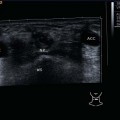
8 Floor of the Mouth and Oropharynx Inspection, bimanual palpation, and laryngoscopy are the classic procedures for examining the tongue, floor of the mouth, and oropharynx. There are two basic ways of performing an ultrasound examination in this area: transcutaneously, that is, through the soft tissues of the neck, and intraorally, in which the ultrasound probe is covered, for example, with a glove, and inserted into the mouth (Figs. 8.1, 8.2). However, special probes exist for application in the oral cavity and deeper areas of the oropharynx and hypopharynx. Bony structures (the horizontal ramus of the mandible and the hyoid bone), which can be seen as hyperechoic reflections with distal acoustic shadowing, are initially used as landmarks when examining the floor of the mouth, tongue, and oropharynx. Like the other muscles in the head and neck, muscles in the floor of the mouth are hypoechoic, while the intrinsic muscles of the tongue appear homogeneously echogenic. The longitudinal, transverse, and vertical groups of muscle fibers can be seen in both transverse and longitudinal views as more echogenic or punctate hyperechoic reflections. The surface of the tongue is easily recognized from the hyperechoic curved line of the air–tissue interface. The penetration depth for examining the whole tongue should be set at 70 mm, with appropriate adjustments of the frequency, focus, and gain. A routine demonstration of the palate and posterior wall of the pharynx with the transcutaneous approach is hampered by the reflection of the ultrasound waves due to the air within the oral cavity. Demonstration of the tip of the tongue, which is surrounded by air, is similarly problematic in transcutaneous ultrasonography, but this area can easily be examined clinically by inspection and palpation. In addition, intraoral ultrasound may be of use here. After the acoustic shadow of the mandible, the first structures to be identified on transcutaneous examination in the transverse plane, starting at the point of the chin, are the rounded anterior bellies of the digastric muscles (Fig. 8.3; The geniohyoid muscles, which lie between the mylohyoid muscles spanning the horizontal rami of the mandible and the genioglossus muscles, can be identified from their typical hypoechoic structures and distinguished from the echogenic intrinsic muscles of the tongue. The entire length of the tongue, including its base, can be assessed by moving the ultrasound probe down to the hyoid. The lingual arteries can be demonstrated at the transition of the middle to posterior third of the tongue as round hypoechoic or anechoic structures (Figs. 8.4, 8.5; The tonsillar bed can be examined if the ultrasound probe, held slightly above the hyoid bone in the transverse plane, is tilted laterally in the submandibular region. The tonsil appears as a hypoechoic, relatively well-defined structure with multiple echogenic reflections due to small inclusions of air (Fig. 8.6). The sonographic appearance of the paltine tonsils may resemble the shape of a scallop. The size of the tonsils depends on age and shows great interindividual variation. Below the hypoechoic infrahyoid muscles, the somewhat more echogenic preepiglottic fatty tissue can be demonstrated between the hyoid and upper edge of the thyroid cartilage (Fig. 8.7). After identification of these landmarks, both the transverse and longitudinal views must be checked carefully for any pathological findings. In infections and inflammatory conditions of the floor of the mouth, tongue, and oropharynx, a distinction has to be made between a phlegmon and an abscess. A phlegmon in the floor of the mouth can be identified as diffuse hypoechoic areas lying between the different layers of tissue, which often appear blurred and loosely structured (Figs. 8.8, 8.9), while an abscess in the floor of the mouth can be recognized as a clearly defined hypoechoic space-occupying lesion, containing hypoechoic to anechoic central structures with distal acoustic enhancement (Figs. 8.10, 8.11). Perfusion in the inflamed tissue areas is usually increased. A visible gap in the hyperechoic contour line may be identified at the position where a dental abscess has breached the mandible (Fig. 8.12). Acute inflammatory conditions affecting the palatine tonsils are seen as an enlargement with hypoechoic change and loss of clear demarcation from the surrounding tissues. It is not possible to use ultrasound to unambiguously distinguish an intra-, peri-, or retrotonsillar abscess from an acute tonsillitis, but ultrasound may support the provisional diagnosis (Figs. 8.13, 8.14, 8.15; A hypoechoic, clearly defined space-occupying lesion touching the tonsillar bed can be identified on the ultrasound image. It shows the typical signs of an abscess: a central anechoic area, possibly with isolated internal echoes indicating cell debris, and distal acoustic enhancement. Ultrasound may sometimes be a very useful diagnostic tool and examination can also be performed when there is trismus related to infection or inflammation. Progression of the infection may result in a parapharyngeal abscess (Figs. 8.16, 8.17, 8.18) or phlegmon (Figs. 8.19, 8.20; Pearls and Pitfalls Comparison of the two sides is invaluable in deciding whether there is a tonsillar abscess. A split-screen display is extremely helpful here, as the two sides can be seen simultaneously in the corresponding plane and compared directly with each other. Branchial cysts and fistulas lying laterally in the neck are mostly related to the second branchial (pharyngeal) cleft, as this is the largest in size and persists longest during embryonic development. A cyst or fistula developing here has a close positional relationship to the carotid bifurcation; if there is an internal sinus, it opens into the supratonsillar fossa (Fig. 8.21). The cyst sac usually lies laterally to the internal jugular vein and caudally to the posterior belly of the digastric muscle. Malformations of the second, third, and fourth branchial clefts are considerably less common. Ultrasound scans show clearly defined cysts that are round or oval, lying in levels II and III. Sonographic palpation allows the fluid contents to be felt. The homogeneous internal echoes range in the classic description from anechoic to hypoechoic and are more echogenic when infected. Likewise, distal acoustic enhancement is characteristic, as is the lack of perfusion seen in the inner space on color-coded duplex sonography (CCDS) (Figs. 8.22, 8.23, 8.24; Correlating with the clinical picture, the distinct margins of a branchial cyst can be partially or completely lost and the demarcation from the sternocleidomastoid muscle becomes indistinct when an acute super-infection intervenes. CCDS shows considerable hyperperfusion of the tissue periphery. The internal echotexture is inhomogeneous with echogenic secretory elements (Fig. 8.28; The pathogenesis of thyroglossal duct cysts and fistulas, lying in the midline, is closely linked to the embryonic development of the thyroid gland in the neck. The frequently extremely elastic space-occupying lesions found in the midline between the chin and the thyroid gland (very rarely, also suprasternally) are usually noted during or after an infection. Thyroglossal duct fistulas become apparent from the opening found at the level of the superior thyroid notch and the secretions released at this point: infections with corresponding purulent secretions and abscess formation may occur. As expected, B-mode ultrasonography shows the cysts lying in close anatomical proximity to the hyoid bone (Figs. 8.29, 8.30; The ultrasound characteristics of benign tumors in the floor of the mouth, tongue and oropharynx are no different from the findings for similar tumors elsewhere in the head and neck. Lipomas, hemangiomas, and lymphangiomas can be assessed in relation to surrounding structures. The surgical approach (transoral or transcervical) can be selected on the basis of the findings. Benign tumors are described in more detail in Chapters 6 and 10. Pearls and Pitfalls Solid tumors of the oral cavity, particularly those suspected of being associated with the small salivary glands, are more frequently malignant than tumors of the parotid or submandibular glands. Salivary gland retention cysts can, similarly to the ranula, be identified on the basis of the typical ultrasound criteria for a cyst containing clear secretions: they are clearly defined, are homogeneously anechoic, and exhibit a marked distal acoustic enhancement without perfusion on CCDS (Figs. 8.31, 8.32). This usually makes it possible to distinguish a cyst from a solid thyroid tumor. The hour-glass figure of a “plunging ranula” extends outward through the muscles of the floor of the mouth to the submandibular bed. The possibility of an epidermoid cyst should be considered if the constellation of features consists of the typical site for a ranula together with an echogenic internal echo pattern (Figs. 8.33, 8.34; A hypoechoic, cloud-shaped extension of the base of the tongue with central echogenic reflections corresponds to the endoscopic finding of lymphatic hyperplasia of the lingual tonsil (Fig. 8.35). Cystic changes in the base of the tongue must be assessed in relation to the hyoid bone to distinguish a tongue-base cyst from a thyroglossal duct cyst (Fig. 8.36). If a space-occupying lesion that appears homogeneously hyper-echoic is found at the base of the tongue, the possibility of ectopic thyroid tissue has to be considered (Fig. 8.37). This may show marked perfusion on CCDS. Pearls and Pitfalls Ectopic thyroid tissue of clinical relevance is frequently found in patients following a thyroidectomy. Surgical removal of this tissue may result in a hormonal insufficiency. Solid benign tumors are rare and can often be falsely identified as cysts (Figs. 8.38, 8.39). Malignant tumors are seen on ultrasound examination as hypoechoic and inhomogeneous lesions. Their margins are frequently ill defined, although this is not an essential sonographic sign of malignant growth seen with ultrasound. As already indicated, the diagnosis must be confirmed on histology. Ultrasonography helps to determine the approximate size and extension of most primary tumors prior to therapy.
Anatomy
 Video 8.1).
Video 8.1).
 Video 8.2).
Video 8.2).
Inflammatory Changes
 Videos 8.3, 8.4, 8.5).
Videos 8.3, 8.4, 8.5).
 Video 8.6) in the neck.
Video 8.6) in the neck.
Benign Tumors
Branchial Cysts
 Videos 8.7, 8.8). Modern high-resolution ultrasound systems even demonstrate the glycoproteins as finely dispersed “floating” echoes. Under favorable conditions, the path of a branchial fistula or sinus can be followed right into the oropharynx (Figs. 8.25, 8.26, 8.27;
Videos 8.7, 8.8). Modern high-resolution ultrasound systems even demonstrate the glycoproteins as finely dispersed “floating” echoes. Under favorable conditions, the path of a branchial fistula or sinus can be followed right into the oropharynx (Figs. 8.25, 8.26, 8.27;  Videos 8.9, 8.10).
Videos 8.9, 8.10).
Infected Branchial Cysts
 Videos 8.11, 8.12).
Videos 8.11, 8.12).
Thyroglossal Duct Cysts and Fistulas
 Video 8.13). The cyst sac is situated caudal, cranial, anterior, and/or posterior to the hyoid bone. The extent of a sinus or cyst can be determined precisely during the preoperative planning; how far it extends into the base of the tongue can be assessed without difficulty in the transverse and longitudinal ultrasound views. The differential diagnosis includes cysts originating from the base of the tongue and larnygoceles.
Video 8.13). The cyst sac is situated caudal, cranial, anterior, and/or posterior to the hyoid bone. The extent of a sinus or cyst can be determined precisely during the preoperative planning; how far it extends into the base of the tongue can be assessed without difficulty in the transverse and longitudinal ultrasound views. The differential diagnosis includes cysts originating from the base of the tongue and larnygoceles.
Other Benign Tumors
 Video 8.14).
Video 8.14).
Malignant Tumors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree