frustrating, and occasionally depressing. The development of sonar* was the precursor to medical ultrasound. Sonar equipment was initially constructed for defense efforts during World War II to detect the presence of submarines. Various investigators later proved that ultrasound had a valid contribution to make to medicine. Sound travels through tissues at different speeds depending on the density and stiffness of the medium. Acoustic impedance of a medium determines how much of the wave transmits to the next medium (Fig. 33-2). Imaging transducers routinely operate in a frequency range of 2 to 16 MHz. Transducers may be linear, convex, sector, or vector in construction (Fig. 33-3). Higher frequencies are used in intracavity and intraluminal transducers and for visualizing the extremities or superficial structures. Lower frequencies are needed for deeper structures of the thoracic cavity, abdomen, and pelvis. Lower frequencies provide necessary penetration depth at the expense of detail resolution. Volume scanning allows for quick “sweeps” of specific areas of the body or fetus. These sweeps give volume data that can be rendered even after the patient has left the ultrasound department. Threedimensional imaging systems allow the sonographer to acquire volume data. The sonographer can reconstruct these data into a three-dimensional image on the ultrasound machine or at a workstation. With four-dimensional imaging, the ultrasound system is able to acquire and display three-dimensional images in real time. The use of anatomic landmarks to define specific areas of the human body is an important part of the imaging and orientation skills of the sonographer. The middle hepatic vein is a sonographic landmark used to locate the division between the left and right hepatic lobes (Fig. 33-4, A). The main lobar fissure is used to locate the gallbladder fossa (Fig. 33-4, B). The ovaries are located medial and anterior to the iliac vessels (Fig. 33-4, C). The use of anatomic landmarks is a routine part of many sonographic examinations. CHARACTERISTICS OF THE SONOGRAPHIC IMAGE The sonographer uses specific terms to characterize the sonographic image. If the echo pattern is similar throughout a structure or mass, it is termed homogeneous (Fig. 33-5, A). If the echo pattern is dissimilar throughout a structure or mass, it is termed heterogeneous (Fig. 33-5, B). Internal composition of a structure or mass is described using the terms anechoic (without internal echoes), echogenic (with internal echoes), and complex (containing anechoic and echogenic regions) (Fig. 33-6). Descriptive terms are also used by the sonographer to describe the borders of a mass. Are the borders smooth or irregular; thin or thick; calcified or dilated? Imaging artifacts are an additional concern for the sonographer. Acoustic artifacts include reflections that are missing; not real; improperly positioned; or of improper brightness, number, shape, or size (Fig. 33-7). Understanding the assumptions of the ultrasound system and the physical principles of sound waves, the sonographer is better able to comprehend the real-time images. The abdominal ultrasound examination generally includes a survey of the liver, pancreas, gallbladder, spleen, great vessels, and kidneys in the sagittal and transverse planes (Figs. 33-8 and 33-9). Specific protocols are followed to image size, shape, and echogenicity of the organ parenchyma and anatomic relationships of the surrounding structures. Doppler flow patterns of the upper abdominal blood vessels may be included. Patients are examined in two different body positions (i.e., supine and decubitus). The use of two positions shows mobility of gallstones and repositions interfering bowel gas. Air reflects most of the sound wave, making visualization of the abdominal and retroperitoneal structures difficult. Abdominal examinations are typically scheduled in the morning with the patient fasting 6 to 8 hours before the sonogram. The retroperitoneal ultrasound examination includes a survey of the great vessels, kidneys, and bladder in the sagittal and transverse planes before and after voiding. Specific protocols are followed to image the size, shape, cortical thickness, and echogenicity of the renal parenchyma. Diameters of the inferior vena cava, aorta, and common iliac arteries are measured and documented. Doppler flow patterns of the great vessels and kidneys may be included. Retroperitoneum examinations can be scheduled in the morning or afternoon with the patient drinking 8 to 16 oz. of water 1 hour before the sonogram. Sonographic examinations of the liver and biliary tree are generally requested in patients with right upper quadrant pain or elevations in liver function laboratory tests. The liver is assessed for size and echogenicity of the parenchyma. Under normal circumstances, the liver parenchyma appears moderately echogenic and homogeneous. Some types of liver pathologies shown on ultrasound include fatty infiltration, cirrhosis, cavernous hemangioma, and hepatoma (Fig. 33-10). Doppler evaluation of the hepatic artery, hepatic veins, and portal veins is included with a patient history or suspicion of cirrhosis, portal hypertension, portal vein thrombosis, and Budd-Chiari syndrome. The biliary tree includes the gallbladder and the intrahepatic and extrahepatic bile ducts. The gallbladder is evaluated for size, wall thickness, and absence of internal echoes. Under normal circumstances, the gallbladder is a pear-shaped anechoic structure located in the gallbladder fossa on the posterior surface of the liver (Fig. 33-11). The intrahepatic biliary ducts converge near the porta hepatis forming the common hepatic duct. The cystic duct joins the common hepatic duct to form the extrahepatic common bile duct. The biliary tree is evaluated for size and evidence of intraductal stones or masses. Some abnormalities of the biliary tree shown on ultrasound include intrahepatic and extrahepatic biliary obstruction, cholelithiasis, and cholecystitis (Fig. 33-12). The pancreas is an elongated organ oriented in a transverse oblique plane in the epigastric and left hypochondriac regions of the retroperitoneal cavity. The head of the pancreas lies in the descending portion of the duodenum and lateral to the superior mesenteric artery. The body is the largest portion, lying anterior to the superior mesenteric artery and splenic vein (Fig. 33-13). The tail is the superiormost portion lying posterior to the antrum of the stomach and generally extends toward the splenic hilum. The echogenicity of the pancreas varies depending on the amount of fat but should appear homogeneous throughout the organ. Ultrasound examinations of the pancreas are requested in patients with a history of unexplained weight loss, epigastric pain, and elevation in pancreatic enzymes or liver function laboratory tests. The pancreas is evaluated for size and echogenicity of the parenchyma. The distal common bile duct is routinely measured in the head of the pancreas. Some abnormalities of the pancreas shown on ultrasound include inflammation, calcifications, tumor, or abscess formation (Fig. 33-14).
DIAGNOSTIC ULTRASOUND

Principles of Diagnostic Ultrasound
CHARACTERISTICS OF DIAGNOSTIC MEDICAL SONOGRAPHERS
Historical Development
Physical Principles
Acoustic impedance
TRANSDUCER SELECTION
VOLUME SCANNING AND THREE-DIMENSIONAL AND FOUR-DIMENSIONAL IMAGING
Anatomic Relationships and Landmarks
Clinical Applications
ABDOMEN AND RETROPERITONEUM
Liver and biliary tree
Pancreas