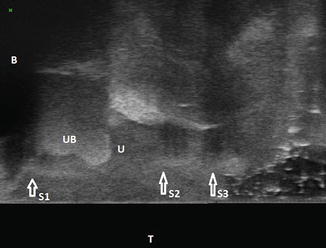
Fig. 7.1
180° scan of anterior compartment: midurethral retropubic sling seen as a hyperechogenic structure beneath midurethra. B bladder, U urethra, P pubic symphysis, UVJ urethrovesical junction, S midurethral retropubic sling
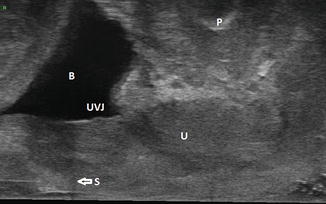
Fig. 7.2
180° scan of anterior compartment: retropubic sling seen proximal to the urethrovesical junction. B bladder, U urethra, P pubic symphysis, UVJ urethrovesical junction, S retropubic sling
7.2.2.2 360° Scan
Similarly, while scanning with the 2052 probe, it is important to ensure that the probe is inserted in the vagina in the neutral position and has been inserted cephalad enough to capture all important details. Though normally the cephalad extent of the 3D scan should begin just proximal to the urethrovesical junction so that in the sagittal cut of the data volume, a small portion of the bladder is seen narrowing into the urethrovesical junction, it must be kept in mind that in the case of slings that have not fixated suburethrally and hence are located proximally beneath the bladder, the 3D scan may need to begin even more cephalad. At the same time, it is necessary to ensure that the caudad extent of the 3D data volume is beyond the external urethral meatus so that the urethra is imaged along its entire length. Hence often it may be necessary to capture two 3D data volumes along the length of the urethra to ensure that all important structures are included. Increasing the depth may help to include the entire extent needed in a single data volume, but it must be remembered that increasing the depth reduces the resolution and decreases the image size.
7.2.3 Manipulation of the 3D Data Volume to Trace the Intrapelvic Course of Slings, Retropubic, and Transobturator
The 180° 3D data volume of the anterior pelvic compartment (probe 8848) can be manipulated in the sagittal, axial, or coronal planes. However to track the intrapelvic course of a sling, it is preferable to begin with manipulation in the sagittal plane. It is important to first orient to the egocentric coordinates, i.e., the relative directions of the data volume, or more simply put, it is important to first understand which sagittal surface of the data volume denotes the left of the patient and which surface, the right. Depending on how the 3D external mover moves the probe, the 3D scan may begin on the left or right of the patient. If the 3D external mover is programmed to begin the scan on the left of the patient, then the data volume is constructed progressively in real time during scanning from the left to the right.
As one begins manipulating the 3D data volume in the sagittal plane, the arm of the sling on that side progressively comes into vision. The arm of the sling, in case of retropubic slings, can be seen, exhibiting a mesh-like weave, extending until the pubic symphysis. In the case of transobturator sling, the arm can be seen extending at a more obtuse angle beyond the pubic symphysis. The sling can be tracked behind the urethra in the midsagittal plane and then can be seen extending on the other side to the pubic symphysis in case of retropubic slings or beyond the pubic symphysis at a more obtuse angle in case of transobturator slings.
The location of the sling behind the urethra in the midsagittal plane will vary depending on the type of sling. In case of TVT slings (Fig. 7.1) and transobturator slings (Fig. 7.3), the sling will be seen as a hyperechogenic horizontal structure beneath the midurethra, and in the case of a bladder neck sling, it can be seen beneath the proximal urethra with its proximal end at the urethrovesical junction (Fig. 7.4).

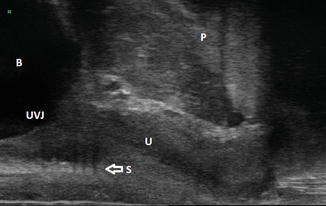

Fig. 7.3
180° scan of anterior compartment: transobturator sling seen as a hyperechogenic structure beneath midurethra. B bladder, U urethra, P pubic symphysis, UVJ urethrovesical junction, S transobturator sling
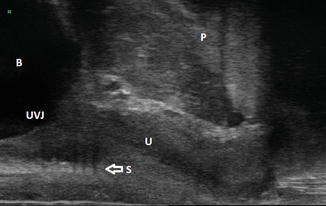
Fig. 7.4
180° scan of anterior compartment: pubovaginal sling seen at bladder neck. B bladder, U urethra, P pubic symphysis, UVJ urethrovesical junction, S pubovaginal sling
The intrapelvic course of the slings can be tracked more easily when the rendered volume of the data volume is manipulated (Fig. 7.5). Often one may need to manipulate the data volume in oblique parasagittal planes to be able to track the sling course better.
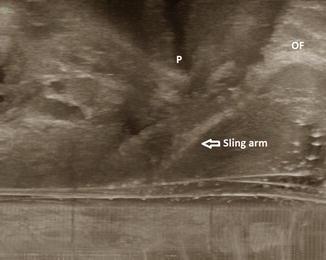
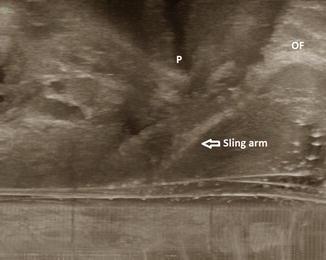
Fig. 7.5
180° scan of anterior compartment: rendered volume, single incision sling arm seen on the right of the patient extending beyond the pubic symphysis until the obturator foramen. P pubic symphysis, OF obturator foramen
Manipulation of the 3D data volume obtained with the 2052 probe can also be done in the axial, sagittal, and coronal planes. However, transobturator and retropubic slings can be more easily differentiated in the axial plane. Manipulation in the axial plane adds to the information obtained from sagittal manipulation of the data volume obtained via the 8848 probe as we are able to look at the sling from a different angle. The retropubic sling can be seen in the axial plane in a u-shaped curve hugging the urethra (Fig. 7.6), while the transobturator sling can be seen extending hammock-like to the obturator foramina bilaterally (Fig. 7.7). The slings can be seen better when the rendered volume of the data volume is manipulated. We may also need to manipulate the data volume in oblique planes to follow the course of the sling until its insertion points bilaterally.
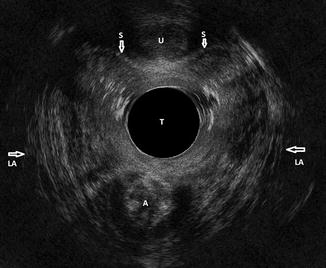
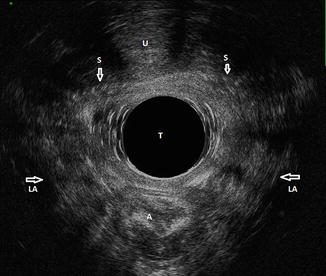
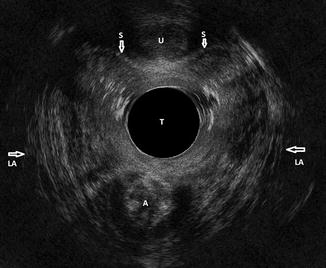
Fig. 7.6
360° scan: retropubic sling seen hugging the urethra in a u-shape. U urethra, A anal canal, LA levator ani muscles, T probe, S midurethral retropubic sling
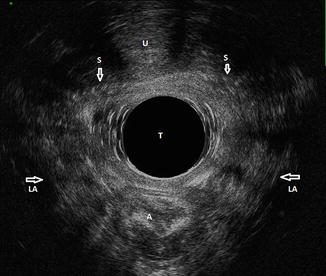
Fig. 7.7
360° scan: transobturator sling seen extending hammock-like to the obturator foramina bilaterally. U urethra, A anal canal, LA levator ani muscles, T probe, S transobturator sling
7.2.4 2D Dynamic Functional Assessment of the Slings and Its Correlation with Outcome
The in vivo behavior of the sling during periods of stress, namely, cough, Valsalva, and squeeze maneuvers, can be assessed by recording 20 s 2D cineloops in the midsagittal plane or the axial plane using the 8848 probe (endovaginal ultrasound of the anterior compartment) or the 8802 probe (transperineal ultrasound). These cineloops can also be stored for offline analysis and are available as a permanent record of in vivo sling behavior.
Dynamic assessment of the sling in the mid-sagittal plane helps to understand whether the urethra moves in a concordant manner with the sling during cough and Valsalva maneuvers. We are currently conducting a study in which we are comparing results of dynamic assessment of the sling performed with the transperineal 8802 probe and endovaginal 8848 probe with continence outcomes in the case of Monarc (American Medical Systems, Minnetonka, MN), TVT (Ethicon, Bridgewater, New Jersey), and I-STOP pubovaginal sling (CL Medical, Lyon, France) 1 year after surgery. Our experience has helped us understand that when the urethra and the sling don’t move in a concordant fashion, i.e., the urethra moves independent of the sling, the outcome is poor. It may be that the sling has not fixated itself well to the suburethral connective tissue or that the sling has been inserted too loosely and therefore, even though the sling has scarred in following surgery, the urethra and surrounding tissue move independent of it. Therefore even if the midurethral or bladder neck sling is confirmed on static 2D and 3D ultrasound to be placed in the correct location, dynamic assessment may show that the urethra moves independent of it on dynamic assessment. In some patients with failed slings, the urethrovesical junction is sometimes even seen to move distal to the sling on dynamic assessment. Therefore the sling does not have the desired functional effect and may fail.
Kociszewski et al. correlated the dynamic changes in TVT sling shape seen on transperineal ultrasound with outcomes following TVT sling surgery in 72 women [10]. They found that 98 % of patients, in whom the tape was flat at rest along its width in the midsagittal plane and curved into a c-shape during straining, were continent after surgery. There was improvement in one case (2 %) and none of these patients was classified as failure. However, in 39 % of the patients, no change was visible in the sling shape along its width on straining in the midsagittal plane. In the 11 % of patients in whom the tape position was flat along its width at rest and during straining (i.e., too far away from the urethra), the failure rate was highest at 25 %. In the 28 % of patients in whom the sling was c-shaped along its width at rest and on straining, the failure rate was 10 %.
In our experience, the deformability of the sling on Valsalva (flat at rest along its width and deformed to a c-shape on Valsalva), the concordance of urethral movement with the sling and the location of the sling are all correlated with outcomes following sling surgery. Our data (unpublished) suggests that the best outcomes following transobturator sling surgery are found to be associated with concordance of urethral movement with the sling, followed by midurethral location of the sling and deformability of the sling on dynamic assessment in that order. A patient in whom the sling does not deform on Valsalva (i.e., does not curve into a c-shape from flat at rest along its width) may still have a successful outcome if the sling is located in the correct location (midurethral) at rest and the urethra moves in a concordant manner with the sling. Conversely, a patient, in whom the sling deforms on Valsalva, may still have a poor outcome if the urethra moves in a discordant manner with the sling and/or the sling is not located beneath midurethra.
7.2.5 Diagnosis and Planning of Future Treatment in the Case of Failed Sling Surgery
In patients who have poor outcomes following sling surgery, multicompartment 3D imaging can often be invaluable in delineating the cause for failure and also plan future treatment. There are various scenarios we encounter in such patients at our center which we shall discuss in this section.
7.2.5.1 Unknown Sling Type
Often the patient is unaware of the exact nature of the previous sling surgery. 2D imaging cannot delineate the type of sling on either transperineal ultrasound or endovaginal ultrasound. A midurethral sling, whether retropubic or transobturator, will appear as a hyperechogenic horizontal structure behind the midurethra (Figs. 7.1 and 7.3). A bladder neck sling, which is located correctly at the urethrovesical junction, should ideally be easy to distinguish from a midurethral sling based on location. But in patients with poor outcome following surgery, a midurethral sling is often found to be located too proximally. Therefore a sling that is found to be located under proximal urethra may not necessarily be a bladder neck sling, but could be a midurethral sling.
Multicompartment 3D imaging including dynamic functional assessment is very useful in determining the type of sling that was inserted in such patients. As described above, the intrapelvic course of the sling can be tracked by manipulating the 3D data volume. The sling can be examined in the three different data volumes obtained with transperineal ultrasound, 180° endovaginal scan with the 8848 and/or 360° scan, and hence the diagnosis obtained through one probe can be confirmed through the other. Rendered volumes can be used to track the sling better.
Dynamic functional assessment also helps to distinguish slings based on elasticity and deformability. At our center, we use an inelastic retropubic sling (I-STOP, CL Medical, Lyon, France) placed at the bladder neck in patients with intrinsic sphincter deficiency. The I-STOP sling has lower elasticity and lower deformability as compared to other slings [11]. We find that an I-STOP sling lies flat at rest (Fig. 7.4) against the urethra and, on dynamic assessment, it moves with the urethra and constricts the bladder neck without deforming or bending into a c-shape along its width. This is concordant with its mechanism of action, which is by increasing resistance at the bladder neck during periods of stress as opposed to that of elastic midurethral slings, which act by causing dynamic compression. Thus it is easy to distinguish the I-STOP sling from other slings that have higher elasticity and greater deformability (TVT (Ethicon, Bridgewater NJ), Monarc (American Medical Systems, Minnetonka, MN), SPARC (American Medical Systems, Minnetonka, MN), etc.).
It is also possible to distinguish different types of materials, with the previous generation IVS being much less echogenic than the TVT [6]. Because the I-STOP sling is less deformable, it appears fatter and wider than TVT or Monarc slings. Also since the SPARC sling carries a central suture that prevents pretensioning [12], it generally seems flatter and wider than TVT sling [6].
7.2.5.2 Determining the Location of a Failed Sling
Confirming the location of the sling may be useful preoperatively if sling takedown surgery is planned. Determining the location of the failed sling may help to elucidate the reasons for failure of the surgery. There is controversy whether location of the sling is important to ensure continence. Several authors contend that location of the midurethral sling does not have any impact on the outcome following surgery [4, 13, 14]. From a theoretical point of view, Dietz et al. contend that since midurethral slings work by “dynamic compression,” i.e., kinking or compression of the urethra against the posteroinferior contour of the pubic symphysis whenever intraabdominal pressure is raised, it should not matter much for success as to whether the obstruction affects proximal or distal urethra [6].
However, urethral pressure profile measurements and lateral urethrocystography have confirmed that the urethral zone between the point of maximal urethral closure pressure and the urethral knee is crucial for continence mechanism. This zone, termed as the high-pressure zone of the urethra, has been calculated to lie between 53 and 72 % of the functional urethral length, where pubourethral ligaments attach [1]. We conducted an unmatched case-control study of 100 patients who underwent transobturator sling surgery (Monarc, American Medical Systems, Minnetonka, MN) at our center to determine the association of static and dynamic location of transobturator slings with outcomes 1–2 years following surgery [15]. These 100 patients constituted two groups: group A (n = 50) who had successful outcomes and group B (n = 50) who had poor outcomes 1–2 years following surgery. Treatment outcome was determined based on a composite measure of “failure”: presence of urine leakage on a standardized cough stress test (CST) at 250 mL and a “yes” answer to question 3 of the UDI-6 validated questionnaire. All the enrolled patients underwent 3D EVUS of the anterior pelvic compartment by a fellow who was blinded to the treatment outcomes. The sling location was significantly more proximal in group B as compared to group A (p < 0.001). In group A, while only 50 % of the slings were located beneath the “high-pressure zone,” 20 % were located at the junction of proximal and midurethra. On dynamic assessment during cough and Valsalva, the urethra moved concordant with the sling in 44 (88 %) patients in group A and only in 21 (42 %) of patients in group B (p < 0.001). The urethrovesical junction moved distal to the sling on dynamic assessment in nine (18 %) patients in group B and none of the patients in group A (p < 0.001). Thus in our study, transobturator slings were found to be located more proximally on 3D EVUS in patients with sling surgery when compared with patients with successful outcomes. Also dynamic functional assessment of the sling helped understand in vivo sling behavior in patients with poor outcome following surgery.
Kociszewski et al. [10] found using transperineal ultrasound in 72 women, that a TVT tape located between 50 and 80 % of the urethral length was associated with a success rate of 91 %, whereas the other tape positions failed in 36 % of the patients (p = 0.0085). In another study of 61 patients who had poor outcome following sling surgery (49 patients had undergone transobturator sling surgery and the remaining, a retropubic procedure), 3D EVUS was performed with the 8848 probe [16]. Only 21.3 % of the patients had the tape positioned between 50 and 75 % of the urethral length. The tape was found below 50 % of the functional urethral length in 73.8 % of the patients examined and above 75 % of functional urethral length in 4.9 % of the patients [16].
Is this change in position observed a natural progression or iatrogenic? The position of TVT sling has not been observed to change much over time [17, 18]. A gradual caudal displacement of the TVT has been described, but it is concordant with the distal movement of the surrounding tissues, particularly in women who have undergone concomitant anterior repair. It therefore may reflect recurrence or progression of prolapse rather than natural tape movement [6]. One possible explanation is that the sling was inserted proximally rather than in the midurethral location at the time of surgery. In a study of 102 women who underwent TVT sling surgery, urethral length was measured by preoperative introital ultrasonography, and suburethral incision was initiated at one-third of the sonographically measured urethral length [19]. Six months following surgery, the TVT sling was found in the target range of 50–70 % of the urethral length in 88.2 % of patients. 91.1 % of the patients were cured and 6.9 % of the patients showed improved continence symptoms.
If location of the sling is important, does stitching the sling in place after insertion help? Rechberger et. al. randomly allocated 463 patients with SUI to treatment with a standard transobturator sling procedure (232 patients) or to a transobturator sling procedure with additional 2-point tape fixation with absorbable sutures (231 patients). Both the subjective cure rate (85.15 % vs. 75.77 %) and the objective cure rate (85.37 % vs. 75.59 %) were significantly more in the tape-fixation group [20]. Among patients with intrinsic sphincter deficiency, the outcomes were significantly better in the tape-fixation group when compared with the control group (95.1 % vs. 73.8 % cured or improved; p = 0.0011).
However, does suture-fixating the sling at the time of implantation ensure that the sling will remain in the desired location a year after surgery? We conducted an unmatched case-control study of 80 patients returning to our center for the 1-year follow-up visit following sling surgery for SUI [21]. The study group A consisted of 40 patients who had undergone transobturator sling surgery (Monarc, American Medical Systems, Minnetonka MN) in which the sling was not suture-secured to the midurethra. Forty patients had undergone a suburethral pubovaginal sling procedure during which the tape was suture-fixated to the proximal urethra (I-STOP, CL Medical, Lyon, France) and constituted the control group B. All the enrolled patients underwent 3-dimensional endovaginal ultrasound of the anterior pelvic compartment at the 1-year follow-up visit by a fellow who was blinded to the type of sling surgery performed. Only 14 (35 %) patients had the sling in the desired location in group A as compared to 31 (77.5 %) patients in group B (p < 0.001). The odds of the sling being located at the desired position was significantly more in group B when compared with group A (OR, 2.21; 95 % CI, 1.027–4.77, p = 0.04). Thus, we found that suture-fixating the sling tape in place during implantation may ensure that the sling is in the desired location 1 year following sling surgery. In order to understand whether the transobturator route of the surgery was a potential confounder to the study results, we expanded the study to include 40 patients who had undergone TVT (Ethicon, Bridgewater, NJ) sling surgery in a third group (unpublished data). In the TVT group also, only 14 (35 %) patients had the sling in the desired midurethral location when compared to 31 (77.5 %) in the I-STOP group. Based on tape percentile (the distance of the midpoint of the sling from the urethrovesical junction divided by the urethral length), the tape location in the patients who had undergone transobturator sling surgery was more proximal than that in patients who had undergone TVT sling surgery; however, it was not statistically significant (p = 0.254). There may be other confounders that we have not accounted for, including the difference in elasticity and flexibility of the slings; however, the study results do suggest that suture-fixating the tape in place during implantation may help to ensure desired sling location a year following surgery. We are now conducting a pilot study where we are stitching Monarc slings in place after insertion, and we will compare location of the slings in these patients with those in whom the sling has not been stitched in place.
7.2.5.3 Planning of Treatment in Patients with Complicated Treatment History
Many patients who are referred to a center with incontinence have a complicated treatment history. Many have history of multiple sling surgeries (Fig. 7.8) or multiple previous sling surgeries followed by multiple bulking agent injections (Fig. 7.9).
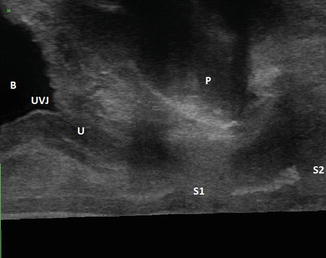
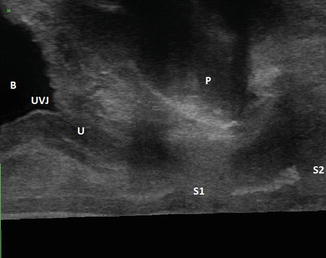
Fig. 7.8
180° scan of anterior compartment: multiple previous sling surgeries. B bladder, U urethra, P pubic symphysis, UVJ urethrovesical junction, S1 midurethral retropubic sling, S2 transobturator sling displaced distally