(1)
Department of Radiology, John H Stroger Jr Hospital of Cook County, Chicago, IL, USA
Pancreatitis
Imaging Features
A.
Less than 4 weeks after onset
1.
Interstitial edematous pancreatitis—acute peripancreatic fluid collection, sterile or infected
2.
Necrotizing pancreatitis
(a)
Parenchymal necrosis alone
(b)
Peripancreatic necrosis alone
(c)
Pancreatic and peripancreatic necrosis
B.
More or equal to 4 weeks
(a)
Interstitial edematous pancreatitis with pseudocyst (sterile or infected)
(b)
Necrotizing pancreatitis with walled-off necrosis (sterile or infected)
Diagnosis
Interstitial Edematous Pancreatitis
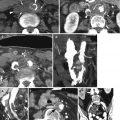
Fig. 13.1
Interstitial edematous pancreatitis. Axial postcontrast CT (a) examination done a few years earlier shows normal pancreas. (b) CT done for suspicion of pancreatitis shows pancreatitis with diffuse increased enhancement of the pancreas with mild increase in size and minimal peripancreatic inflammation. (c) Examination done 5 months later shows increase in inflammation involving the transverse mesocolon (thin arrow) and peripancreatic fluid collection in the anterior pararenal space (thick arrow). (d) Axial CT done 2 weeks later shows improved peripancreatic inflammation and fluid collection. (e) T1W MRI and (f) postcontrast fat-saturated T1 MRI done at the same time as (d) show improved pancreatitis with minimal mistiness of surrounding fat (arrow)
Fig. 13.2
Interstitial edematous pancreatitis. Axial postcontrast CT (a, b) shows localized enlargement of the pancreatic tail (thick arrow) with diffuse enhancement of the body and tail and surrounding acute peripancreatic fluid collection (thin arrow). (c) Coronal reformatted image shows increased enhancement of the head of the pancreas (black arrowhead) and edema of the adjacent duodenum (white arrowhead), fluid in the pancreaticoduodenal groove (black arrow), and around the tail of the pancreas (white arrow)
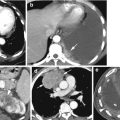
Fig. 13.3
Peripancreatic necrosis alone. Postcontrast CT (a) axial image shows normal homogeneous pancreatic enhancement. (b, c) Axial CT and coronal reformatted images show normal size of the head and uncinate process (black arrow). Extensive acute heterogeneous nonliquified inflammation in the right anterior pararenal space (white arrow), root of mesentery, and transverse mesocolon with edema in right-sided subcutaneous tissue. (d, e) Axial and coronal reformatted CTs show diffuse inflammation around the root of the mesentery (black arrowhead) and transverse mesocolon (thick white arrow) causing luminal narrowing of the right colon with wall edema, extending inferiorly to the perirenal space (white arrowhead) and APS laterally (thin head). Fluid is tracking down to the pelvis in the APS (black arrow)
Diagnosis
Necrotizing Pancreatitis
Fig. 13.4
Necrotizing pancreatitis with acute necrotic collections. (a) Axial CT image shows a diffusely enlarged nonenhancing body and tail of the pancreas with patchy areas of enhancing pancreatic tissue (arrow) and diffuse surrounding peripancreatic necrotic collection. Axial CT (b) and (c) coronal reformatted images show acute peripancreatic necrotic collection which is faintly heterogeneous, in bilateral anterior pararenal spaces (arrow). (d, e) Axial and coronal reformatted CTs 3 weeks later show large necrotic collection in the lesser sac (arrows) between the necrotic pancreas (arrowheads) and contrast-filled stomach
Fig. 13.5
Necrotizing pancreatitis with peritonitis. Same patients as in Fig. 13.4 about 5 weeks later. CECT axial (a, b) and coronal reformatted images (c) show nearly complete necrosis of the body and small residual tail of the pancreas (short white arrow). Large pseudocyst in the lesser sac with enhancing wall (black arrowhead) adjacent to the head (black arrow) and tail of the pancreas and diffuse reactive peritonitis with enhancement of the peritoneum (long white arrows) and large ascites. The abdominal wall shows diffuse edema
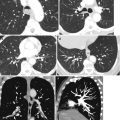
Fig. 13.6
Acute necrotizing pancreatitis. Contrast-enhanced CT axial (a, b) and coronal reformatted images show necrosis of the tail of the pancreas (thick white arrow) with surrounding heterogeneous acute necrotic collection (thin white arrows in a, b) with fluid and necrotic material in the left anterior pararenal space (long thin arrow), causing thickening of the lateroconal fascia (arrowhead) and posterior renal fascia (short thin arrow in c)
Fig. 13.7
Walled-off necrosis. History of recent resection of the body and tail of the pancreas. CECT (a, b) axial CT, (c) coronal, and (d) sagittal reformatted images show loculated fluid collection in the region of the resected body and tail of the pancreas (black arrow) which has ruptured (white arrows) into the lesser sac. The lesser sac collection (arrowheads) shows areas of low-density fat necrosis and areas of higher density and with faint surrounding rim of loculation. About 8 weeks later, (e) axial CT shows pseudocyst formation of the WON (arrow) with wall enhancement and superimposed infection with gas collections (arrowhead). (f, g) Axial and sagittal reformatted images show focal perforation (black arrowhead) of the pseudocyst wall with gas (white arrowhead) and fluid (black arrowhead) extending into the abdominal wall
Diagnosis
Gallstone Pancreatitis


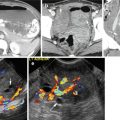
Fig. 13.8
Gallstone pancreatitis. Axial contrast-enhanced CT shows calcified stone in the distal common bile duct at the head of the pancreas (thin black arrow). The head of the pancreas is enlarged with heterogeneous enhancement (long thick white arrow) with diffuse peripancreatic inflammatory changes (thin white arrow). The second part of the duodenum shows reactive dilatation and wall thickening (black arrowhead)
Diagnosis
Groove Pancreatitis
Imaging Features
1.
Soft tissues or fluid within the pancreaticoduodenal groove.
2.
Small cystic lesions may be seen along the medial wall of the duodenum.
Fig. 13.9
Groove pancreatitis in a patient with a history of alcohol abuse. Axial (a) and coronal reformatted (b) CT show fluid in the pancreaticoduodenal groove. The second part of the duodenal sweep shows mucosal enhancement. Cystic lesions are attached to the medial wall of the duodenum (arrow). (c) Axial CT done 5 months later shows dense scar tissue in the groove with decreased size of the cystic lesions (arrow). Endoscopic study showed periampullary mass, biopsy of which showed acute and chronic inflammation