Diffuse Cystic Lung Diseases
W. Richard Webb
Acyst is a thin-walled, well-defined, air-containing lung lesion 1 cm or more in diameter. Cysts may be seen in patients with emphysema (i.e., bullae; see Figs. 24-3, 24-8, 24-12, and 24-13 in Chapter 24); honeycombing (i.e., large honeycomb cysts; see Fig. 10-17B in Chapter 10); pneumonia (i.e., pneumatoceles) (Fig. 25-1); cystic bronchiectasis (i.e., dilated bronchi) (Fig. 25-2; see also Fig. 9-28 in Chapter 9); subacute hypersensitivity pneumonitis; trauma with lung laceration (see Fig. 9-36 in Chapter 9); multiple healing cavities; and some parasitic infections (Table 25-1). The differential diagnosis (see Table 9-6 in Chapter 9) overlaps with that of multiple cavitary masses.
Several lung diseases are characterized by cysts as their primary abnormality. These are rare, and include Langerhans cell histiocytosis (LCH), lymphangiomyomatosis (LAM), tuberous sclerosis (TS), neurofibromatosis, lymphoid interstitial pneumonia (LIP), and Sjögren’s syndrome. Another rare disease, tracheobronchial papillomatosis, is discussed in Chapter 3.
PULMONARY LANGERHANS CELL HISTIOCYTOSIS (PULMONARY HISTIOCYTOSIS X)
The term Langerhans cell histiocytosis refers to a group of diseases of unknown etiology, most often recognized in childhood, in which Langerhans cell accumulations involve one or more body systems, including bone, lung, pituitary gland, mucous membranes and skin, lymph nodes, and liver. This disease also is known as histiocytosis X or eosinophilic granuloma (Table 25-2). Lung involvement in LCH is common, seen in 40% of patients, and may be an isolated abnormality. In patients with multisystem disease, other commonly affected sites include bone and the pituitary gland.
In the early stage, pulmonary LCH is characterized by the presence of granulomas containing large numbers of Langerhans cells and eosinophils, resulting in destruction of lung tissue. LCH lesions typically are peribronchiolar in distribution. In the later stages of the disease, the cellular granulomas are replaced by fibrosis and lung cysts. Although LCH is characterized by a clonal proliferation of cells, it is likely that LCH in adults represents an abnormal immune response in response to an unidentified antigenic stimulus rather than a neoplasm.
Most patients with pulmonary LCH are young or middleaged adults (average age, 32 years). Over 90% of adults with LCH are smokers, and this disease is considered to be related to smoking in most cases. Common presenting symptoms include cough and dyspnea. Up to 20% of patients present with pneumothorax.
Compared to patients with multisystem disease, the prognosis in patients with isolated pulmonary involvement is good; the disease regresses spontaneously in 25% and stabilizes clinically and radiographically in 50%. In the remaining 25% of cases, the disease follows a progressive downhill course, resulting in diffuse cystic lung destruction. In a small number of cases, death results from either respiratory insufficiency or pulmonary hypertension.
Radiographic Findings
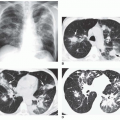
The radiographic findings of LCH include reticular, nodular, and reticulonodular patterns, often in combination (Figs. 25-3, and 25-4A and B); a cystic appearance may
mimic honeycombing. Abnormalities usually are bilateral, predominantly involving the middle and upper lung zones, with relative sparing of the costophrenic angles. Lung volumes are characteristically normal or increased (see Fig. 25-4A,B), an unusual appearance in the presence of reticular opacities or honeycombing.
mimic honeycombing. Abnormalities usually are bilateral, predominantly involving the middle and upper lung zones, with relative sparing of the costophrenic angles. Lung volumes are characteristically normal or increased (see Fig. 25-4A,B), an unusual appearance in the presence of reticular opacities or honeycombing.
TABLE 25.1 Multiple Lung Cysts | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
HRCT Findings
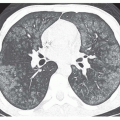
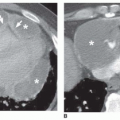
In almost all patients, HRCT demonstrates cystic air spaces, which are usually less than 10 mm in diameter (see Figs. 25-4,25-5 and 25-6). The lung cysts have walls, which range from being thin and barely perceptible to several millimeters thick. The presence of distinct walls makes it possible to differentiate these cysts from areas of emphysema. Although many cysts appear round, they can also have bizarre shapes, being bilobed or clover-leaf in appearance (see Figs. 25-4,25-5 and 25-6). An upper lobe predominance in the size and number of cysts is common (see Figs. 25-4 and 25-6). Large cysts or bullae (more than 10 mm in diameter) are seen in more than half of cases; some cysts are larger than 20 mm. True honeycombing, often suggested by the chest radiograph, does not occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree