Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
16.1 Inflammatory Lesions
16.1.1 Acute Peritonitis
16.1.2 Granulomatous Peritonitis
16.2 Tumor-Like Lesions
16.2.1 Peritoneal Inclusion Cysts
16.2.2 Splenosis (Figs. and )
16.3.1 Localized Neoplasms
16.3.2 Diffuse Neoplasms
16.4 Metastatic Tumors
16.4.3 Pseudomyxoma Peritonei
16.5.4 Leiomyomatosis
Abstract
Acute diffuse peritonitis is characterized by serosal fibrinopurulent exudates. It is most commonly associated with a perforated viscus. Rare infectious causes include candida and actinomycetes.
16.1 Inflammatory Lesions
16.1.1 Acute Peritonitis
Acute diffuse peritonitis is characterized by serosal fibrinopurulent exudates. It is most commonly associated with a perforated viscus. Rare infectious causes include candida and actinomycetes.
Localized acute peritonitis may be secondary to appendicitis (Fig. 16.1), sigmoiditis (Figs. 16.2 and 16.3), or can be associated with PID (Fig. 16.4).
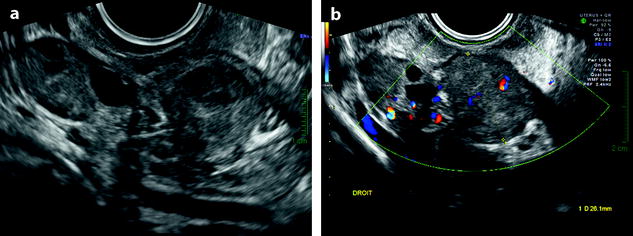
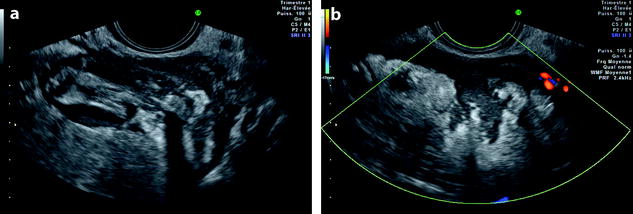
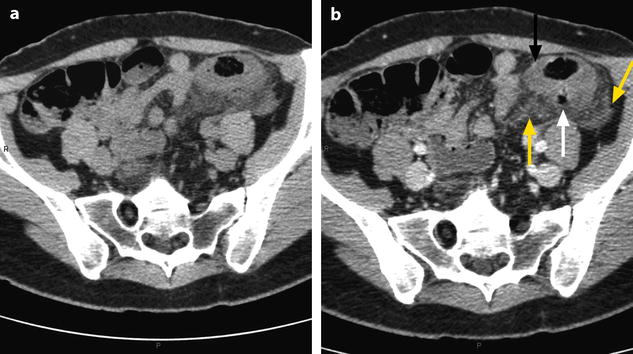
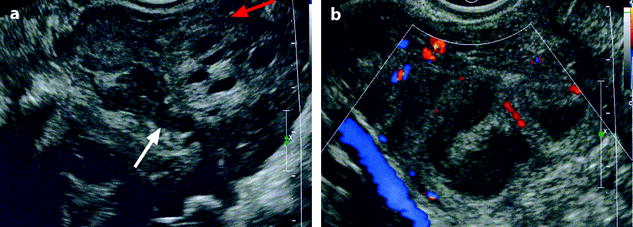
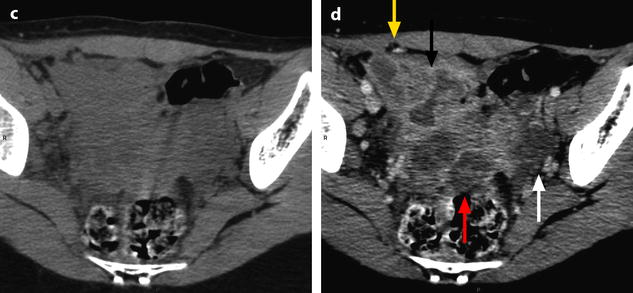
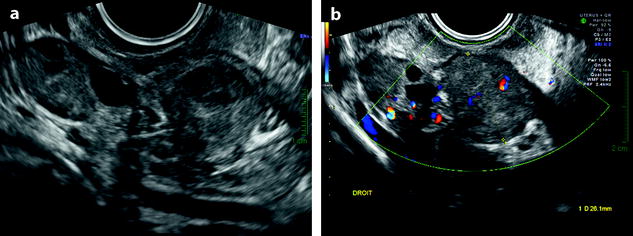
Fig. 16.1
Appendicular perforation complicated with localized peritonitis. EVS (a) and color Doppler (b) display a normal right ovary and medially a localized peritonitis
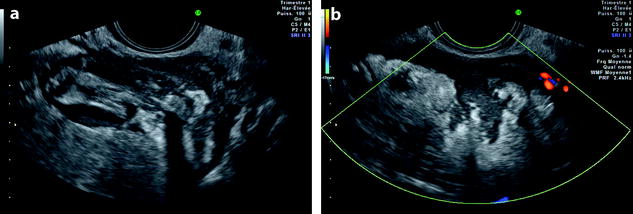
Fig. 16.2
Perforation of a sigmoid diverticulum complicated with sigmoiditis. (a) Sigmoid diverticulum. (b) Thickening of the mesosigmoid associated with echogenic peritoneal fluid, related to a localized peritonitis
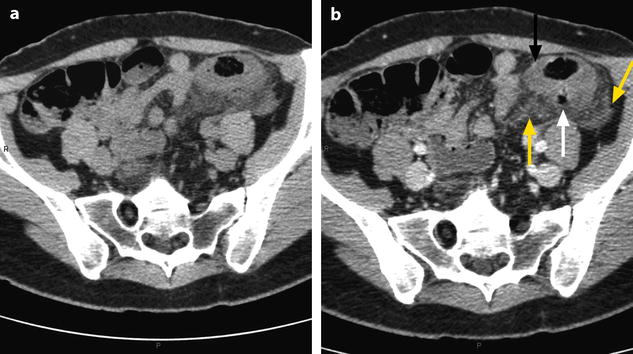
Fig. 16.3
Sigmoid diverticulum perforation complicated with sigmoiditis and peritoneal inflammatory reaction. Forty-three-year-old woman. Acute left pelvic pain. Increased white cell count 12,000/ml, CRP 113. CT without (a) and with IV contrast (b) displays (1) a thickening of the sigmoid wall (black arrow), (2) a perforated diverticulum (white arrow), and (3) an inflammatory reaction of the mesosigmoid (yellow arrows)
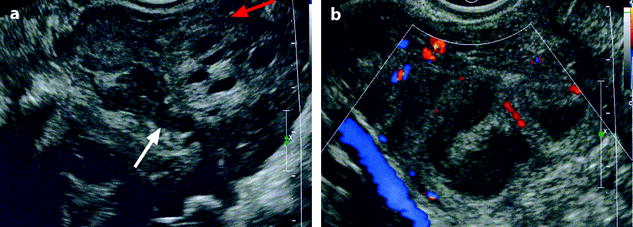
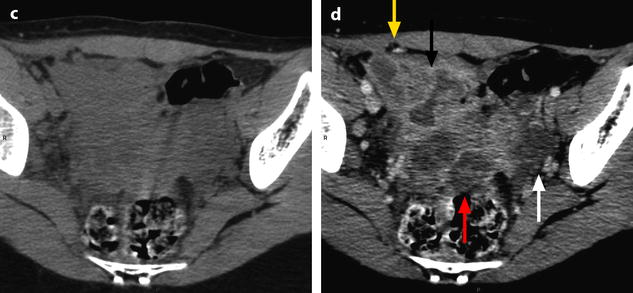
Fig. 16.4
Peritonitis complicated with left pyosalpinx following an appendicitis with peritonitis operated 10 days before (with right salpingectomy). Recurrence of fever, right pelvic pain, white cell count 19,000/ml CRP 48. EVS (a) depicts an inflammatory involvement of the right iliac fossa around the lateral face of the right ovary (red arrow) with peritoneal fluid related to a recurrence of peritonitis (white arrow). Transverse view of the left iliac fossa (b) displays a left pyosalpinx. Fig. 16.4 (continued) CT without (c) and with injection (d) depicts a huge abscess of the right iliac fossa (black arrow), extending to the anterior abdominal wall (yellow arrow), encasing small bowel loops, a left pyosalpinx (white arrow), an abscess in the Douglas (red arrow) with pelvic peritonitis
16.1.2 Granulomatous Peritonitis
16.1.2.1 Tuberculous Peritonitis
Tuberculous peritonitis, which is increasing in incidence, particularly among immunosuppressed patients, may be secondary to spread from a focus within the abdominopelvic cavity or be a manifestation of miliary spread.
The granulomas are characterized by caseous necrosis and Langhans giant cells; mycobacteria may be demonstrated by acid-fast stains or immunofluorescence methods.
There are several reports that point out to uncertainty in the preoperative diagnosis of peritoneal tuberculosis and advanced ovarian cancer [1–6]:
(a)
Clinical findings: PT presents with nonspecific findings and symptoms such as ascites and pelvic and abdominal pain and mass, and hence mimic ovarian cancer. Progression of PT often takes months or even years.
(c)
US of PT with female genital tract tuberculosis: adnexal masses, adhesions, and septate or particulate ascites. Omental and peritoneal thickening can also be seen.
(d)
CT (Figs. 16.5 and 16.6): smooth peritoneum with minimal thickening and pronounced enhancement suggests peritoneal tuberculosis, whereas nodular implants and irregular thickening suggest peritoneal carcinomatosis; however, peritoneal implants have also been observed in tuberculosis [1]. Omental and mesenteric thickening were demonstrated in all patients in BILGIN’s series [1]. Extensive adhesions can cause bowel obstruction. Para-aortic lymph nodes can be present.
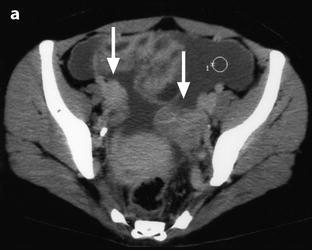
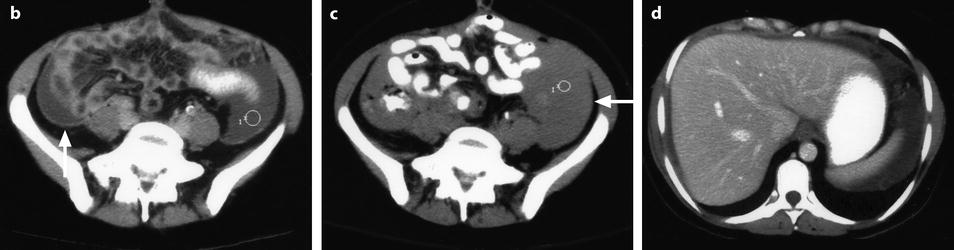

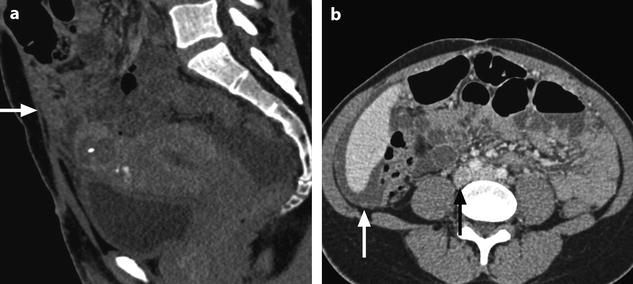
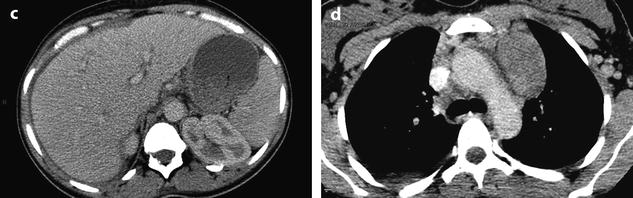
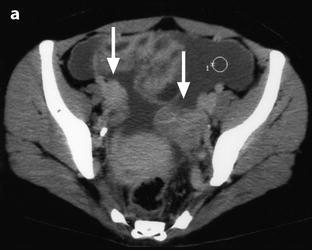
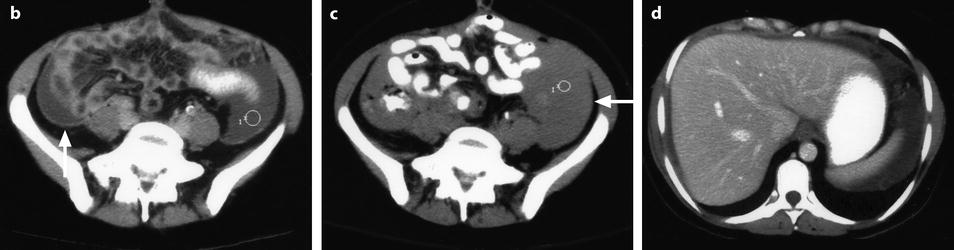

Fig. 16.5
Peritoneal tuberculosis with bilateral adnexal tuberculosis CT scan performed 60s after contrast (a), 4 min after (b, c, d), and half an hour after (e) demonstrates. (1) Bilateral slightly enlarged ovaries which look on the left multicystic (a) (arrows). (2) Pelvic ascites with thin and regular thickening of the peritoneum (b) (arrow). Diffuse contrast enhancement in the ascitic fluid after the delayed sequence is remarkable (c) (arrow). Abdominal ascites in both subphrenic spaces (d). (3) On (e), slightly enlarged lomboaortic (black arrow) and mesenteric lymph nodes (white arrows). Prospective diagnosis: Association of these different findings raised preoperatively the diagnosis of bilateral ovarian tumors with peritoneal metastases. Definite diagnosis: bilateral TB of the adnexae with peritonitis. The smooth pattern of the peritoneum without any focus or nodule or plaque and the pattern of the ovaries should have suggested the possibility of peritoneal tuberculosis
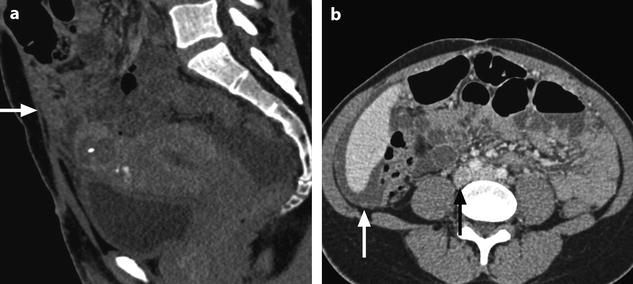
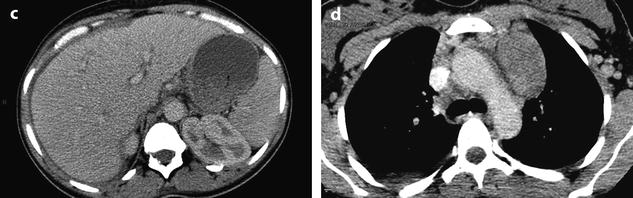
Fig. 16.6
Peritoneal tuberculosis. Thirty-year-old woman VIH+. CT after injection displays: (a) ascites in the Douglas and thickening of the greater omentum (arrow); (b) ascites of the subhepatic space, with thickening of the peritoneum (white arrow), lomboaortic lymph nodes, one of these with a necrotic center (black arrow); (c) ascites in the right subphrenic space; (d) the mediastinum: huge adenopathies. Prospective diagnosis: Association of the peritoneal lesions with the necrotic lomboaortic mediastinal lymph node suggested the diagnosis of TB. Fine-needle aspiration of the ascetic fluid confirmed the diagnosis of tuberculosis
(e)
MR: usually, the peritoneum is regular and thin, with a miliary diffusion.
(f)
Laparotomy is usually performed in the preoperative presumptive diagnosis of adnexal ovarian cancer. A rather pathognomonic picture of miliary tuberculosis with peritoneal thickening, omental cake formation, and adhesions are discovered throughout the peritoneal cavity.
16.1.2.2 Noninfectious
Foreign material (Fig. 16.7), sebaceous material, and keratin from ruptured dermoid cyst, spillage of amniotic fluid at caesarean section can produce a granulomatous peritonitis.
Fig. 16.7
Retained surgical sponge with abscess. Fifty-two-year-old woman, operated from perforation of the splenic flexure during colonoscopy a year before. Pelvic pain and dysuria. US without (a) and with color Doppler (b) depicts in the vesicouterine pouch a 6-cm round cystic mass with adhesion to the sigmoid containing an echogenic structure suggesting a retained sponge. Around the mass, thickening of the peritoneum suggests an abscess. Surgery confirms the diagnosis of abscess around the sponge, associated with adhesion to small bowel loops and localized inflammation of the peritoneum
16.2 Tumor-Like Lesions
16.2.1 Peritoneal Inclusion Cysts
Peritoneal pseudocyst occurs in different circumstances, all of them related to peritoneal adhesions: (1) after pelvic surgery, (2) after PID, and (3) after endometriosis.
Definition [7].
It is defined histologically by an inner sheet of peritoneal flat cells of mesothelial type.
These cells usually secrete clear fluid responsible for the development of the cyst. But in some circumstances, different kinds of fluid may be encountered.
The surgical and radiologic findings are reported in Table 16.1.
Table 16.1
Surgical and radiologic findings of peritoneal inclusion cysts
Common |
Size: usually between 4 and 10 cm |
Mainly or exclusively cystic |
Wall and septa thin and regular (loose fibrovascular connective tissue) |
Solid tissue can be present(related to inflammatory tissue) |
Usually not round, conforming to surrounding structures |
Lying against the peritoneum |
Most commonly multilocular, may be unilocular |
Adhesions to surrounding structures vey common(bladder, sigmoid) |
Uncommon |
May resemble simple free peritoneal fluid |
Small papillae present(exceptionally) |
16.2.1.1 US, CT, and MR Findings
1.
Unilocular cystic mass
The wall is thin and regular, without papillary projection. Its shape can be round or oval. Content of the cyst is usually clear fluid, anechoic, of a density close to 0 UH, with a signal close to urine on T1 and T2. Close relationship with the peritoneum can suggest the diagnosis.
However, differential diagnosis may include other differential diagnosis of unilocular cystic masses, particularly functional ovarian cyst, ovarian serous cystadenoma, paraovarian cyst, and hydrosalpinx.
2.
Multilocular pattern: the multilocular peritoneal inclusion cyst (MPICs) (Figs. 16.8 and 16.9).
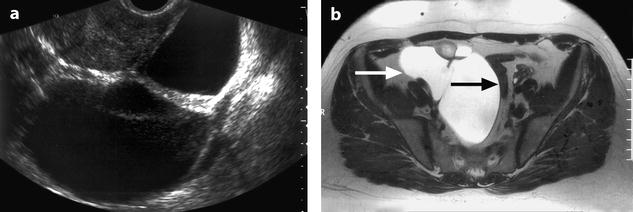
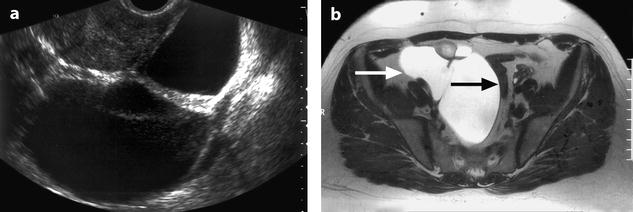
Fig. 16.8
Inclusion peritoneal cyst: multilocular form. Forty-year-old woman; right adnexectomy 3 years before. EVS (a) displays a multilocular collection, with a regular wall and septa. MR axial T2 (b) depicts and confirms the data concerning the shape and the structure of the collection and visualizes in its anterior part some tissue (which was inflammatory at pathology); MR precisely defined the topography of the mass, which follows the posterior, lateral (white arrow), anterior parietal peritoneum, and medially the sigmoid (black arrow). These relationships with the peritoneum are characteristic for inclusion peritoneal cyst
(a)
The characteristic overall shape of the mass is not round, conforming to the surrounding structures, encasing the ovary (which either looks normal or may contain large follicles related to some degree of ovaritis), and in direct relationship with the parietal and visceral.
(b)
The different loculi can be of the same or of different natures, separated by thin and regular septae. Regular vessels in the wall and in the septa can be displayed.
When a tissular portion is present, it looks regular with absence of tumoral vessel.
(c)
Although definite diagnosis of adhesions is difficult to assess, asymmetrical deformation of a full bladder and a close and identical relationship to contiguous organs according to different positions of the patient are very suggestive.
(d)
The pelvic ureter may be surrounded by fibrosis, resulting in a partial obstruction.
3.

Collection resembling simple free peritoneal fluid (Fig. 16.10).
Fig. 16.10
Peritoneal inclusion cyst: interest of the prone position. Forty-year-old woman operated from appendicular peritonitis 4 years ago. Two months ago, an abscess in contact to the anterior border of the right ovary was drained, but a posterior collection was left. MR with sagittal T2 (a) and Axial T2 in supine position (b) posterior peritoneal collection between the rectum and the posterior part of the uterus and the broad ligaments (arrows), which resembles free peritoneal fluid. Because of the previous clinical history, a prone position is performed. Axial T2 in prone position (c) The relationships of the peritoneal effusion with the pelvic structures do not change (arrows), allowing to make the diagnosis of a peritoneal inclusion cyst. Axial T1 (d) and fat suppression (e). Content of the collection is watery. After injection (f). This collection has a very thin wall with no contrast uptake
The only way to make the diagnosis is for the patient to change from position and to display exactly the same topography of the fluid in the peritoneal cavity (Fig. 16.11).
Get Clinical Tree app for offline access
Fig. 16.11
Peritoneal inclusion cyst secondary to PID. Thirty seven years old woman. Left pyosalpinx diagnosed at coeliscopy 4 years before. Infertility. EVS (a




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree