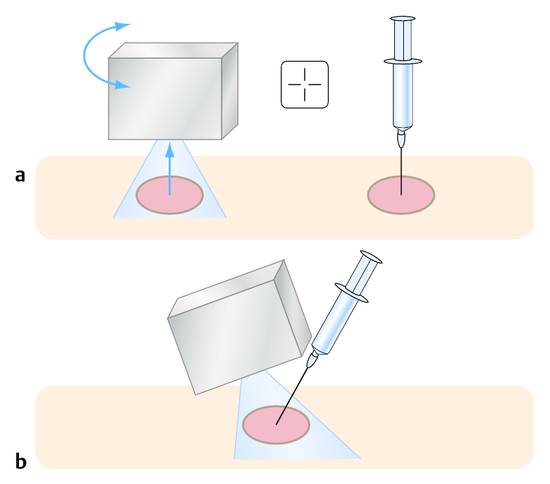
Fine Needle Aspiration Biopsy and Core Needle Biopsy The first percutaneous needle biopsy with localization by palpation and inspection was documented in 1856 by Albrecht Theodor Middeldorpf (1824–1868) in his “Overview of Akidopeirastik, a New Diagnostic Method Using Sharp Pointed Tools.”1 The advent of ultrasonography more than a century later made the diagnostic puncture of small intra-abdominal masses possible. In 1969, Kratochwill performed one of the first ultrasound-guided amniocentesis procedures using a Kretz biopsy transducer and localization by A-mode ultrasound.2 Holm and Rasmussen3 were among the first authors to describe percutaneous biopsies guided by dynamic B-mode ultrasound in the early 1970s. This technique became a safe and established method of tissue sampling for the diagnosis of masses that could be visualized by ultrasonography. Before performing an aspiration or core biopsy, the operator must decide what type of needle to use. Several questions should be answered in making this decision. A fine needle, defined as a needle less than 1 mm in diameter, is sufficient to sample material for cytologic analysis. A fine needle may also be able to harvest small tissue aggregates when inserted with a slight twisting motion, depending on the consistency of the target site. These tissue aggregates, like blood clots, should be immersed in formalin for histologic processing. This “mini-histology” can result in a more accurate diagnosis4 (Chapters ▶ 5 and ▶ 6). In many cases a cytologic analysis is inadequate, especially in well-differentiated tumors, and a larger specimen is needed for histologic evaluation.5 Several studies have documented the superiority of a combined histologic-cytologic analysis (fine needle aspiration plus core needle biopsy) over histology and cytology alone (▶ Table 14.1, ▶ Table 14.2). Löschner showed in his study that a combination of fine needle and core needle biopsy increased diagnostic sensitivity, but that the gain depended on the organ biopsied.6 We use Chiba needles (0.7-mm), among others, to reach targets located farther from the skin, and we use a 21-gauge needle (green) or 22-gauge needle (black) for more superficial targets (e.g., inguinal lymph nodes). Even in the case of a palpable superficial mass, the lesion and its surroundings should be evaluated with ultrasound before the biopsy is performed. Time and again, we encounter difficult surroundings that are made clearer by ultrasound, enabling us to sample the lesion with precision. The needle may be inserted after first imaging the lesion with ultrasound and marking the skin, or a short needle may be introduced freehand under continuous ultrasound guidance as in the fine needle aspiration of cervical lymph nodes (▶ Fig. 14.1). Fig. 14.1 a Principle of the freehand technique. The superficial mass is visualized with ultrasound, and the puncture site is marked on the skin. The needle is inserted without direct ultrasound guidance (e.g., for the aspiration of pleural effusion or ascites). b Ultrasound-guided technique. The needle is introduced alongside the transducer and is angled slightly for better visualization (see Chapter ▶ 27, Interventional Thyroid Ultrasound). Needle calibers of 21 gauge (green) or 22 gauge (black) are used to harvest cells for cytology, and various types of core needle (≥1 mm in diameter) are used for histology (Chapter ▶ 2
14.1 Historical Background
14.2 Description of Biopsy Techniques
14.2.1 What Type of Needle Should Be Used?
Does the Investigation Require a Fine Needle or Core Needle?
Organ
Sensitivity (%)
CNB
FNA
CNB + FNA
Liver
89.5
81.6
97.4
Kidney
75
83.3
91.7
Pancreas
60
80
90
Lymph nodes
100
90
100
Abbreviations: CNB: core needle biopsy; FNA: fine needle aspiration.
Source: Löschner C. Retrospektive Analyse der ultraschallgestützten diagnostischen Feinnadelpunktion im onkologischen Patientengut eines Versorgungskrankenhauses und prospektive Bewertung der Doppelpunktion. Inauguraldissertation zur Erlangung des akademischen Grades Doktor der Medizin. Rostock; 2008: table 38, p.44, with kind permission of C. Löschner.
Author
n
Sensitivity (%)
FNA
CNB
FNA + CNB
Swobodnik 1990a
1213
83
72
Not stated
Buscarini 1990b
2091
91
93.5
97.4
Wernecke 1991c
180
87
86
94
Tikkakoski 1993d
155
86
86
97
Borzio 1994e
100
78
81
96
Nürnberg 1997f
101
84.5
84.5
95.8
Abbreviations: CNB, core needle biopsy; FNA, fine needle aspiration.
Source: Löschner C. Retrospektive Analyse der ultraschallgestützten diagnostischen Feinnadelpunktion im onkologischen Patientengut eines Versorgungskrankenhauses und prospektive Bewertung der Doppelpunktion. Inauguraldissertation zur Erlangung des akademischen Grades Doktor der Medizin. Rostock; 2008: table 39, p.44, with kind permission of C. Löschner.
aSwobodnik W, Janowitz P, Kratzer W, Wechsler JG. Vergleich ultraschallgezielter Fei- und Grobnadelpunktionen bei umschriebenen Läsionen im Abdomen. Ultraschall Med 1990; 11: 287–289.
bBuscarini L, Fornari F, Bolondi L et al. Ultrasound guided fine needle biopsy of focal liver leasions: techniques, diagnostic accuray and complications. A retrospectiv study on 2091 biopsies. J Hepatol 1990; 11: 344–348.
cWernecke K, Mertens G, von Bassewitz DB, Peters PE. Möglichkeiten und Grenzen der perkutanen Nadelbiopsie in der histologischen Klassifikation von malignen Tumoren. RoFo 1991; 155: 538–544.
dTikkakoski T, Paivansalo M, Siniluoto T et al. Percutaneous ultrasound-guided biopsy. Fine needle biopsy, cutting needle biopsy, or both? Acta Radiol 1993; 34: 30–34.
eBorzio M, Borzio F, Macchi R et al. The evaluation of fine-needle procedures for the diagnosis of focal liver lesions in cirrhosis. J Hepatol 1994; 20(1): 117–121.
fLöschner Ch, Nürnberg D, Jung A. Stellenwert und Ergiebigkeit der ultraschall-gezielten Fein- und Grobnadelpunktion in der onkologischen Diagnostik – Vorteil der “Doppelpunktion”. Endoskopie heute 1997; 10: 84.
How Long is the Needle Path?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree