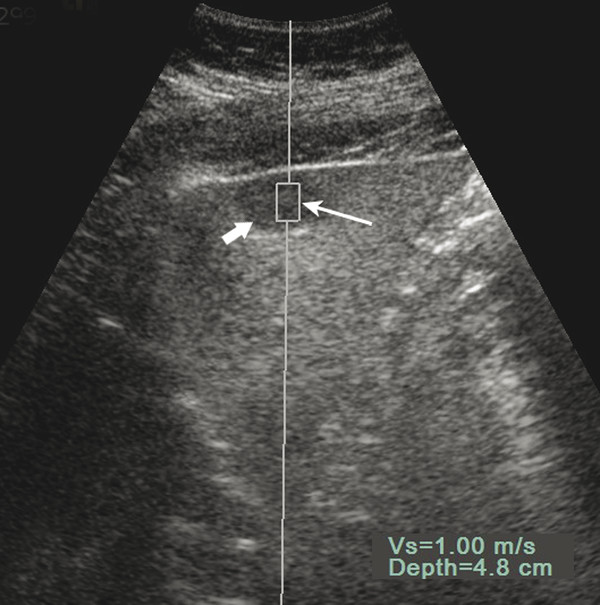
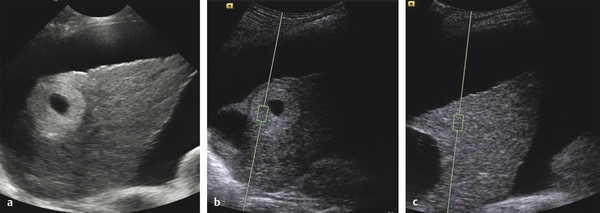
Elastography for Focal Liver Disease Characterizing focal liver masses comprises a significant component of health care costs with substantial impact on patient management both in health and disease. Metastatic liver cancers are the most frequently encountered malignant liver tumors, and patients with common primary cancers of the lung, breast, and colon are at such risk for development of these tumors that frequent surveillance of the liver is standard care in the period following detection and treatment of one of these primary lesions. Primary liver cancer is the fifth most common cancer in the world,1 and its detection and management place a large demand on imaging, as imaging surveillance of high-risk populations allows for improved detection of lesions while they are still at a small size and amenable to treatment. Added to this concern for the detection of possible malignant liver tumors, however, is the recognition that benign liver tumors and tumorlike liver conditions are also frequent. Although these benign lesions may have typical features on baseline ultrasound, their confident diagnosis is often required to ensure that they are not mistaken for a significant malignant lesion and also to be certain that a significant malignant lesion is not erroneously overlooked. Therefore, many masses incidentally detected on ultrasound are studied further with contrast-enhanced cross-sectional imaging, including magnetic resonance imaging, computed tomography, or ultrasound. Historically, liver masses were diagnosed by either their surgical excision or biopsy. In the last four decades, however, there has been a progressive trend away from such invasive procedures. We now live in an era of noninvasive liver mass diagnosis. This has been accomplished largely on the basis of information acquired with the use of contrast-agent imaging on computed tomography (CT), magnetic resonance imaging (MRI),2 and more recently ultrasound (US).3 This works exceedingly well and, today, only a minority of liver masses are subjected to biopsy to establish their diagnosis. The noninvasive evaluation of liver masses is important, as benign and insignificant masses are frequently encountered. Hemangioma, the most common benign liver tumor, for example, is present in as many as 20% of patients on autopsy studies.4,5 They are frequently identified in this era of cross-sectional imaging, where they are often discovered as an incidental finding on CT, MRI, or US examinations performed for unrelated reasons. Noninvasive confirmation of their benign nature allows them to be removed from consideration for clinical management and avoids unnecessary painful biopsy and anxiety. Elastography, or elasticity imaging, is a newer noninvasive imaging technology that measures the natural tendency of tissue to resume its original size and shape after being subjected to a deforming force or stress.6,7 The provision of these stiffness measurements is established as a method of assessing diffuse liver disease, for the determination of the degree of fibrosis through its progression to cirrhosis. It is also established as a method for differentiating hard malignant breast tumors from those that are softer and more likely to be benign. It is known that tumors are generally many times stiffer than their surrounding tissue regardless of their organ of origin, making their response to deformation much different. Therefore, when a mechanical compression or vibration is applied, the tumor deforms less than the surrounding tissue. However, if one compares a cirrhotic liver, which is stiffer than a normal liver, with a tumor, the difference in the stiffness may vary. A tumor that might be hard relative to a normal liver may, in fact, be soft relative to a liver with cirrhosis. Here, we address the application of elastography to the diagnosis of focal liver masses in any liver and the differentiation of those that are malignant from those that are benign. Numerous approaches to elastography have been described in the literature but three in particular, point shear wave elastography (p-SWE), two-dimensional shear wave elastography (2D-SWE), and strain elastography (SE), are considered best for this application. These different types of elastography are applied differently and their tissue response varies although a similar scientific foundation is common to all. Transient elastography (TE), marketed as FibroScan (Echosens, Aix-en-Provence, France), is performed with an ultrasound transducer at the end of a vibrating piston, which produces a vibration of low amplitude and frequency. The transducer is placed blindly (as there is no visual confirmation of the location of the measurement) on the skin surface and the shear wave produced is transmitted through the skin and into the liver up to a depth of about 6 cm. The velocity of the returning pulse is proportional to the tissue stiffness with higher velocities suggestive of stiffer tissue. This blind propagation of a pulse is seemingly suitable for the evaluation of an entire large organ, such as the liver, and may also show stiffness measurements for palpable masses, such as those encountered in the breast. A liver mass, however, is generally not palpable as it is deep to the costal margin, making TE unacceptable for this application. Point shear wave elastography utilizes acoustic radiation force impulses (ARFI), a newer US elastography technique recently introduced within a conventional ultrasonsograhic device (Acuson S2000, Siemens Medical Solutions, Mountain View, CA) and more recently also on the Philips EPIQ (Philips, Bothel WA). It differs from TE, which applies a pressure manually to the surface of the organ to induce an elastic shear wave. In ARFI, an acoustic radiation pulse is generated in the area of interest by the probe during the real-time B-mode imaging. As with TE, higher shear wave speeds are representative of stiffer tissue. ARFI uses high-energy focused acoustic pulses of short duration (< 1 ms) to excite the tissue in the region of interest, and these pulses displace soft tissue between 1 and 20 µm. These displacements result in shear wave propagation away from the region of excitation, which travel perpendicular to the acoustic push pulse and are detected by using US tracking beams. The speed of the shear waves propagated are measured as a velocity, in meters per second, and the display shows the fixed region of interest and its placement within the tissue under study in grayscale (▶ Fig. 4.1). The measurements, in meters per second, are obtained by placing a region of interest (ROI) box of fixed size within the tissue under direct guidance (▶ Fig. 4.2). Fig. 4.1 Acoustic radiation force impulse (ARFI) technique for shear wave elastography (SWE). Measurement of velocity of shear wave within the ROI (long arrow) of a hypoechoic focal liver mass (short arrow) with underlying fatty liver of a 29-year-old woman. This mass is confirmed as a hemangioma on following contrast-enhanced ultrasound. Vs = velocity of shear wave. Depth indicates the distance from the skin to the center of the ROI. Fig. 4.2 Point shear wave elastography of the liver and a focal liver mass. The patient is a 41-year-old male with hepatitis B virus–related cirrhosis and a known renal cell carcinoma of the kidney. (a) Baseline ultrasound shows a cirrhotic liver and ascites. An unusual mass shows a highly echogenic rim and a necrotic or cystic center. (b) shows an ARFI measurement from the solid rim, Vs 1.09 m/s. (c)The measurement at a similar depth in the liver shows an abnormally high result, consistent with the known cirrhosis. The mass is softer than the cirrhotic liver. The mass is a biopsy proven hepatocellular carcinoma.
4.1 Introduction
4.2 Noninvasive Diagnosis of Focal Liver Masses
4.3 Elastography for Liver Mass Diagnosis
4.3.1 Shear Wave Elastography
Transient Elastography
Point Shear Wave Elastography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree