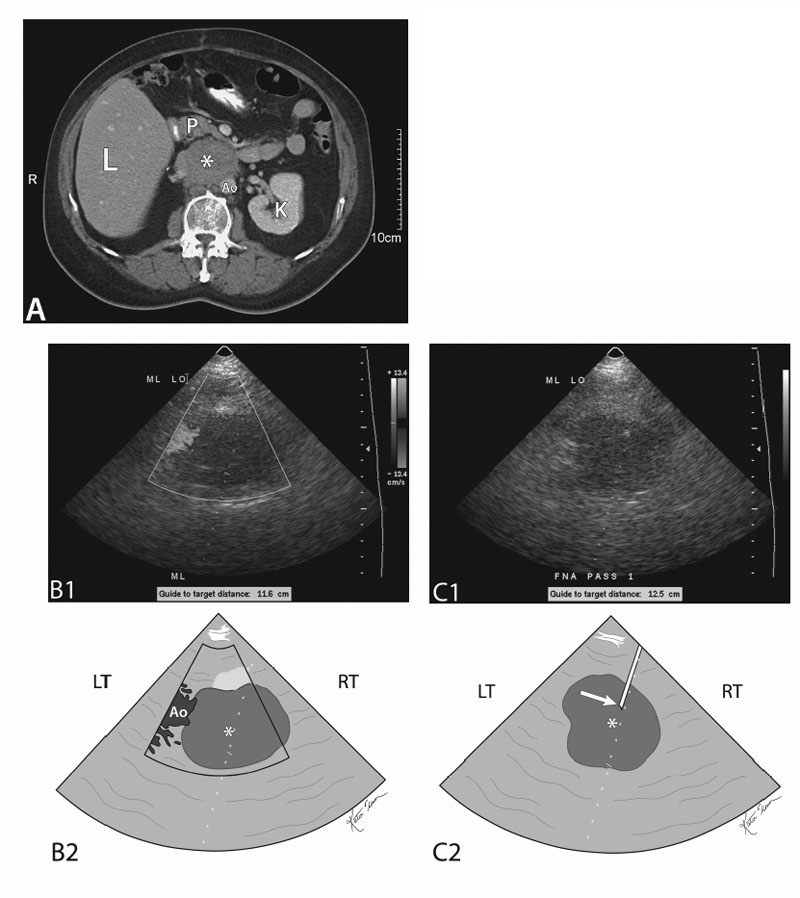
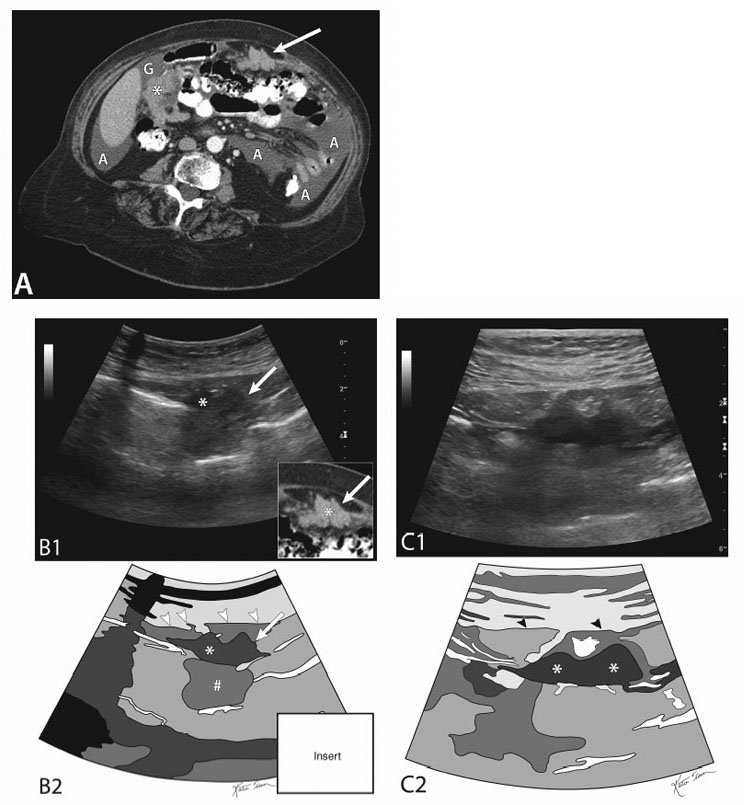
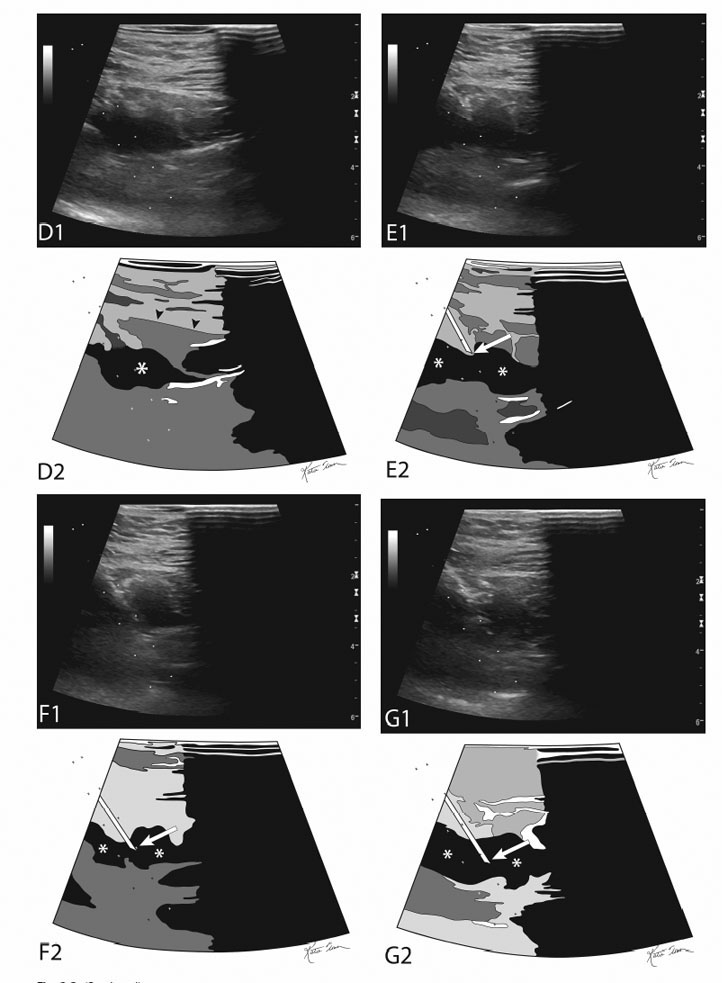
3 Extravisceral Abdominal Mass Biopsy Extravisceral abdominal masses can be classified into extravisceral retroperitoneal masses and extravisceral intraperitoneal masses. Fig. 3.1 Retroperitoneal mass biopsy (fine-needle aspirate [FNA]). (A) Contrast-enhanced axial computed tomography (CT) image of the abdomen. The image demonstrates a large retroperitoneal mass (asterisk) most likely the result of amalgamated paraaortic retroperitoneal lymph nodes. (B) Doppler ultrasound image of the retroperitoneal mass seen in Fig. 3.1A (top) and sketch of same (bottom). The retroperitoneal mass is again seen (asterisk at epicenter). It is avascular and the aorta is seen to its left. The needle trajectory guide (dotted line) is seen going through the mass. (C) Ultrasound image of the retroperitoneal mass (asterisk in center of mass) seen in Figs. 3.1A and 3.1B (top) and sketch of same (bottom). A 19-gauge coaxial needle has been passed into the mass (arrow at coaxial needle tip). The operator now is ready to pass the 22-gauge FNA needle sequentially. (K, left kidney; L, liver; Ao, aorta; P, pancreas; LT, left; RT, right) Fig. 3.2 Omental mass biopsy. (A) Contrast-enhanced axial computed tomography (CT) image of the abdomen. The image demonstrates peritoneal fluid (A, ascites) and omental masses (asterisk and arrow). Peritoneal fluid is also seen at the gallbladder fundus (G). The omental mass deep to the gallbladder (asterisk) is difficult to access. The operator decided to biopsy the more superficial left-sided mass (arrow), which is more accessible. Hypothetically, if the right-sided omental mass was the only mass (no left-sided mass), a transhepatic approach utilizing a coaxial needle would be reasonable to entertain. Strictly speaking, when trying to determine the diagnosis (which is most likely malignant in this setting) from the least risky to the more risky, the following (in order) should be performed: (1) Cytology evaluation of ascetic fluid aspirate; (2) direct percutaneous left-sided-mass aspiration/biopsy, and (3) transhepatic fine-needle aspiration of the right-sided mass. (B) Ultrasound image of the left-sided mass seen in Fig. 3.2A (top) and sketch of same (bottom). An insert is placed in the bottom left-hand corner, which is a cropped CT image from Fig. 3.2A. Again seen is the mesenteric mass (arrow), which has a superficial “double-humped” component (asterisk) and a deeper component (#) which is relatively more echogenic than the more superficial double-humped component. The arrowheads point to the sonographic plain of the deep fascia. (C) Ultrasound image utilizing a linear transducer of the same mass seen in Figs. 3.2A and 3.2B(top) and sketch of same (bottom). The more superficial double-humped component (asterisks) is more closely seen. The arrowheads point to the sonographic plain of the deep fascia. (D) Ultrasound image utilizing a linear transducer of the same mass (top) and sketch of same (bottom). The operator has switched on the needle trajectory guide (sites: diverging dotted lines), which traject through the more superficial double-humped component (asterisk). The arrowheads point to the sonographic plain of the deep fascia. (E) Ultrasound image utilizing a linear transducer of the same mass (top) and sketch of same (bottom). The operator has passed an 18-gauge Trucut biopsy needle, which is indenting the tissue plain superficial to the mass (asterisks). (F) Ultrasound image utilizing a linear transducer of the same mass (top) and sketch of same (bottom). The operator has “fired” or deployed the 18-gauge Trucut biopsy needle (arrow), which has penetrated the mass (asterisks). (G) Ultrasound image utilizing a linear transducer of the same mass (top) and sketch of same (bottom). The operator has made a second 18-gauge Trucut biopsy needle (arrow) pass, which has again penetrated the mass (asterisks). Extravisceral abdominal lesions/masses biopsies can be sampled utilizing ultrasound or computed tomography (CT) guidance. The choice of CT versus ultrasound guidance depends on operator preference, experience, and the availability of adequate ultrasound and/or CT imaging. The size of the target lesion/mass, its location, and its proximity to important organs and/or structures, as well as the proximity of structures and/or viscera in the needle path all contribute to the choice of imaging modality. Certainly, ultrasound guidance can be used for large lesions; however, small lesions/masses adjacent to important abdominal structures usually require CT guidance for precision biopsy. Generally, at my institution the majority of retroperitoneal masses are biopsied utilizing CT guidance. Intraperitoneal masses are biopsied by either ultrasound guidance (superficial lesions with a wide window for the needle trajectory) or by CT (deeper lesions with a narrow window of needle trajectory).
Classification
Retroperitoneal Extravisceral Masses
Intraabdominal Extravisceral Masses
Indications
Contraindications
Absolute Contraindications
Relative Contraindications
Preprocedural Evaluation
Evaluate Prior Cross-sectional Imaging
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree