Fig. 2.1
The venous valves in the leg. (a) With upward flow, the valve opens. (b) When there is return flow, the blood flows back into the “swallow’s nest” (small arrows) and closes the valve
Copyright: [Author]
The nomenclature used follows international convention. The saphenous trunks are the “great saphenous vein” (GSV) (Latin: V. saphena magna) and the “small saphenous vein” (SSV) (Latin: V. saphena parva). In international use, the accessory veins are called anterior (formerly lateral), superficial and posterior (formerly medial) accessory saphenous veins (Caggiati et al. 2002).
This chapter describes the anatomy of the superficial veins (Askar 1963; Dodd and Cockett 1976; Bergan 1999; Caggiati and Mendoza 2004; Cavezzi et al. 2006; Kubik 1985 in Appendix 2). To avoid duplication, anatomical variants important for diagnosis will be discussed in the relevant chapters. The deep venous system is described in Chap. 14.
2.2 The Fascial Compartment of the Saphenous Veins
In addition to the subfascial and epifascial veins, the perforating veins are described as transfascial. The muscle fascia or deep fascia is regarded as the border. According to this description, all the veins which lie between the muscle fascia and the dermis are called superficial with no further differentiation. However, the great saphenous vein, small saphenous vein and the proximal section of the accessory saphenous veins run in their own intermediate fascial compartment with the tributaries remaining truly epifascial.
2.2.1 Membranous Layer
The subcutaneous tissue is constructed around a skeleton of connective tissue, which is filled with fat (Fig. 2.2). On ultrasound, this connective tissue is visible as white, echogenic layers which blend irregularly into the grey fat tissue in widely differing patterns (Fig. 2.3a). In the deeper zone of the subcutaneous tissue, the connective tissue fibres thicken to form a membrane which usually lies directly on the muscle fascia. This is called the membranous layer or pseudofascia. This membranous layer is not a duplication of the muscle fascia as described in the anatomy book by Tillaux in 1897, because their embryological origin is different. Muscle fascia arises from the mesoderm, while the membranous layer arises from the ectoderm (Tillaux 1897 in Appendix 2).
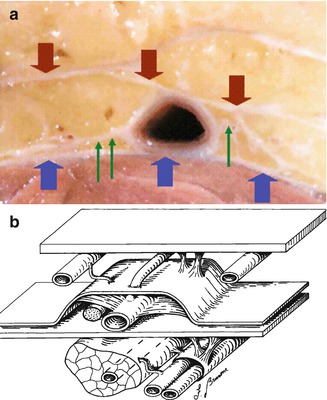
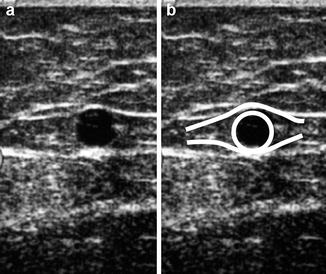
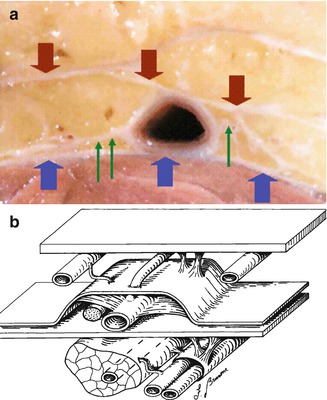
Fig. 2.2
(a) Section through the thigh in an anatomical preparation demonstrating layers of connective tissue separating cushions of fat around the great saphenous vein. (b) Sketch depicting the anatomical section with the muscle fascia and immediately above it the great saphenous vein in the fascial compartment. A connecting tributary is seen in the subcutaneous fatty tissue (Prof. A. Caggiati, Rome; by kind permission)
Copyright: A. Caggiati, Rome
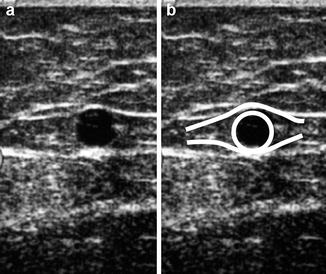
Fig. 2.3
(a) Transverse view through the thigh showing the great saphenous vein. (b) Overlay highlighting the “saphenous eye” where the upper lid is the saphenous fascia, the lower lid is the muscle fascia and the iris is the great saphenous vein. In the upper half of both images, the structure of the lax subcutaneous connective tissue can be seen as a white pattern in the grey fatty tissue
Copyright: [Author]
The muscle fascia and the membranous layer form a structural unit of connective tissue separating the muscle from the subcutaneous fatty tissue. In some parts of the leg, the two fasciae separate to form a tunnel for the veins and their accompanying arteries, nerves and lymphatic vessels. This tunnel is called the compartment of the great and small saphenous veins. In the upper part of the leg, it also contains the accessory saphenous veins. Within the fascial compartment, there are varying amounts of fat cushioning the vein (Figs. 2.3 and 2.4). Fascial compartments are found surrounding the following structures within the leg:
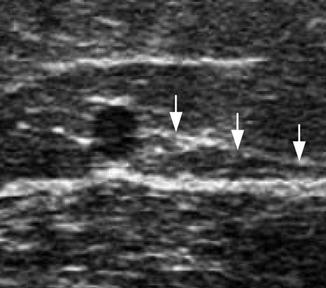
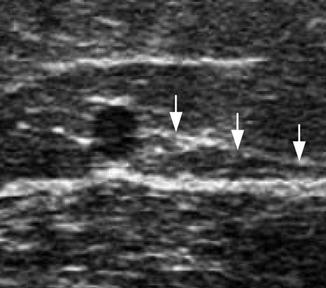
Fig. 2.4
Transverse view through the thigh in an obese patient showing the great saphenous vein within its fascial compartment surrounded by fat. The arrow demonstrates the saphenous ligament
Copyright: [Author]
Great and small saphenous veins.
Vein loops on the dorsum of foot connecting the great and small saphenous veins.
Proximal section of the anterior accessory saphenous vein.
Proximal section of the posterior accessory saphenous vein and occasionally along its entire course up to the confluence with the small saphenous vein.
In the region of the greater trochanter, mentioned for completeness. The principal content in this compartment is fat and it is only surgically important in the context of liposuction.
The membranous layer along the saphenous veins is seen as a white layer on ultrasound and can be distinguished easily from the surrounding echo-poor fat and muscle fascia. The fascia enveloping the saphenous trunks is important as a landmark for diagnosis and treatment and has only recently been discovered by duplex ultrasound. The characteristic ultrasound image of the saphenous veins between the two fasciae led to the description of the saphenous eye (Bailly [1995]) (Fig. 2.3b).
2.2.2 Saphenous Compartment
The saphenous veins lie directly on the muscle fascia. At some point along their course, the membranous layer separates from the muscle fascia to form a cover over the vein. These fasciae form an enclosed volume called the “saphenous compartment” (Caggiati and Ricci 1999; Caggiati 2001). In lean legs, this saphenous compartment is limited and contains very little fat (Fig. 2.3). The saphenous veins are tightly enclosed. However, in legs swollen by lipoedema, the saphenous compartment appears enlarged and stretched on ultrasound (Fig. 2.4). Here, a layer of fat is usually seen separating the vein from its enveloping fascia.
The membranous layer along the course of the saphenous vein was given the name saphenous fascia and has since been adopted into anatomical nomenclature.
2.2.3 Anchoring of the Saphenous Veins
In transverse view, two echogenic connective tissue streaks are visible which appear to anchor both sides of the saphenous trunks. They connect the adventitia of the saphenous vein, run relatively parallel to the membranous layer and the muscle fascia and finally merge into them (white arrows in Fig. 2.4). This was confirmed by anatomical dissection where two layers of connective tissue were identified connecting the saphenous adventitia to the membranous layer and the muscle fascia (green arrows in Fig. 2.2). Using ultrasound, they are easier to see in the thigh for the great saphenous vein and in the upper calf for the small saphenous vein. Caggiati called them the “saphenous ligament” (Caggiati and Ricci 1999).
The envelopment of the saphenous veins by the saphenous compartment between the membranous layer and the muscle fascia and their anchorage by the saphenous ligament appear to be responsible for the lack of tortuosity observed when they become refluxive and dilated. This is in direct contrast to the behaviour of their refluxing tributaries.
2.3 The Foot Veins
For each toe, there are four veins, two dorsal and two ventral, which drain into the metatarsal veins. These in turn drain into the dorsal vein loop. The medial extension of this dorsal vein loop forms the origin of the great saphenous vein (Fig. 2.5), while the lateral extension forms the small saphenous vein (Fig. 2.6). The two veins are therefore haemodynamically connected by this loop. The dorsal vein loop on the foot also receives the marginal veins which connect the ventral and dorsal foot veins on the instep and lateral side of the foot.



Fig. 2.5
The medial part of the dorsal vein loop of the right foot (blue arrow) and its junction with the great saphenous vein. It is visible in front of the medial malleolus (white arrow)
Copyright: [Author]

Fig. 2.6
The lateral part of the dorsal vein loop of the right foot (blue arrow) and its junction with the small saphenous vein. It is visible behind the lateral malleolus (white arrow)
Copyright: [Author]
2.4 The Great Saphenous Vein
2.4.1 Course of the Great Saphenous Vein
The great saphenous vein is the longest vein in the body. It originates from the confluence of the dorsal foot veins on the medial side of the dorsal vein loop and runs consistently along the front of the medial malleolus where it can be seen or felt when standing (Fig. 2.5).
It continues medial to the edge of the tibia up to the knee. At first, it runs in a slightly posterior position, but at about a hand’s-breadth below the knee, it curves further posterior behind the medial femoral condyle (Fig. 2.7).


Fig. 2.7
Course of the great saphenous vein in right lower leg and knee
Copyright: [Author]
In its course along the thigh, it returns to a more ventral position reaching the inner third of the groin where it drains into the femoral vein (Figs. 2.8 and 2.9). Throughout its course, it rests on the muscle or deep fascia. It lies deep to the arch of the saphenous fascia (Sect. 2.4.2).



Fig. 2.8
Course of the great saphenous vein in the right thigh
Copyright: [Author]

Fig. 2.9
Course of the great saphenous vein in the whole right leg
Copyright: [Author]
At its upper end, the great saphenous vein drains into the common femoral vein at the saphenofemoral junction. Here, it curves down towards the deeper femoral vein where its path has been described as the “crosse” which is French for a bishop’s crook. The junction is located in the groin and is always distal of the inguinal ligament (Fig. 2.10).
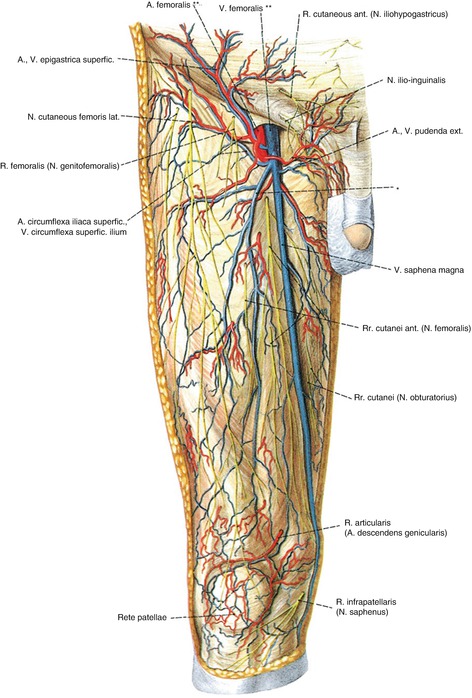
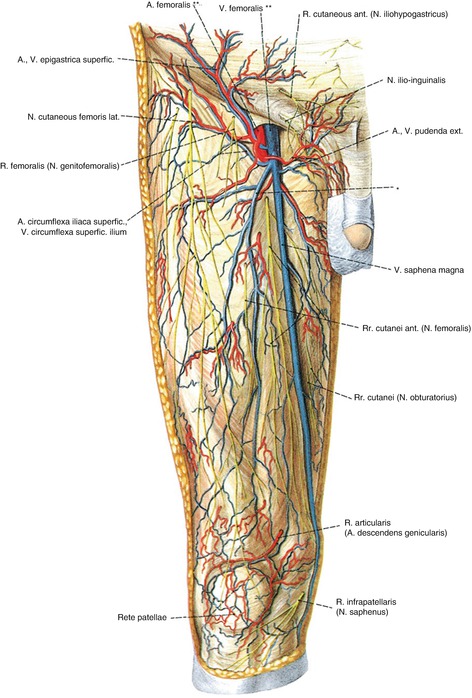
Fig. 2.10
Diagram of the saphenofemoral junction in the groin and its relation to the inguinal ligament. Anterior accessoric saphenous vein. (**) Common femoral artery and vein. (With kind permission from Paulsen, Waschke, Sobotta Atlas der Anatomie des Menschen, 23. Auflage 2010 © Elsevier GmbH, Urban & Fischer, München)
The saphenofemoral junction is the confluence of the great saphenous vein with the common femoral vein. As shown in Figs. 2.10 and 2.11, the “crosse” refers to the region of the saphenofemoral junction rather than the point of entry into the common femoral vein.
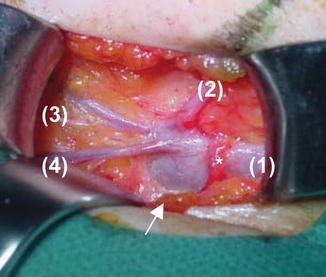
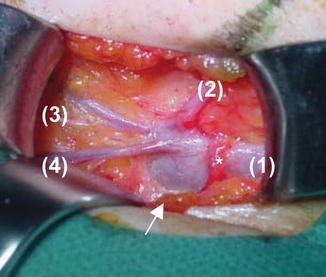
Fig. 2.11
Intra-operative picture of the saphenofemoral junction with the exposed saphenofemoral junction of the left leg (right = distal). The great saphenous vein (1) passes downwards through the saphenous hiatus (black arrow), a hole in the fascia, to join the common femoral vein. The region of the saphenofemoral junction contains the confluence of the anterior accessory saphenous vein (course marked on the skin in black 2), as well as those of the superficial circumflex iliac (3) and superficial epigastric veins (4). Also in the saphenofemoral junction region, the external pudendal artery crosses the great saphenous vein
Copyright: [Author]
The common femoral vein is a deep vein which runs below the deep fascia, while the great saphenous vein runs above the fascia. There is therefore an opening in the deep fascia, called the saphenous hiatus or oval foramen, through which the great saphenous vein passes immediately before it joins the deep vein. This saphenous hiatus allows the confluence of the great saphenous vein with the deep leg vein to be distinguished from confluences of other tributaries with the great saphenous vein when the saphenofemoral junction region is surgically exposed (Figs. 2.10 and 2.11).
A variable number of tributaries drain into the great saphenous vein in the groin, forming the confluence of superficial inguinal veins. Starting medial of the left great saphenous vein and going clockwise, these are the superficial external pudendal, superficial epigastric, superficial circumflex iliac, anterior accessory saphenous and posterior accessory saphenous veins (Figs. 2.10 and 2.11). The presence and form of the confluence of the individual veins are very variable and are described in more detail in Sect. 7.1.
In 88.5 % of cases, the great saphenous vein has a terminal valve in the region of its confluence. The distance of the terminal valve from the saphenofemoral junction varies between 0.0 and 1.4 cm. A preterminal valve is present in 89.2 % of cases, 1.4–8.2 cm from the saphenofemoral junction (in Mühlberger et al. 2009).
In the saphenofemoral junction region, the superficial external pudendal artery usually crosses the great saphenous vein from lateral to medial (Fig. 2.11).
2.4.2 Fascial Compartment of the Great Saphenous Vein
The membranous layer covers the great saphenous vein over its whole course, creating a tunnel from ankle to groin known as the saphenous compartment (Caggiati and Ricci 1999). In the distal part of the leg, the great saphenous vein is closely attached to both fasciae forming a compartment with a narrow tunnel. This broadens at the knee, and the distance over which the membranous layer is separated from the muscle fascia continues to broaden in the thigh (Figs. 2.12, 7.32 and 7.40). With normal amounts of fat, the great saphenous vein remains in constant contact with the two membranes. In this situation, the tunnel becomes broader with the corners of the eye further apart but the eye is no “wider open”. The broadening continues to increase up to the inguinal ligament, where the two membranes (membranous layer and muscle fascia) terminate, closing the upper end of the compartment.


Fig. 2.12
The fascial compartment of the great saphenous vein. The course of the great saphenous vein is drawn on the inner side of the leg. The green hatching shows the width of the saphenous compartment starting on the dorsal foot. It is very narrow along the lower leg, grows broader in the thigh and ends at the inguinal ligament where the two fasciae (muscle fascia and saphenous fascia) are joined
Copyright: [Author]
In the knee region, the membranous layer is poorly defined. Using ultrasound, it appears to be composed of several layers which are loose and open in places. This disruption may result from the forces placed on the knee joint.
The saphenous fascia in an anatomical preparation can be seen in Fig. 2.13.
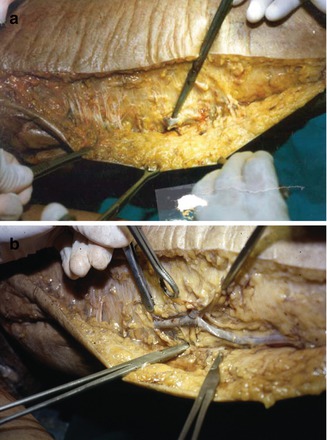
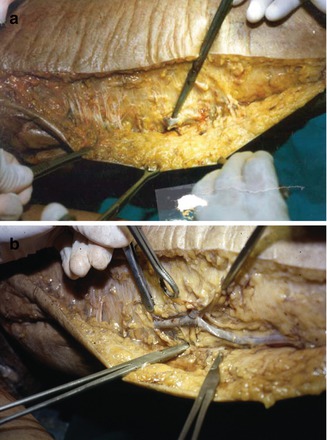
Fig. 2.13
The inner thigh of an anatomical preparation. (a) Inside of the left thigh where the skin and fat layers have been incised lengthwise and roughly separated from the saphenous fascia. The saphenous fascia has been opened at this point and the great saphenous vein lifted with a hook. (b) The saphenous fascia has been removed in the middle region revealing the great saphenous vein. To the left of the picture, the great saphenous vein disappears under the unopened tunnel of saphenous fascia (Prof. A. Caggiati, Rome; by kind permission)
Copyright: A. Caggiati, Rome
2.4.3 Duplication of the Great Saphenous Vein
From descriptions and from the histology of the veins in the saphenous compartment as compared with tributaries (Sect. 2.6), it may be concluded that only veins which course through the saphenous compartment really correspond to the great saphenous vein. Duplication of the great saphenous vein is therefore only present when both vessels course through the compartment (Fig. 2.14). Using this criterion, duplication of the great saphenous vein is only found in 1 % of patients (Table 2.1) (Ricci and Caggiati 1999). This is in contrast to the considerably higher figures published previously for duplication (27 %, Kubik 1985 in Appendix 2).
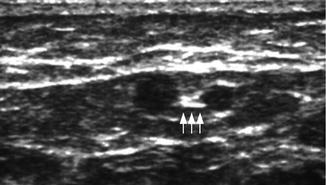
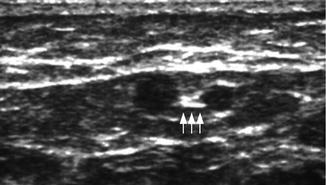
Fig. 2.14
Ultrasound view through the thigh showing a duplicated great saphenous vein. The two saphenous veins are bound together by the saphenous ligament (arrowed). It may be noted that the “eye” here is very wide; the corners are not visible in the transverse image because it is taken quite high up the thigh
Copyright: [Author]
Table 2.1
Classification of the courses of the great saphenous vein and its principal tributaries in the thigh as seen in ultrasound in 676 legs (Ricci and Caggiati 1999)
Type | Description | % |
|---|---|---|
A | One longitudinal vein visible running through the saphenous compartment | 52 |
B | Two longitudinal veins visible both in the saphenous compartment (true duplication) | 1 |
C | Two longitudinal veins visible, the saphenous vein in the compartment and one parallel to this which joins the great saphenous vein proximally | 26 |
D | Two longitudinal veins, one in the classic saphenous compartment and the other further ventral in the thigh, also in its own fascial eye. Proximally, these two saphenous eyes unite together | 10 |
E | Aplastic/hypoplastic segment of the great saphenous vein. A large vein in the subcutaneous fatty tissue pierces the saphenous fascia somewhere in the thigh and then continues as the great saphenous vein proximally | 11 |
True Duplication?
Epifascial, lengthwise tributaries can be distinguished clearly from saphenous veins by ultrasound. Ricci and Caggiati found these veins (superficial accessory veins) in 26 % of legs. They run parallel to the saphenous vein, but in the subcutaneous fatty tissue (Fig. 2.15). This is not duplication of the great saphenous vein. This configuration was previously evaluated as duplication before the discovery using duplex ultrasound of the difference between the great saphenous vein and other parallel veins on the basis of the saphenous fascia. If the 1 % of true duplication in the fascial compartment is added to the 26 % of great saphenous veins and superficial accessory saphenous veins with parallel courses, the result is the 27 % duplication rate given in the literature.
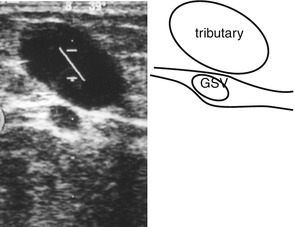
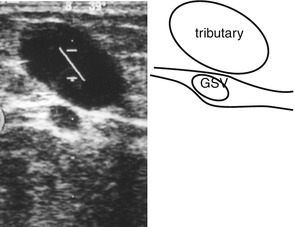
Fig. 2.15
Ultrasound view through the inner thigh showing the great saphenous vein and a parallel epifascial tributary. The sample volume cursor is seen in the epifascial refluxing tributary
Copyright: [Author]
2.4.4 Hypoplasia and Aplasia of the Great Saphenous Vein
In the groin region and proximal thigh, the great saphenous vein is fairly constantly seen in the fascial compartment. However, between the mid thigh and knee, the saphenous vein is absent from the saphenous eye in 15 % of legs: 12 % of patients with healthy veins and 24 % of patients with reflux (Caggiati and Mendoza 2004). This condition is described as a segmental aplasia of the great saphenous vein since histologically this vein is always present in the saphenous eye in rudimentary form (Caggiati 2000; Caggiati and Ricci 2000). In legs with segmental aplasia of the great saphenous vein, a large straight venous tributary is always visible in the subcutaneous fatty tissue, parallel to the empty saphenous eye. This joins the distal and proximal sections of the great saphenous vein and maintains the flow between them. Since this vein loop replaces the great saphenous vein functionally, it may be termed a functional great saphenous vein.
Great saphenous vein hypoplasia was defined by Caggiati when a segment of less than 3 mm in luminal diameter was found (Caggiati 2000).
Aplasia and Hypoplasia of the Great Saphenous Vein in the Literature
Ricci and Caggiati (1999) found that in 11 % of the 676 legs examined, there was no great saphenous vein in stretches of the fascial compartment. Instead, there was a vein running through the subcutaneous fatty tissue parallel to the expected course of the great saphenous vein. In these cadavers, Caggiati showed that a histologically rudimentary great saphenous vein with the same wall properties was present in the fascial compartment (Sect. 2.6; Caggiati et al. 1998). In a further survey (Caggiati and Ricci 2000), they found a reduction of >30 % of the calibre of the great saphenous vein in some segments in 20 % of legs. They conjectured that the aplasia/hypoplasia variants were associated with the formation of varicose veins because they were frequently found in legs with a refluxive great saphenous vein compared to legs with healthy veins.
Subsequent examinations by Mendoza and Mahdy (in Caggiati and Mendoza [2004]) showed that hypoplasia, defined as a reduction in the luminal calibre of the great saphenous vein to below 3 mm, has no statistical correlation with the occurrence of varices. This is in contrast to segmental aplasia where there is a weak relationship. Furthermore, in 15 % of patients and volunteers, the great saphenous vein between the knee and the mid thigh is not found in the fascial compartment under ultrasound. Instead, continuity between the proximal and distal parts of the aplastic segment is maintained by an extrafascial great saphenous vein which has pierced the fascia to become subcutaneous (Figs. 2.16 and 2.17).
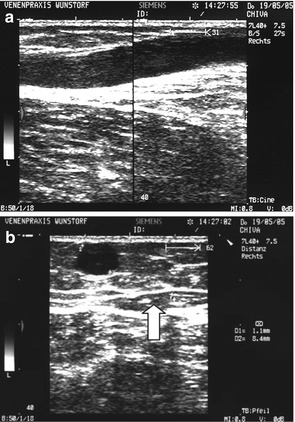
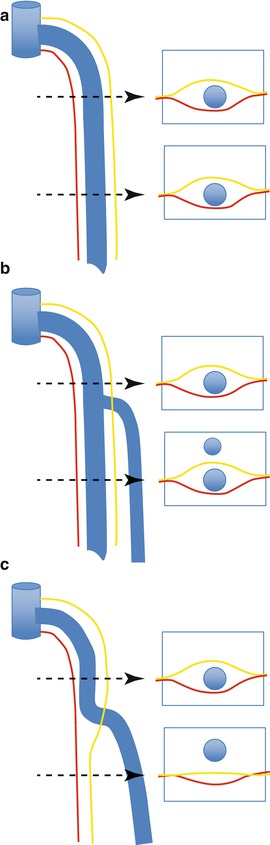
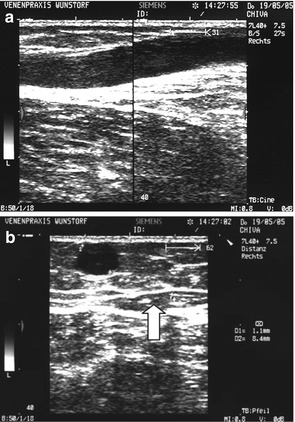
Fig. 2.16
(a) Longitudinal view of the inner thigh demonstrating the junction of the great saphenous vein with a tributary in segmental aplasia of the great saphenous vein. (b) Transverse view distal of this junction where the tributary runs in the subcutaneous fatty tissue and the saphenous eye is empty (arrow)
Copyright: [Author]
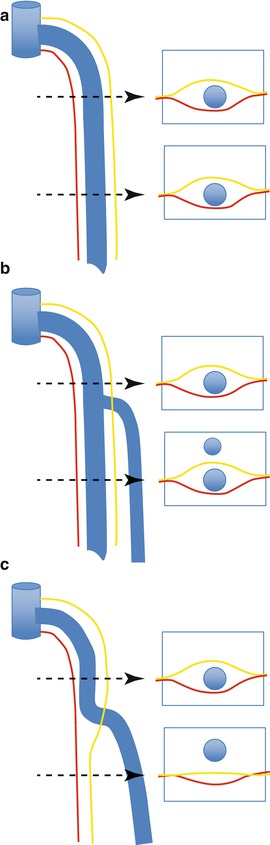
Fig. 2.17
The great saphenous vein and the variation in the connection of its tributaries. (a) The vein has a straight course within the saphenous fascia which is confirmed at bot h ultrasound points in the thigh. (b) A parallel extrafascial tributary is seen at the distal ultrasound point. (c) An aplastic segment is seen at the distal ultrasound point with the absence of a lumen in the fascia, “empty saphenous eye” and a replacement epifascial lumen
Copyright: [Author]
Segmental aplasia of the great saphenous vein is found in only 12 % of healthy legs. However, in legs with a refluxive great saphenous vein, an aplastic segment occurs in 24 %. The difference is statistically significant. This would indicate that segmental aplasia of the great saphenous vein is related with venous insufficiency, while hypoplasia is not (Caggiati and Mendoza 2004).
The classification of vein courses in the lower leg is difficult because they are more variable with many more tributaries. Interestingly, the great saphenous vein itself sometimes disappears completely. True duplications were not found in this region (Caggiati and Ricci 1999).
2.4.5 Tributaries of the Great Saphenous Vein
The great saphenous vein does not have very many described tributaries visible on ultrasound. However, in a pathological vein, more tributaries can be seen on ultrasound or contrast phlebography. It is also known from saphenous vein harvesting that a healthy vein has few tributaries (Caggiati 2000).
The tributaries are known as anterior and posterior arch veins in the lower leg region and as the anterior and posterior accessory saphenous veins in the thigh. These named veins are fairly constant in position.
The anterior arch vein in the lower leg runs from the lateral region of the foot via the lateral malleolus, proximal along the lateral edge of the tibia, and crosses the tibia at a variable height between halfway and one-third from the top. It joins the great saphenous vein in the upper third of the calf. Two anterior arch veins are occasionally found in the calf (Fig. 2.18).
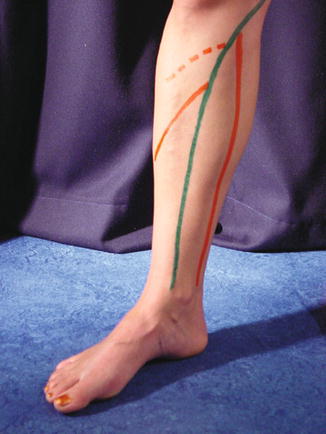
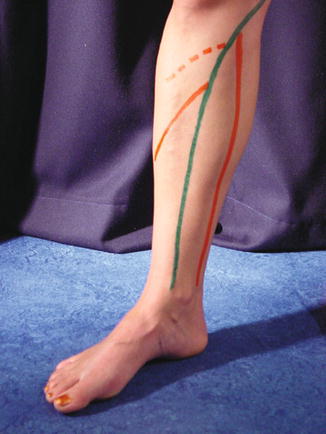
Fig. 2.18
Arch veins with a view of the inner side of the right calf. The course of the great saphenous vein is marked green. The anterior arch vein, marked in orange, enters just after it crosses the tibia. The dotted line is a frequent alternative and/or additional course of the arch vein. The posterior arch vein is marked medially, also in orange, along Linton’s line
Copyright: [Author]
The posterior arch vein originates posterior to the medial malleolus and runs fairly straight proximally along Linton’s line on the inside of the leg. It drains into the great saphenous vein below the medial femoral condyle. Most of the important pathological perforating veins in the calf lie along Linton’s line (Fig. 2.19 and Sect. 2.4.7).


Fig. 2.19




Postero-medial view of the calf demonstrating the inter-saphenous vein between the small and great saphenous veins in the calf (arrow). The posterior arch vein arises behind the medial malleolus and travels straight up to the great saphenous vein. The black dots represent the locations of the perforating veins. The numbers by the perforating veins show their distance in cm from the ground in a standing patient (4 medial ankle perforating vein, formerly Kuster perforating vein; 7 lower posterior tibial perforating vein, formerly Cockett 1, C1; 14 middle posterior tibial perforating vein, formerly Cockett 2, C2; 18 upper posterior tibial perforating vein, formerly Cockett 3, C3; 24 medial paratibial perforating vein in the mid lower leg, formerly Sherman perforating vein)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree