Fig. 5.1
Apparatus for patients to stand on during examination (Dr. Faiez Baghdadi, Neustadt an der Orla; by kind permission)
(Copyright: Dr. Faiez Baghdadi, Neustadt an der Orla)
In the author’s opinion, the tilt table is unsuitable as the backs of the legs cannot be examined easily because the patient is required to turn around repeatedly on the small step at the end of the table. It would be much easier if they were standing freely.
A raised apparatus with a surrounding railing is more comfortable and stable for the patient (Fig. 5.1). However, the vertical supports may hinder the doctor’s work. A further disadvantage is that when patients faint and fall backwards, there is no couch behind to rescue them.
The author therefore prefers a combination of a platform set in front of the examination couch whilst sitting on a low stool or exercise ball (Fig. 5.2).


Fig. 5.2
A workstation for superficial leg vein examinations
(Copyright: [Author])
The ultrasound machine should be placed to the left of the examiner. However, as the monitor is mounted on top of the machine and the patient is standing in front, the examiner must turn his head to the left and upwards to see the monitor. This position frequently leads to problems in the cervical and thoracic spine. Such can be avoided by installing an additional screen close to the patient’s legs to avoid repetitive head turns.
5.2 Examination Modes
5.2.1 Examination of the Patient Standing, Sitting or Lying
The ideal position for the patient is standing for a variety of reasons, the most important being that standing is the position in which patients are most symptomatic and is the position in which identification of reflux is most reliable (DeMuth et al. 2012). Also because the veins become fully distended, even small connecting and perforating veins can be easily identified (Fig. 5.3). Furthermore, reflux due to gravity is accentuated by provocation manoeuvres like manual compression and the Paraná, Wunstorf and orthostatic manoeuvres, which are only possible when standing (Chap. 6). Standing was recommended as the best position in the international consensus document on duplex ultrasound examination of leg veins (Coleridge-Smith et al. 2006).
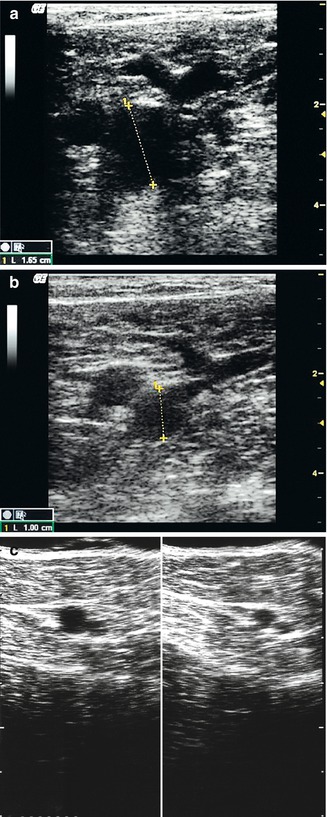
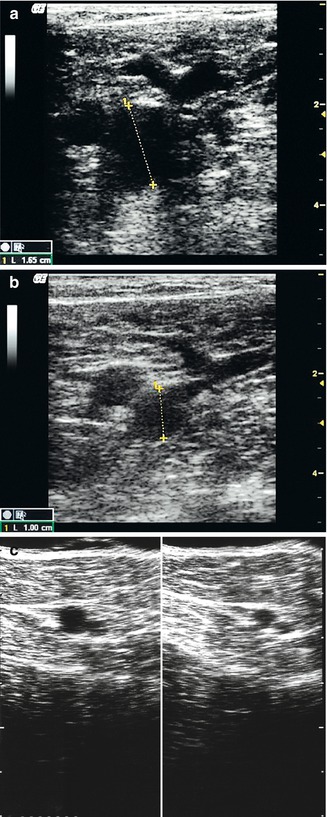
Fig. 5.3
(a) Common femoral vein in a standing patient at a diameter of 16.5 mm. Transverse view through the right groin. (b) Common femoral vein in the same patient lying down at a reduced diameter of 10 mm. The probe was gently applied so as not to compress the great saphenous vein. (c) Transverse view through right thigh great saphenous vein with a perforating vein in the adductor canal (previously Dodd’s perforator) in the same patient standing (left) and lying (right). Note the reduced calibre on lying
(Copyright: [Author])
Patients who are unable to stand or repeatedly feel unwell during the examination can be examined sitting, but the prognostic value of provocation manoeuvres (Chap. 6) is limited under these conditions.
Some colleagues examine veins in the recumbent patient, as this is the usual position for insonating arteries and for detecting deep vein thrombosis. In a lying patient, the common femoral vein in the groin is much smaller than the common femoral artery, whereas in a standing patient, it expands to at least twice the diameter (Fig. 5.3a, b). It is possible to provoke antegrade flow in a lying patient by manual compression or manual activation of the calf muscles by foot movements. However, reflux is sometimes not detected following these manoeuvres because there is insufficient gravitational effect. In a supine patient, reflux can best be provoked by the Valsalva manoeuvre or by applying pressure on the abdomen, even if distal compression may prompt a reflux in proximal portion of the saphenous veins in this position. The examiner will miss many findings by examining underfilled veins. Examination of varices in lying patients should therefore be avoided as far as possible.
5.2.2 Examination in Special Situations
Patients with standing disabilities can be examined sitting down. In this situation, the Wunstorf manoeuvre cannot be used so the patient’s calves must be compressed manually. In patients with muscle spasticity, compression manoeuvres should be applied cautiously to avoid triggering muscle cramp which is unpleasant for the patient.
In patients with leg pain and tenderness, the examination should be kept as short as possible and restricted to the central problem. The patient can be re-examined once the leg settles. Manual calf compression should be avoided in so far as possible if it causes pain or performed at a later time. Alternatively, foot compression can be used if the examiner does not wish to apply the Wunstorf manoeuvre or the patient is unable to move his feet or toes.
In patients with pronounced oedema, the veins may be scarcely sonographically visible, especially in the lower leg region. At best, the course of the saphenous trunks can be estimated. Even then, flow may not be demonstrated because the oedema compresses the vessels making them less visible on ultrasound. The correct sequence would be the treatment of the oedema with recall of the patient in order to carry out a fresh examination under improved conditions. Combinations of leg elevation, manual lymphatic drainage and especially compression bandages or stockings are usually successful. If there is a strong suspicion of DVT, it cannot be safely ruled out in this type of patient. Therefore, in such patients, consideration should be given to treatment with anticoagulants until the definitive examination.
Obese patients are more difficult to examine. The veins are deeper, and image resolution becomes poorer with increasing distance from the probe. It is often necessary to switch to a low-frequency probe (Fig. 5.4). The lumen of the vein may be compressed inadvertently in order to get a clearer image. If the examiner tries to get too close by pressing too hard, the vein may disappear altogether.
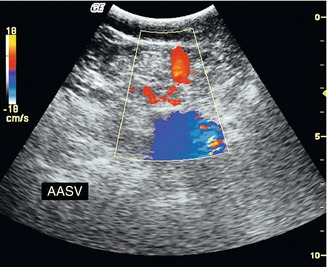
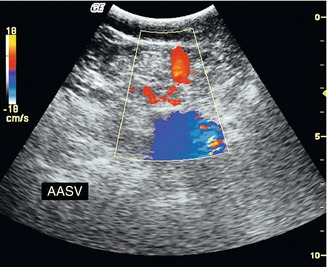
Fig. 5.4
Ultrasound of an obese patient. Transverse view through the left groin with 3.5 MHz curved array probe during muscular systole. The common femoral vein lies at a depth of 5 cm (blue); the anterior accessory saphenous vein is refluxive (red); the great saphenous vein is not shown
(Copyright: [Author])
Patients with venous ulcers must be treated as a priority. Perforating veins may lie beneath and often contribute to the ulceration. General examination of the leg veins can be carried out as described. The author proceeds in patients with inflammatory or suppurating ulcers by first treating the wound and applying compression. As soon as the wound base is clean, the underlying zone can be examined by ultrasound using ultrasound gel. The transducer head should be cleaned before and after the examination with disinfectants recommended by the supplier.
5.3 Course of the Examination
5.3.1 Interview the Patient
It is essential to establish the patient’s phlebological case history before the ultrasound examination begins, particularly:
Type and extent of ailment and when it began
Prior examinations and results
Previous interventions like surgery, endothermal ablation or sclerotherapy
Family and personal history of thrombosis
The answers to these questions may indicate the cause of the condition which may not be venous. The patient should also be asked about underlying conditions and current medication.
5.3.2 Examination
The examination process is a matter of individual preference. The decision has to be made whether the entire superficial vein system, as well as the deep veins in the popliteal region and the groin, should be examined as a matter of routine or only the affected region(s) based on the symptoms. However, important information may be overlooked if only parts of the venous system are examined. It is the author’s view that there are certain basic regions which should always be examined before reaching a diagnosis of “superficial venous system free of pathological findings”.
In order to avoid overlooking or forgetting any segment, it is recommended that an examination routine should be developed and the same course always followed. Below is a suggested order of examination (minimum requirements are shown in italics):
Examination of the groin:
Deep leg veins compressible?
Flow?
Saphenofemoral junction refluxive?
Saphenofemoral junction tributaries refluxive?
Course of the great saphenous vein to the knee in the B-scan, with branches and perforating veins, switch on colour and/or PW-mode when sudden changes in calibre are encountered
Diameter of great saphenous vein in the thigh if reflux occurs
Course of great saphenous vein from knee to ankle in the B-scan, with branches and perforating veins, switch on colour and/or PW-mode when sudden changes in calibre are encountered
Examination of posterior tibial perforating veins (Cockett’s perforators)
Examination of the popliteal region:
Deep leg veins compressible?
Flow?
Saphenopopliteal junction refluxive?
Vein of Giacomini present?
Refluxive?
Course of small saphenous vein to the ankle in the B-scan, with branches and perforating veins, switch on colour and/or PW-mode when sudden changes in calibre are encountered
Examination of back of thigh to exclude refluxive Hach perforating vein
Examination of visible side branches to establish origin of reflux
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree