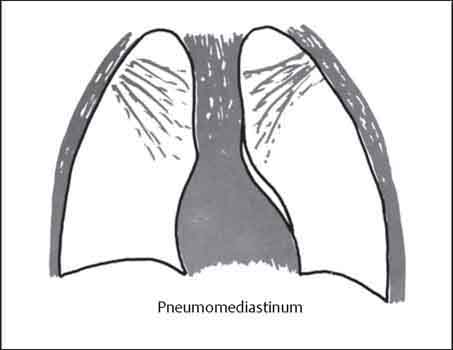
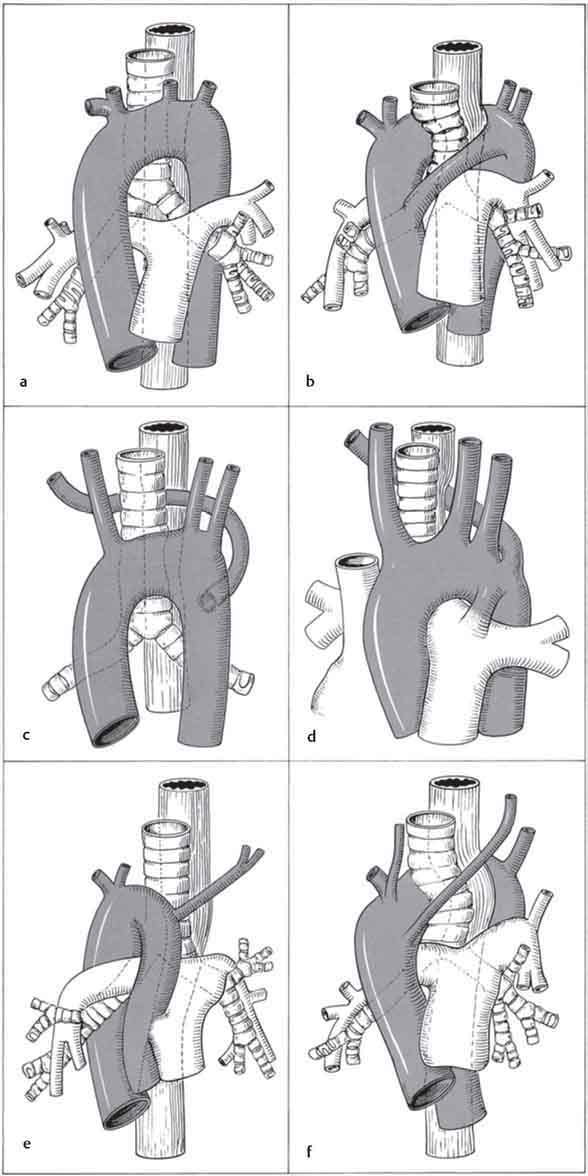
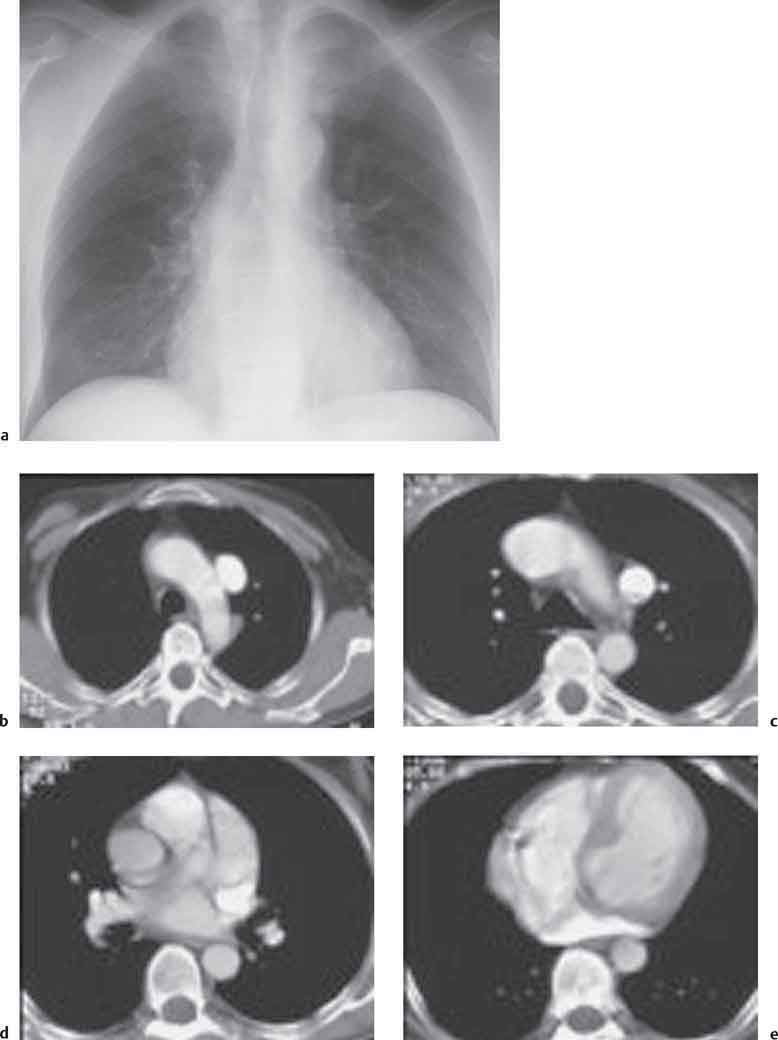
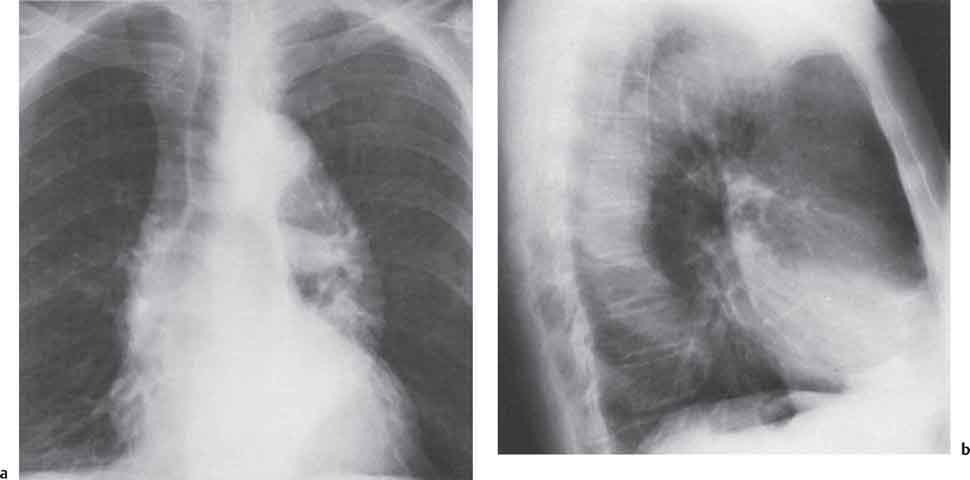
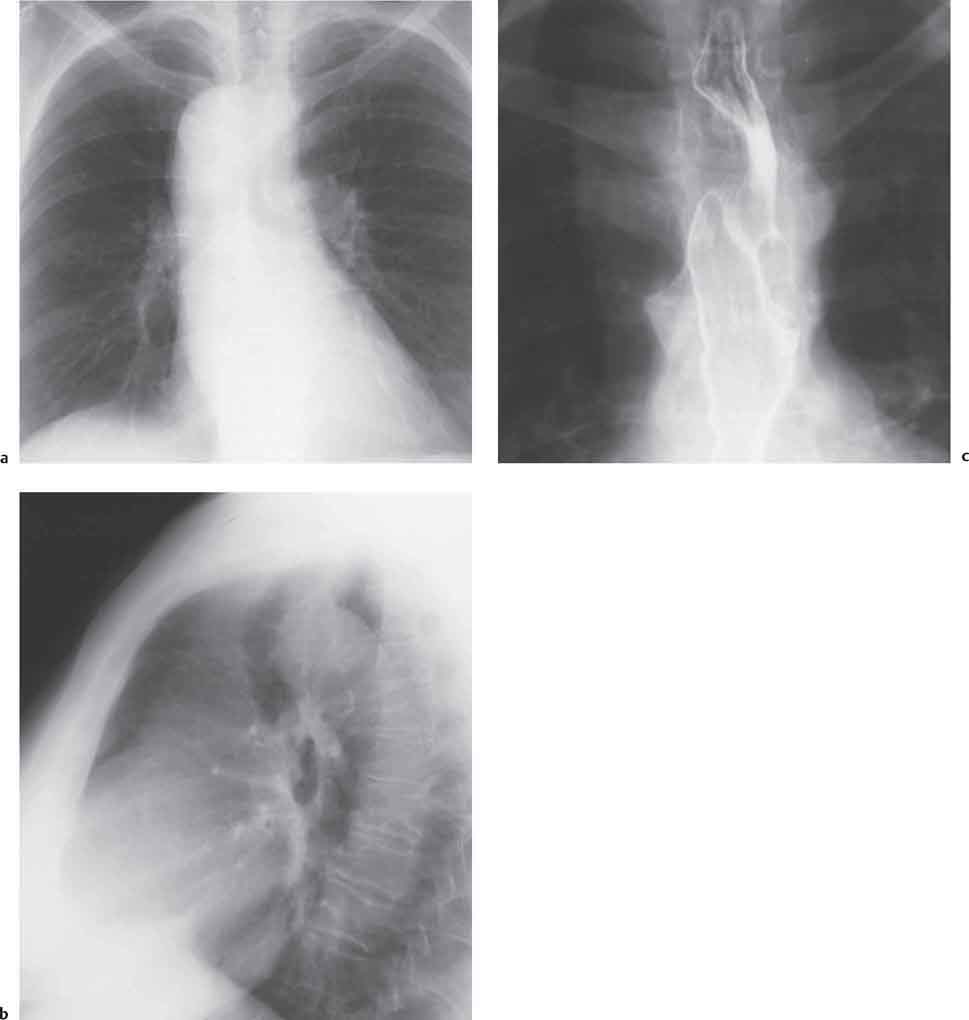
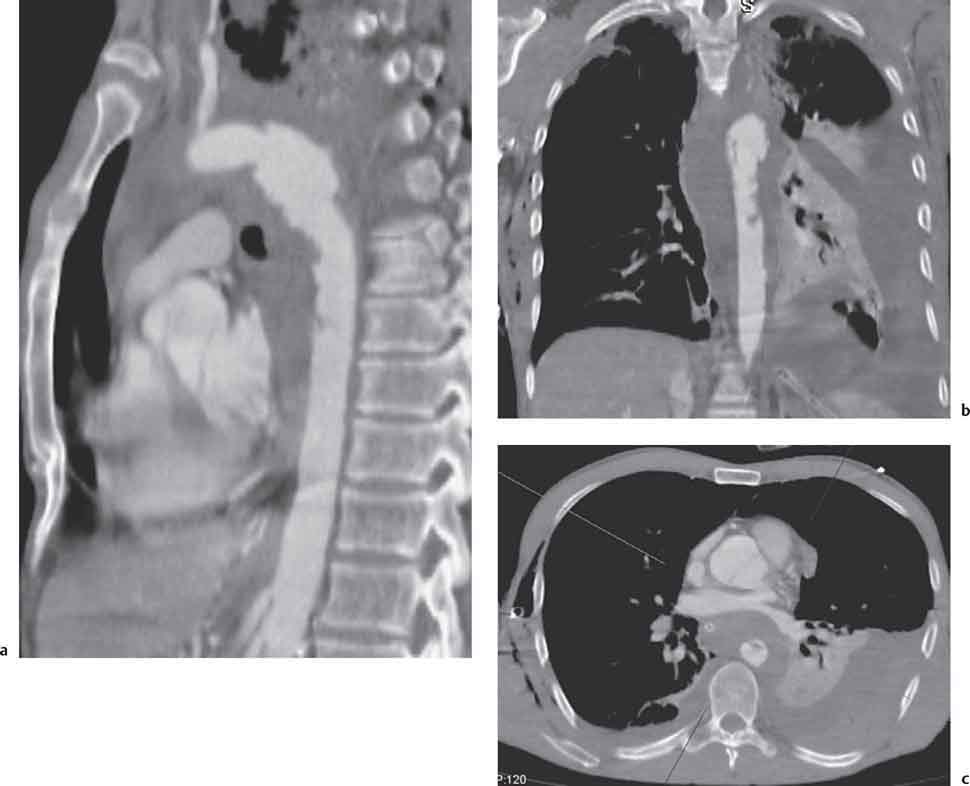
11 Diseases of the Mediastinum The mediastinum is bordered anteriorly by the sternum, posteriorly by the thoracic vertebral column, and laterally by the mediastinal pleura. Its contents include the heart, esophagus, trachea, thyroid gland, thymus, major nerves, and vascular structures. Complete mediastinal displacement results in asymmetric pulmonary expansion. More localized mediastinal displacement results in unilateral extension of a pleuropulmonary recess across the midline. These localized displacements frequently result from pulmonary atelectasis and usually involve the anterior or posterior mediastinum (Fig. 11.1). Mediastinal displacement may be fixed when the differential diagnosis includes: or dynamic when there is mediastinal shift during the respiratory cycle and when the differential diagnosis includes: Fig. 11.1 Air in the mediastinum. Occasionally, swallowed air may be identified within the esophagus; it is recognized by visualization of the left esophageal wall separate from the azygoesophageal stripe. Megaesophagus, esophageal diverticula, hiatus hernia, and communicating esophageal duplication cysts may also appear radiographically as air-containing lesions. Air from ruptured alveoli dissects along the peribronchovascular connective tissue planes into the adjacent mediastinum (Figs. 11.2, 11.3). Alveolar rupture is usually a consequence of marked increases in intra-alveolar pressure during mechanical ventilation, severe bouts of coughing, or acute exacerbations of asthma. Blunt chest trauma with rupture of the esophagus or tracheobronchial tree will also result in pneumomediastinum (Table 11.1). Fig. 11.2 Pneumomediastinum. Table 11.1 Causes of pneumomediastinum Fig. 11.3 Pneumomediastinum. Air column separates the visceral from the parietal layers of the mediastinal pleura. Frequently, there is associated deep cervical and subcutaneous chest wall emphysema. Occasionally, a large pneumomediastinum may lead to impaired systemic venous return and respiratory compromise. See Chapter 8, p. 210. Mediastinal widening is a common radiographic finding. Anteroposterior (AP) supine views taken in shallow inspiration or expiration lead to foreshortening of mediastinal structures and to apparent widening of the mediastinum. Causes of pathologic mediastinal widening include mediastinal hemorrhage and inflammation, esophageal, aortic and vascular dilatation, and lymph node enlargement. Acute mediastinitis is a serious though rare pathologic process with a mortality rate approaching 50%. Initial diffuse purulent inflammation progresses to abscess formation and these are frequently multiple. Mediastinitis may be secondary to esophageal perforation or postoperative infection. Less commonly it results from direct spread of infection from the retropharyngeal space, lung, or from suppurative mediastinal lymph nodes. These patients tend to be very ill with severe retrosternal chest pain and pyrexia. When esophageal perforation is present, there is associated dysphagia and deep cervical emphysema. The chest radiograph shows mediastinal widening with obliteration of fat planes, an accompanying pneumomediastinum, and associated unilateral or bilateral pleural effusions. In diffuse mediastinitis, computed tomography (CT) shows diffuse soft tissue infiltration of the mediastinum with loss of the normal fat planes. When there is progression to abscess formation, gas bubbles and air-fluid levels may be seen within discrete collections (Armstrong 1995). Upper gastrointestinal contrast swallow using low osmolar water-soluble contrast medium will show leakage of contrast into the mediastinum from an esophageal perforation. Chronic mediastinitis is a granulomatous inflammatory disorder which may progress to fibrosis. Known causes include tuberculosis and in the United States, histoplasmosis. However, many cases are of unknown etiology. Idiopathic mediastinal fibrosis may be of autoimmune etiology and there may be an association with retroperitoneal fibrosis (Ormond disease). Patients may initially be asymptomatic. Symptoms usually result from stenosis or occlusion of the superior vena cava or from extrinsic narrowing of the esophagus and tracheobronchial tree. The chest radiograph usually shows mediastinal widening ± calcification in cases of histoplasmosis. Other findings are determined by the severity of the obstructive phenomena and include pulmonary oligemia if a pulmonary artery is involved. Narrowing of the trachea and major bronchi may also be seen. Computed tomography will demonstrate soft tissue infiltration of the mediastinum and there maybe airway and vascular encasement. Dilated collateral vessels also may be present. The thoracic aorta runs cranially in the anterior mediastinum (ascending aorta) from its origin at the aortic valve, curves posteriorly over the left main bronchus to form the aortic arch, and passes caudally to the diaphragm (descending aorta). The normal diameters based on CT data are: The aortic isthmus lies just distal to the origin of the left subclavian artery at the level of the ligamentum arteriosum. Coarctation of the aorta has been discussed in Chapter 10, p. 244. Fig. 11.4a–f Aortic and great vessel anomalies (modified from Schinz 1983). a Normal left-sided aortic arch. b Double aortic arch. c, d Left aortic arch with an aberrant right subclavian artery. c Right subclavian artery crossing the mediastinum between the trachea and esophagus. d Right subclavian artery crossing behind the esophagus. Other common anomalies include (Figs. 11.4–11.6): Fig. 11.5a–c Right aortic arch, posterior type. Note the displacement of the trachea (b) and the indentation of the esophagus (c). This patient had presented clinically with dysphagia lusoria. Loss of normal vessel elasticity results in aortic dilatation and ectasia; associated changes may be found in the aortic valve. This degenerative process is common in the elderly and eventually may result in aneurysmal dilatation (Higgins 1992, Fig. 11.7). Fig. 11.6a–e Persistent left superior vena cava. Note the low density widening of the superior mediastinum on the chest radiograph (a). CT defines the course of the persistent left SVC through to the coronary sinus (b–e). An aneurysm is a saccular or fusiform dilatation of the aortic lumen to greater than 5 cm in diameter. It may be due to atherosclerosis (especially in individuals with systemic arterial hypertension), aortitis in patients with syphilis, some vasculitides including Takayasu’s disease and cystic medial necrosis in Marfan’s syndrome. Inflammatory aneurysms have a predilection for the ascending aorta while atherosclerosis most commonly involves the descending aorta. Fig. 11.7a, b Elongated, ectatic thoracic aorta. Fig. 11.8a–c Traumatic aortic injury with rupture giving hemothorax and mediastinal hemorrhage. Classic aortic dissection is an emergency which requires prompt diagnosis and treatment (Pretre et al. 1997). Blood dissects between the intima and media through an intimal tear; this separates the layers and creates a false lumen that may reunite with the true lumen at a more distal level. Aortic dissections may be acute (first 2 weeks) or chronic (Crawford 1990). Sites of predilection are the proximal ascending aorta just superior to the valve ring and the region of the aortic isthmus. It is important to determine if a dissection is limited to the descending aorta (type B dissection) or if it also involves the ascending aorta and the origins of the great vessels (type A dissection, Fig. 11.10). Intramural hematoma may be an early stage or a variant of aortic dissection (Yoshida et al. 2003). Many authors distinguish between aortic dissection and intramural hematoma by the presence or absence of an intimal flap (Maraj et al. 2000). Intramural hematoma is also classified as type A or B depending on its location and extent. Ulcer-like projection/penetrating atherosclerotic ulcer. An ulcer-like projection is defined at CT and angiography as a localized blood-filled pouch protruding into the thrombosed wall of the aorta and showing the same degree of contrast enhancement as the aortic lumen. They may develop in both types A and B intramural hematoma.
Mediastinal Displacement
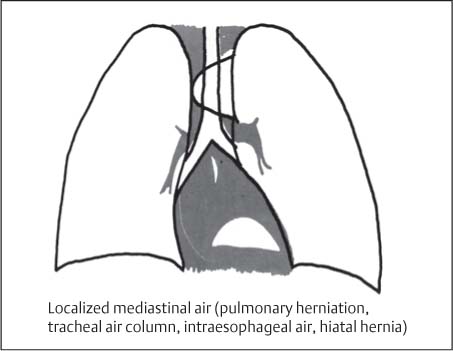
Air in the Mediastinum
Air in the Esophagus and Stomach
Pneumomediastinum
Traumatic
Pulmonary contusion and pneumothorax
Bronchial rupture
Spontaneous
Acute exacerbation of asthma
Pneumonia (especially in children)
Acute mediastinitis with gas-forming organisms
Spontaneous esophageal rupture (Boerhaave syndrome)
Iatrogenic
Tracheotomy
Positive-pressure ventilation
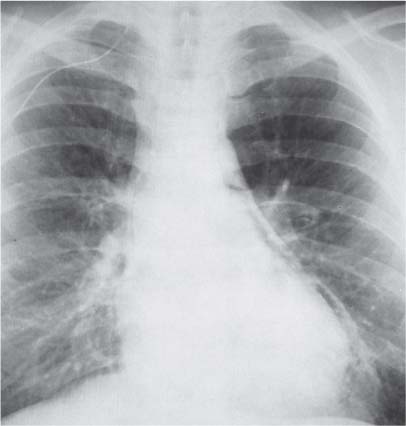
Radiologic Findings
Non-Neoplastic Mediastinal Widening
Acute Mediastinitis
Radiologic Findings
Chronic Mediastinitis
Radiologic Findings
Diseases of the Thoracic Aorta
Aortic Anomalies
e Right aortic arch, anterior type. f Right aortic arch, posterior type.
Aortic Ectasia
Thoracic Aortic Aneurysm and Dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree