Fig. 16.1
Clinical features of oedema: (a) lymphoedema of the foot with swollen toes and transverse creases on the distal part of the dorsal surface of the foot. (b) Lipoedema with a slender foot and ankle. The oedema is symmetrical and starts above the gaiter area which gives the appearance of a constriction. (c) Lipolymphoedema with classic broadening of the calf and slender ankle as with lipoedema. Note the secondary lymphatic oedema on the dorsal surface of the foot
Copyright: [Author]
Phleboedema is part of chronic venous insufficiency. With this condition the venous capillaries distend from the raised ambulatory venous pressure. This itself is caused by a reduced venous filling time and raised venous filling index (Lattimer et al. 2013). The increased intravascular pressure leads to extravasation of fluid by the Starling mechanism. The extravasation of blood components like haemosiderin stimulates melanin release, and the whole process causes hyperpigmentation, induration and fibrosis of the gaiter area. This typical brown skin discolouration is termed dermatoliposclerosis. Circumferential venous ulcers can result in a secondary lymphoedema of the foot.
Lipohyperplasia and lipoedema may occur independently of lymphoedema or phleboedema and is sometimes familial. In these conditions there is a symmetrical thickening of the subcutaneous fatty tissue, starting in the supramalleolar region (gaiter area) and extending to the thigh. Lipohyperplasia is the first phase of the disease and is painless. Later, pain sets in as the pressure increases. It is a fat distribution dysfunction or lipodystrophy. It is not a form of obesity because the cell count in the subcutaneous fatty tissue is abnormally high. This is in contrast to adiposis which is the accumulation of fat into a constant number of cells. The clinical picture is limited initially to calf, thigh and pelvic oedema, but the foot remains unaffected (Fig. 16.2) (Cornely 2011 in Appendix 2). In its further course, lipoedema may obstruct the lymphatic drainage due to increased pressure in the tissue giving rise to mixed forms of lipolymphoedema with pain and involvement of the foot and toes.
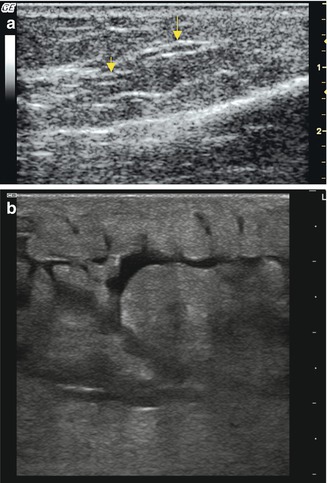
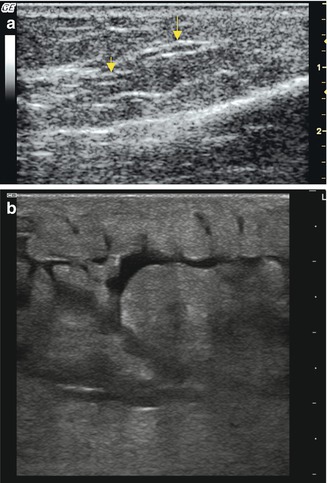
Fig. 16.2
(a) Longitudinal view through the inner calf in lymphatic oedema demonstrating sclerosed collectors with thickened walls (arrowed). (b) Acute lymphatic oedema with free fluid between islands of fatty tissue and stretched collecting ducts
Copyright: [Author]
Many systemic diseases may cause secondary oedemas in the extremities (Table 16.1).
Table 16.1
Systemic causes for oedemas in the extremities
Cause | Clinical picture |
|---|---|
Renal | Glomerulonephritis, nephrotic syndrome |
Cardiac | Right ventricular failure |
Hepatic | Cirrhosis of the liver |
Vascular | Acute tissue ischaemia, oedema after revascularisation |
Intestinal | Ulcerative colitis, enteropathy, malabsorption |
Thyroid disease | Hyper- or hypothyroidism |
Iatrogenic | Medications including antihypertensives, nonsteroidal anti-inflammatory drugs, steroids, proton-pump inhibitors, hormones, ciclosporin, immunosuppressive agents |
Nutritional | Protein deficiency, malnutrition |
Infectious | Cellulitis, borreliosis, filariasis |
Pregnancy and hormones | Cyclical oedema, eclampsia and pre-eclampsia |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree