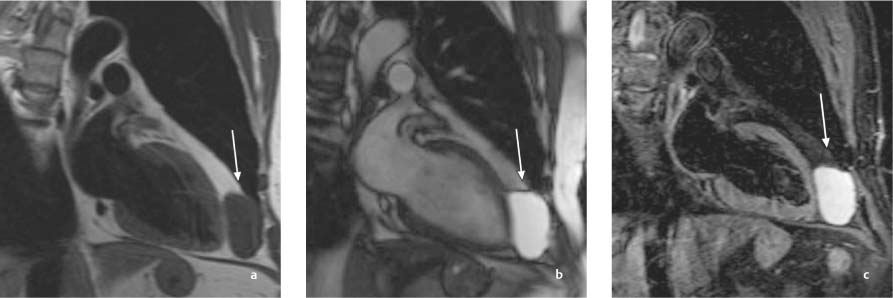
11 Diseases of the Pericardium The pericardium is a fluid-filled, double-walled fibrous sac ~1 mm thick that encloses the heart. Like the pleura and peritoneum, it consists of an outer, parietal pericardial layer and an inner, visceral epicardial layer that covers the heart. Normally these two layers are separated by a fluid film of ~20 to 50 mL that allows smooth movement of the heart during systole and diastole. The parietal layer of the pericardium is attached anteriorly to the chest wall, posteriorly to the thoracic spine, and inferiorly to the diaphragm. Superiorly, the pericardium extends onto the proximal portions of the great vessels, forming a broad fold close to the ascending aorta at the level of the tracheal bijurcation. The pericardium is innervated by the vagal and phrenic nerves, and it drains to the mediastinal and axillary lymph nodes by small pericardial lymph vessels.1,2 Both the outer and epicardial surfaces of the pericardium are surrounded by copious fat, making it easier to identify the pericardium as a thin, fat-embedded membrane on CT and MR images. Healthy pericardium is almost never delineated from the epicardium on echocardiograms because it has the same echogenicity as surrounding structures. The normal pericardium cannot be identified as a separate structure on frontal and lateral chest radiographs3 (see Pericardium, p. 25). Plain films may, however, show tent- or bottle-shaped widening of the cardiac silhouette as evidence of pericardial effusion. This may be indistinguishable from global cardiac enlargement in heart failure, although this condition is associated with enlarged central pulmonary vessels and interstitial fluid accumulation in the lung, allowing differentiation from pericardial effusion.4 Calcifications of the pericardium are easily identified on chest films and do not necessarily indicate a constrictive disease of the pericardium. Finally, a circumscribed bulge in the cardiac outline on the chest film may indicate herniation of myocardial tissue through a pericardial defect.5 With left-sided aplasia of the pericardium, the heart will be displaced toward the left side and will show increased mobility. Echocardiography is the first diagnostic test for evaluation of the pericardium, especially in patients with suspected pericardial effusion. The dynamic information provided by real-time M-mode, B-mode and Doppler imaging allows for detection of pathological changes in the setting of pericardial diseases. The diagnosis of effusion in the pleural or pericardial space was one of the first major applications of M-mode echocardiography. Two-dimensional echocardiography has improved the diagnosis and quantification of pericardial effusions. A pericardial effusion appears on echocardiography as a hypoechoic zone between the epicardium and pericardium. A circumferential effusion can be distinguished from a localized effusion with reasonably high confidence. Difficulties may arise in differentiating between a pleural and pericardial effusion. This can be aided by noting how the effusion is projected relative to the descending aorta in the parasternal view. A posterior pericardial effusion is typically projected between the left atrium and descending aorta in this view, while a pleural effusion is not.1 In the absence of an effusion, however, it may be impossible to delineate the pericardium by echocardiography. It is also difficult to detect pericardial defects. Pericardial calcifications increase the echogenicity of the pericardium, causing the pericardial echo to appear brighter than the surrounding tissue. This finding is relatively nonspecific, however. CT is also used in the diagnosis of pericardial diseases. The pericardial fold close to the ascending aorta should not be misinterpreted as an enlarged lymph node. The pericardium is clearly distinguished from surrounding fat by the difference in attenuation values. This makes it easy to detect focal areas of wall thickening,6 although these sites may be difficult to distinguish from loculated areas of pericardial effusion. When imaged by CT, a pericardial effusion appears as a hypodense stripe that generally encircles the heart. CT is the most accurate imaging modality for the detection of pericardial calcifications.7 Moreover, the use of iodinated contrast media can not only differentiate between cardiac chambers, great vessels, and coronary arteries but can also detect inflammations and circumscribed neoplasms by their increased contrast uptake, although this enhancement is not a specific sign. MRI is most favorable for pericardial imaging owing to its intrinsically high soft-tissue contrast and its high temporal and spatial resolution for structural delineation and functional analysis.4 As in CT, ECG triggering should be used for data acquisition. It should be noted, however, that pleural and pericardial effusions may cause a decreased or wavy amplitude of the QRS complex (electrical alternans), which may hamper detection of the ECG signal for optimal data acquisition. Large pericardial effusions can be detected even without ECG gating in examinations of the chest or abdomen for noncardiac indications. In most cases this can be done with T2-weighted sequences, in which an effusion appears hyperintense within the pericardium. However, pericardial effusion may also have low signal intensity or produce a signal void on T2-weighted images when turbo spin-echo sequences are used and especially in sequences with dark-blood preparation. The low signal intensity in these images results from fluid motion driven by cardiac pulsations. The signal characteristics of pericardial effusions may vary in the case of encapsulated effusions, blood collections, or proteinaceous effusions. Calcifications appear as signal voids on MRI and are detected less sensitively than by CT.8 Dynamic cine sequences (SSFP) can document cardiac and pericardial movements. Also, Gd-based contrast agents make it possible to detect inflammatory and neoplastic changes owing to increased contrast uptake in those areas. Echocardiography is the initial imaging study used in case of suspected pericardial disease, whereas the chest radiograph contributes only little information. Sectional imaging modalities like CT and MRI, however, permit the most accurate morphological analysis of pericardial diseases. While pericardial cysts may be congenital or acquired, pericardial diverticula develop as a result of increased intracardiac pressure or adhesions. Both cysts and diverticula are located in immediate proximity to the pericardium. Cysts are often located in the right cardiophrenic angle, while diverticula often occur over the right atrium on the outer cardiac surface or in the left cardiophrenic angle.9 Pericardial cysts are fluid-filled cavities that do not communicate with normal pericardial fluid and may be encapsulated by pericardium (Figs. 11.1, 11.2). Pericardial diverticula result from increased pressure in the pericardial cavity or from scar traction (e. g., after trauma or surgery) sufficient to cause a fluid-filled outpouching of the pericardium. Pericardial cysts and diverticula have no hemodynamic effects and do not interfere with cardiac filling. Most pericardial cysts and diverticula are detected incidentally at imaging. Aside from an occasional retrosternal pressure sensation, patients are asymptomatic. Whereas diverticula are definitely benign and rarely cause incarceration of cardiac structures, surgical removal may be considered for pericardial cysts to exclude other potentially malignant cystic tumors. Chest radiographs may demonstrate a round paracardiac opacity (Fig. 11.2), which can be further analyzed fluoroscopically for its mobility and deformation during respiratory excursions.4 M-mode echocardiography is of little importance in the detection of cysts or diverticula. On 2D imaging, cysts and diverticula usually appear as extraneous cavities on the pericardium that contain low-level internal echoes and undergo pulsatile movements. Intracardiac and extracardiac masses can be differentiated by administering a transpulmonary ultrasound contrast agent. The agent will opacify the cardiac chambers while sparing extracavitary masses.1 Pericardial cysts and diverticula have the following CT features: • Smooth-walled, hypodense mass bordering the pericardium • Homogeneous (simple) or inhomogeneous density (complicated) • Typically no contrast enhancement • Occasional wall calcifications MRI of simple pericardial cysts shows a rounded, smooth-walled mass with a uniformly hyperintense internal structure on T2-weighted images (Fig. 11.1). Complicated cysts have inhomogeneous signal intensity owing to intracystic hemorrhage, septa, or protein-rich fluid. Complicated cysts may enhance after IV contrast administration, making them difficult to distinguish from other cystic tumors.7,9 As a sectional imaging modality, MRI can additionally demonstrate locoregional lymph nodes and changes in the lung parenchyma. Fig. 11.1a–c Vertical long-axis MRI in a patient with a pericardial cyst. Anterior to the cardiac apex a well-circumscribed mass (arrow) with low signal intensity on the T1-weighted image (a) and homogeneous high signal intensity on the SSFP sequence (b) can be detected. The lesion is isointense to fluid on the fat-suppressed T2-weighted image (c). • Pericardial and paracardiac fat pads or lipomas • Bronchogenic cysts • Aneurysms • Hernias, especially hiatal hernias and “upside-down stomach” • Achalasia • Other mainly cystic tumors arising from the mediastinum, diaphragm, pericardium, or pleura The causes of chronic and acute pericarditis are diverse. Possible causes include viral and bacterial infections, previous cardiac surgery, previous myocardial infarction, neoplasms, systemic diseases, chronic renal failure, and many others.7–9 The various causes of acute and chronic pericarditis are summarized in Table 11.1. A fibrinous (dry) form is distinguished from an exudative (wet) form that is associated with effusion. In fibrinous pericarditis, adhesions may form between the pericardial layers, restricting the motion of the pericardium and interfering with cardiac filling. Chronic forms are characterized by recurrent effusions, adhesive plaques, calcifications, and an audible pericardial friction rub. The diagnosis of pericarditis is based on typical clinical symptoms, ST segment changes, and the presence of a pericardial friction rub. A pericardial effusion is not always detected initially but will usually develop during the course of the disease. Pericardial effusion in pericarditis initially forms in the posterior portion of the pericardium. It then spreads across the anterior wall to the base of the heart and eventually fills the space behind the left atrium (late stage). The distance from the pericardial effusion to the chest wall should be measured, as it may be important in planning a safe ultrasound-guided pericardiocentesis, for example.
Anatomy
Imaging Modalities
Chest Radiographs
Echocardiography
Computed Tomography
Magnetic Resonance Imaging
 Essential Point
Essential Point
Specific Diseases
Pericardial Cysts and Diverticula
Anatomy and Pathophysiology
Imaging
Differential Diagnosis
Pericarditis
Pathophysiology and Clinical Features
• Idiopathic • Infectious (bacterial, viral, fungal, parasitic, tuberculous) • Myocardial infarction • Allergic • Rheumatic • Autoimmune systemic diseases (especially collagen diseases: chronic rheumatoid arthritis, Reiter disease, ankylosing spondylitis, Sjögren disease, Felty disease, lupus erythematosus, scleroderma, dermatomyositis, panarteritis nodosa) • Sarcoid • Metabolic (renal failure, hypothyroidism, Addison disease, diabetes mellitus, hypercholesterolemia) • Posttraumatic, postoperative • Neoplastic (including leukemia and myeloma) • Dissecting aneurysm of the ascending aorta • Postradiogenic • Chylogenic (e.g., due to fistula formation) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree