(1)
Department of Medical Imaging, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan
(2)
Department of Medical Imaging and Radiological Sciences, Institute of Radiological Research Chang Gung University, Taoyuan, Taiwan
10.1 Uterine Prolapse
Case 1
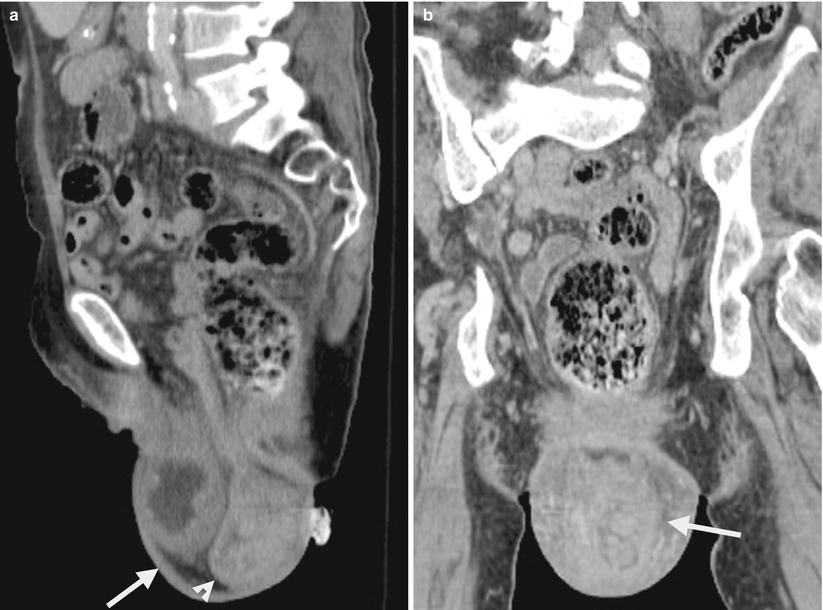
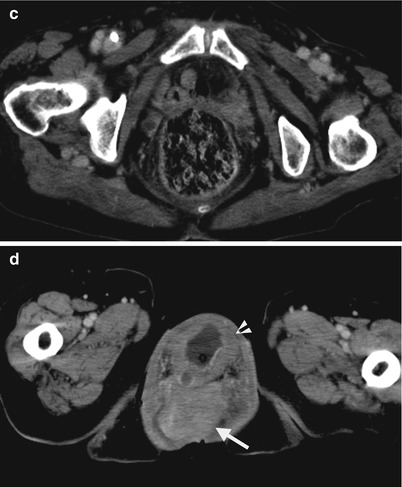
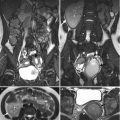
Fig. 10.1
Computed tomography (CT) shows imaging findings of uterine prolapse in a 75-year-old female. Figure 10.1a, sagittal enhanced CT shows a protruding sac (arrow) from the pelvic cavity to the perineum due to underlying severe pelvic floor laxity. There is prolapsed uterus (arrowhead) at the posterior part of the sac. Cystocele is present anterior to the prolapsed uterus. Figure 10.1b, coronal enhanced CT shows the uterus (arrow) prolapsed into the perineal sac simulating male scrotal sac appearance. Figure 10.1c, axial enhanced CT at the symphysis pubis level shows absence of the uterus and urinary bladder at the lower pelvic cavity. Instead, only small bowel loops and the rectum are visualized. Figure 10.1d, axial enhanced CT at the perineal sac level shows a prolapsed uterus (arrow) posterior to the cystocele (arrowhead) in the perineal sac.
Key Diagnostic Features
Uterine prolapse occurs due to pelvic floor laxity which is most commonly seen in multiparous women of old age. Concurrent uterine prolapse and cystocele are common by their similar underlying etiology. On images, uterine prolapse is diagnosed by identifying a prolapsed uterus into the perineal area rather than the normal uterine fossa location.
10.2 Uterine Myomas
Case 2
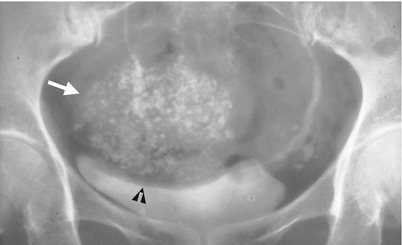
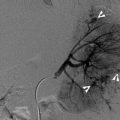
Fig. 10.2
Excretory urography (EU) shows imaging findings of a calcified uterine myoma. Figure 10.2, magnification view of the pelvic cavity shows a calcified mass (arrow) with indentation effect on the urinary bladder dome, consistent with a uterine myoma.
Case 3

Fig. 10.3
Computed tomography (CT) shows imaging features of a uterine myoma of subserosal location. Figure 10.3a, unenhanced axial CT image shows enlarged uterus size (arrow). Figure 10.3b, enhanced axial CT image shows a large uterine myoma (arrow) of predominant homogeneous enhancement but less than that of normal myometrium. The presence of this uterine myoma accounts for enlarged uterine size. Figure 10.3c, enhanced coronal CT image shows this uterine myoma (arrow) protruding externally from the uterine body (arrowhead).
Case 4
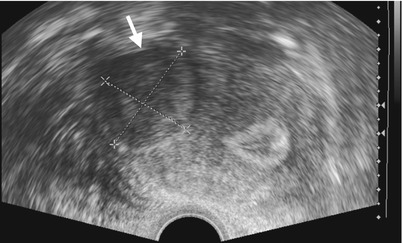
Fig. 10.4
Figure 10.4, ultrasound (US) of the uterus shows a well-defined hypoechoic mass (arrow) in the myometrium of the uterus.
Case 5

Fig. 10.5
Figure 10.5, axial T2-weighted image (T2WI) of magnetic resonance imaging (MRI) shows a homogeneous low signal intensity and well-demarcated mass (arrow) within the uterine body. Another small uterine myoma (arrowhead) has identical imaging features.
Case 6
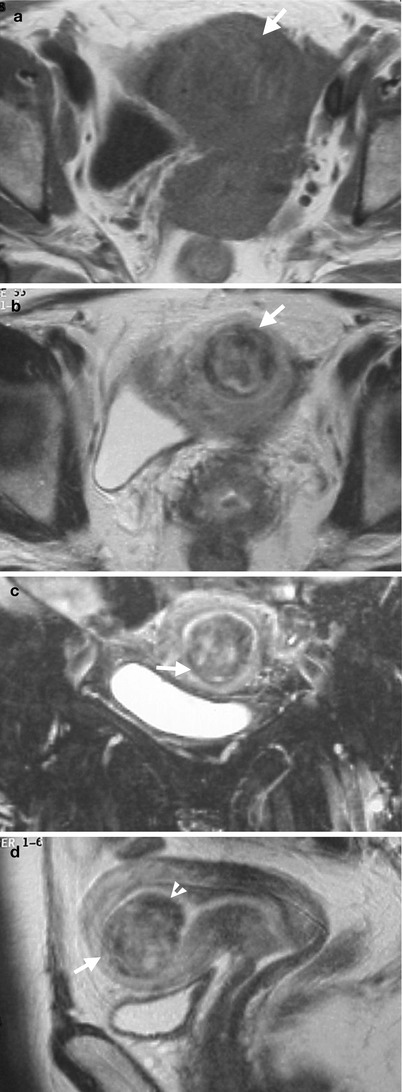
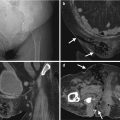
Fig. 10.6
Magnetic resonance imaging (MRI) shows imaging findings of a uterine myoma with submucosal location. Unenhanced axial T1-weighted image on MRI (Fig. 10.6a) shows faint visualization of the uterine myoma (arrow) due to its isointensity to the normal uterine myoma. Unenhanced axial (Fig. 10.6b), coronal (Fig. 10.6c), and sagittal (Fig. 10.6d) T2-weighted images on MRI show clearly visualization of the uterine myoma (arrows). This myoma has heterogeneous signal intensity on MRI due to degenerative change.
Key Diagnostic Features
Uterine myomas are located in the myometrium of the uterus. Uterine myomas could be categorized by their locations as submucosal, intramural, and subserosal myomas [1]. Submucosal myomas protrude internally and cause deformed uterine cavity. Subserosal myomas protrude externally with a resultant lobulated uterine surface. On images, uterine myomas are diagnosed by confirmation of their anatomical locations as well-defined masses within the myometrium and their typical imaging findings as well as the presence or absence of calcifications and degenerations within the tumors. Ultrasound is usually the first-line imaging modality for uterine myomas [1]. On ultrasound, a uterine myoma usually presents as a hypoechoic or heterogeneous mass of round or oval shape relative to the normal myometrium [1]. In the absence of calcifications and degeneration of uterine myomas, they show similar density to that of normal uterine myometrium on unenhanced computed tomography (CT) and homogeneously hypodense to the uterus on enhanced CT. Calcification is a specific sign of uterine myomas but only found in 10 % of patients [2]. Plain radiographs of the kidney, ureter, and bladder, excretory urography, or CT could detect a calcified uterine myoma by its typical calcified pattern and anatomical location. On MRI, T2-weighted images are most useful for demonstrating uterine myomas which are typically shown as homogeneous low signal intensity masses [1, 2]. Uterine myomas are usually well-defined masses on MRI. Uterine myomas with degenerative changes show heterogeneous density on CT and heterogeneous signal intensity on MRI [2].
10.3 Adenomyosis
Case 7
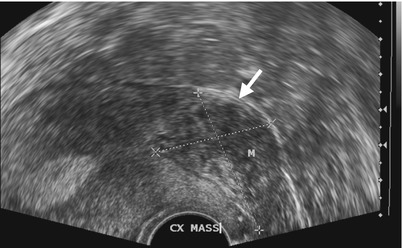
Fig. 10.7
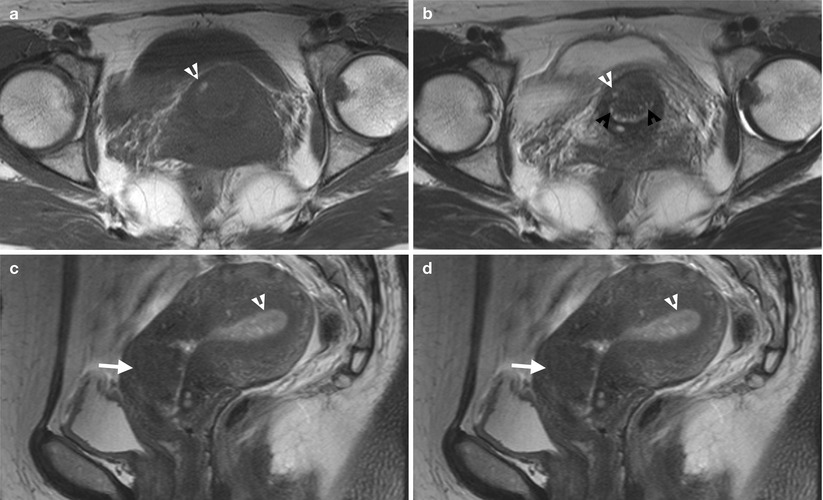
Fig. 10.8
Ultrasound (US) and magnetic resonance imaging (MRI) illustrate imaging findings of adenomyosis. Figure 10.7, ultrasound of the uterus shows a mass lesion (arrow) at the uterine cervix. Figure 10.8a, axial T1-weighted image of MRI shows an isointensity mass lesion at the anterior lip of the uterine cervix. A small hyperintense focus (arrowhead) in the mass is noted. Figure 10.8b, axial T2-weighted image of MRI shows this uterine cervix mass with hyperintense foci (white arrowhead) at the same site as that of Fig. 10.8a, representing hemorrhage. Other hyperintense foci (black arrowheads) in the mass represents endometrial tissue. Figure 10.8c, sagittal T2-weighted image shows ill-defined appearance of this mass (arrow).
Key Diagnostic Features
Adenomyosis is defined as the presence of ectopic endometrial tissue in the myometrium. Adenomyosis is categorized into diffuse and focal forms. Focal adenomyosis shows imaging finding of a uterine mass on ultrasound, which could be indistinguishable from uterine myomas. Diffuse adenomyosis results in uterine enlargement with thickened transitional zone more than 12 mm as shown on T2-weighted image of MRI [1]. Focal adenomyosis shows a uterine mass with an ill-defined border relative to normal uterine tissue, which contains some small hyperintense foci on T2WI, representing hemorrhage or endometrial tissue [1].
10.4 Uterine Leiomyosarcomas
Case 8
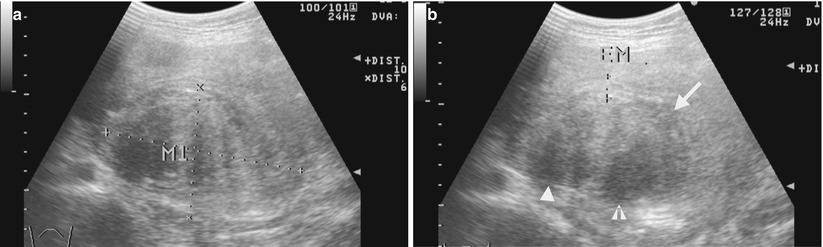
Fig. 10.9
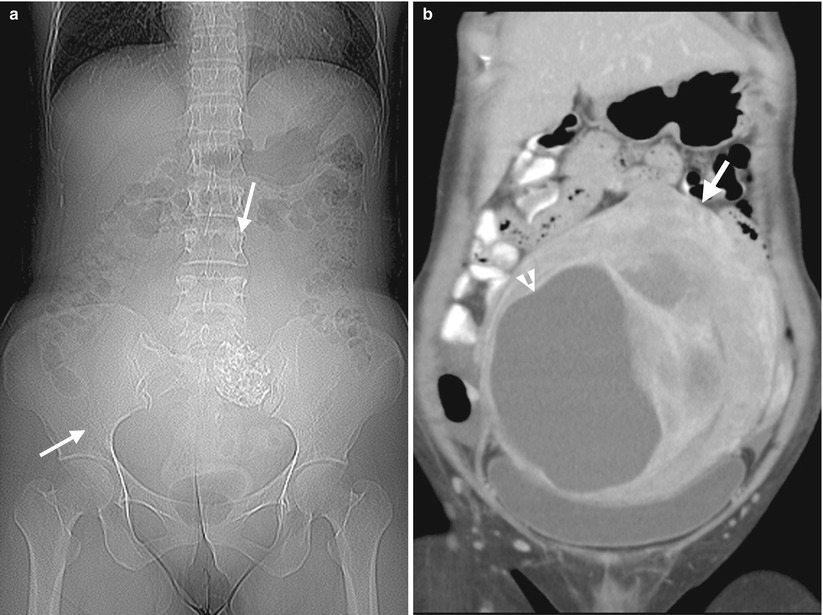
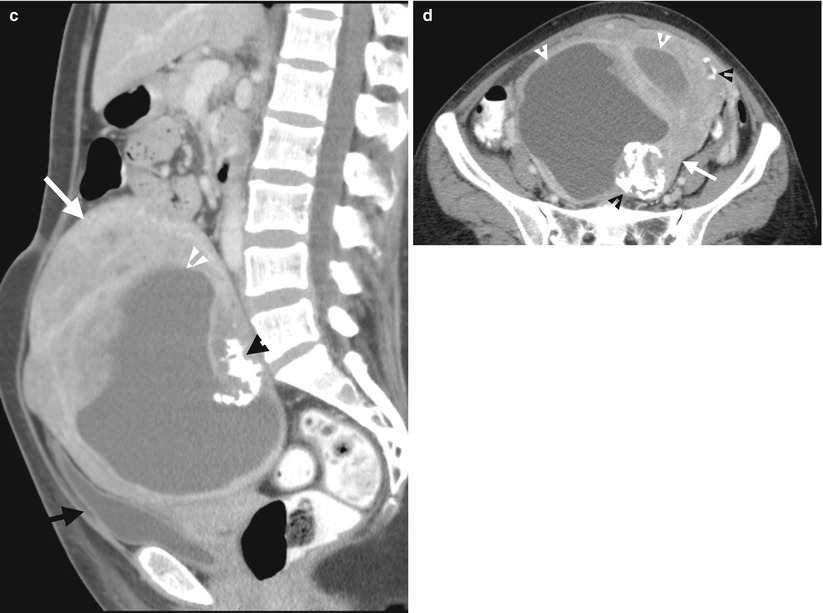
Fig. 10.10
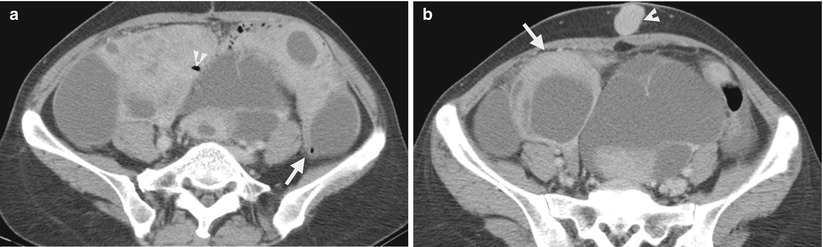
Fig. 10.11
Ultrasound (US) and computed tomography (CT) studies before and after surgery show imaging findings of a uterine leiomyosarcoma. Figure 10.9a, uterine US shows a large uterine mass (M1) with heterogeneous echogenicity. Figure 10.9b, uterine US shows two cystic areas (arrowheads) in this uterine mass (arrow) which compress the endometrial cavity. Figure 10.10a, CT scout image shows a large space-occupying lesion (arrows) at the lower abdominal and pelvic cavity. Figure 10.10b, coronal enhanced CT image shows a large uterine mass (arrow) with both solid and cystic (arrowhead) parts, located superior to the urinary bladder. Figure 10.10c, sagittal enhanced CT image shows the uterine mass (white arrow) compressing the urinary bladder (black arrow). There are solid, cystic (white arrowhead), and calcified (black arrowhead) parts in this huge mass. Figure 10.10d, axial enhanced CT image shows heterogeneous density of this uterine mass (white arrow) by the presence of cystic (white arrowheads), calcified (black arrowheads), and solid parts. Histological examination of surgical specimens of hysterectomy reveals a uterine leiomyosarcoma. Figure 10.11a, enhanced axial image of follow-up CT 18 months after hysterectomy shows metastatic leiomyosarcoma occupying nearly the whole upper pelvic cavity with the involvement of the small bowel loop (arrowhead) and the descending colon (arrow). Figure 10.11b, enhanced axial CT, 3 cm caudal to Fig. 10.11a, shows an abnormal nodule (arrowhead) in the midline of the subcutaneous area and bilateral adnexal mixed cystic and solid masses (arrow), consistent in metastasis.
Key Diagnostic Features
Uterine leiomyosarcoma is an uncommon uterine malignancy. Uterine leiomyosarcomas could not be reliably differentiated from leiomyomas with degenerative changes by imaging features on ultrasound (US), computed tomography (CT), or magnetic resonance image (MRI). However, CT could assess metastasis from a uterine leiomyosarcoma [1]. On MRI, a uterine mass in the myometrium presenting as huge size and with heterogeneous signal intensity and hemorrhage and necrosis should alert the readers of the possibility of a uterine leiomyosarcoma [2]. A close follow-up of the patients by images is necessary because the diagnosis of a uterine leiomyosarcoma is sometimes established after occurrence of metastasis. It is because of the difficulty of establishing histological diagnosis to some uterine leiomyosarcomas at the time of myomectomy or hysterectomy and some leiomyomas undergoing malignant transformation.
10.5 Endometrial Carcinoma
Case 9

Fig. 10.12
Magnetic resonance imaging (MRI) shows imaging findings of myometrium and cervix invasion by endometrial carcinoma. Unenhanced sagittal (Fig. 10.12a) and axial (Fig. 10.12b) axial T2-weighted images show mass lesions (arrows) of intermediate signal intensity in the uterine cavity. Myometrial invasion (black arrowheads) is depicted by tumor signal intensity in the inner part of the myometrium contiguous to the endometrial masses with irregular interface. The endometrial tumor invades the uterine cervix showing a focal intermediate signal mass (white arrowheads) replacing normal low signal intensity of uterine cervix stroma.
Case 10
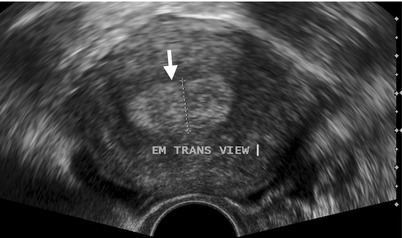
Fig. 10.13

Fig. 10.14
Transvaginal ultrasound and magnetic resonance imaging (MRI) show imaging findings of a patient with endometrial carcinoma confined in the endometrium. Transvaginal ultrasound (Fig. 10.13) shows abnormal thickening of the endometrium (arrow) with heterogeneous echogenicity. Unenhanced axial T1-weighted image (Fig. 10.14a) of MRI shows enlarged uterus with no clear visualization of the tumor. Unenhanced axial T2-weighted image (Fig. 10.14b) of MRI shows irregular masses of intermediate signal intensity (arrow) in the endometrial cavity, consistent with endometrial carcinoma. Enhanced axial T1-weighted fat-suppressed image (Fig. 10.14c) of MRI shows heterogeneous enhancement of the endometrial tumor (arrow), less than that of normal myometrium. Note the preservation of myometrium thickness at the interface of the endometrial tumor suggests no myometrial invasion, which is proved by subsequent histological examination of hysterectomy specimen.
Case 11
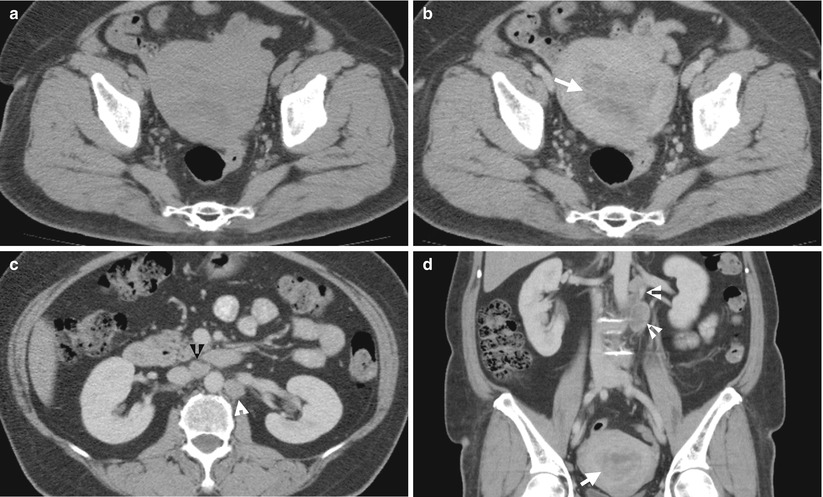
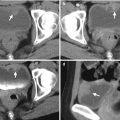
Fig. 10.15
Computed tomography (CT) shows imaging findings of advanced endometrial carcinoma with lymph node metastases. Unenhanced (Fig. 10.15a) and enhanced (Fig. 10.15b) axial CT images at the uterus level show enhancing soft tissue mass in the uterine cavity (arrow), consistent with endometrial carcinoma, which is not conspicuous before contrast medium administration. Enhanced axial CT image at the renal level (Fig. 10.15c) and coronal image (Fig. 10.15d) show abnormally enlarged lymph nodes at the para-aortic (white arrowheads) and aortocaval (black arrowhead) areas, respectively, representing lymph node metastases by the endometrial carcinoma (arrow).
Key Diagnostic Features
Imaging provides preoperative staging and helps select treatment planning for endometrial carcinomas [3]. Endometrial carcinoma is a common malignant tumor of the uterus [3]. The diagnosis of endometrial carcinoma basically relies on histological examination, and its most common histological type is endometrioid type [3]. Magnetic resonance imaging (MRI) is the most accurate for staging of endometrial cancers. MRI could evaluate the presence and depth of myometrial invasion as well as cervical invasion by endometrial cancer [3]. Irregular interface between endometrial carcinoma and adjacent myometrium indicates myometrial invasion [3]. Unenhanced T2-weighted image and enhanced dynamic images on T1-weighted fat-suppressed images are most valuable in assessing myometrial invasion [3]. The uterine cervix stroma loses its normal low signal intensity and is replaced by intermediate signal intensity mass suggesting uterine cervix invasion by endometrial carcinoma [3]. Transvaginal ultrasound is usually the first-line imaging tool for evaluating patients with clinical suspicion of endometrial carcinomas, who usually present with postmenopausal vaginal bleeding [3]. Endometrial thickness of 5 mm on transvaginal ultrasound has been proposed as an imaging criterion for diagnosing endometrial carcinomas [3]. However, MRI has better performance for evaluating myometrial invasion by endometrial carcinomas than transvaginal ultrasound [3]. The use of computed tomography (CT) should be reserved for advanced endometrial cancers [3]. It is because CT has poor performance in assessing myometrial and uterine cervix invasion by endometrial cancer [3]. However, CT could diagnose bladder invasion, pelvic wall invasion, lymph node metastasis of the abdomen and pelvic cavity, or distant organ metastasis by endometrial carcinomas [3].
10.6 Uterine Lymphoma
Case 12
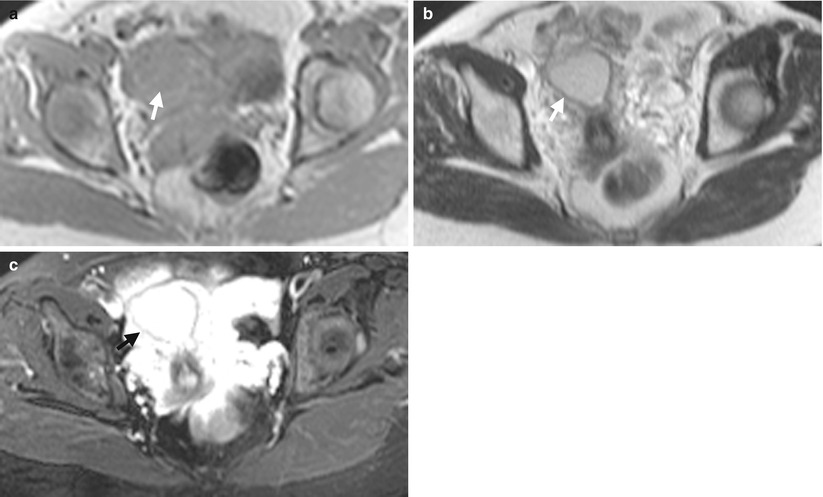
Fig. 10.16
Magnetic resonance imaging (MRI) shows imaging findings of a primary uterine lymphoma. Unenhanced axial T1-weighted image of MRI (Fig. 10.16a) shows a homogeneously low signal intensity mass (arrow) of the uterine corpus. Unenhanced axial T2-weighted image of MRI (Fig. 10.16b) shows homogeneous intermediate signal intensity of this uterine mass (arrow). Enhanced axial T1-weighted fat-suppressed image (Fig. 10.16c) of MRI shows obvious and homogeneous contrast enhancement of this mass (arrow). Biopsy of this uterine mass shows diffuse large B cell lymphoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree