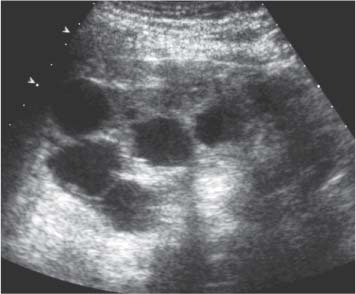
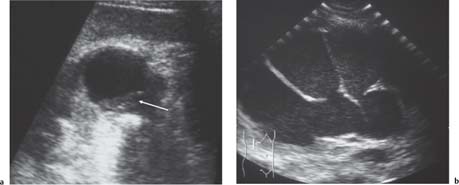
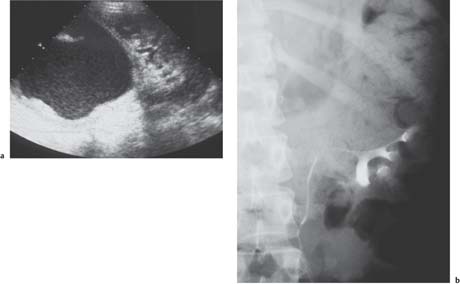
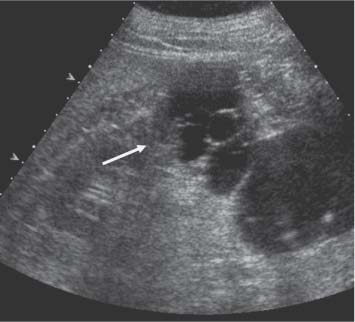
8 Focal Lesions of the Kidney Many focal renal lesions are detected incidentally during investigation for other symptoms. Ultrasound is commonly used in the investigation of diverse abdominal and pelvic symptoms; the kidneys are seen as part of the ultrasound examination. The most likely finding is of a simple renal cyst, and ultrasound has a high degree of accuracy in cyst characterization.1 The mode of presentation of renal tumors gives prognostic information; those that are found incidentally do better than those who present with symptoms.2 It is important for the ultrasonologist to recognize which lesions can be ignored and which need further action. Simple renal cysts are common in older patients; they are a normal part of the process of aging and are the commonest renal mass in adults. A recent prevalence study using ultrasound showed that 5.1% of people in the fourth decade of life have at least one cyst; this increases sevenfold to 36.1% in the eighth decade of life.3 The same study also showed that cysts were twice as common in men as in women. Furthermore, there is an average yearly increase in size of 6.3%. Uncomplicated cysts are usually asymptomatic and do not require any treatment. Large cysts are likely to be symptomatic with pressure effects on adjacent structures, leading to discomfort, hematuria, hypertension, and urinary obstruction. Symptomatic renal cysts can be treated using ultrasound-guided aspiration and instillation of either absolute alcohol alone or alcohol and tetracycline.4,5 Success in relieving symptoms is said to be between 75 and 95%. Fig. 8.1 Simple cortical cyst (between cursors), demonstrating the characteristic features of a cyst: No internal echoes, an ovoid shape, an imperceptible, smooth wall, and increased through transmission of sound The ultrasound features are of a hypoechoic fluid collection arising from the kidney with the following characteristics (Fig. 8.1): • No internal echoes • A rounded or ovoid shape • An imperceptible, smooth wall, with a sharply-defined distal margin • Increased through transmission of sound There are technical factors that influence these appearances. Reverberation echoes from the skin surface or strong superficial reflectors may appear within the cyst. These echoes fade out the deeper into the cyst they go. Harmonic imaging will reduce this effect. Cysts < 2 cm in size may show apparent internal echoes from partial volume effects from adjacent solid tissue. Remember that the ultrasound beam has width. The presence of more than one simple cyst in a kidney becomes commoner with increasing age. These cysts retain the characteristics of a simple cyst (Fig. 8.2). Some medical syndromes produce multiple cysts, but once established these syndromes have innumerable cysts affecting both kidneys equally. In contrast, multiple simple cysts affect the two kidneys in an asymmetric way and always remain countable in number. Fine septations of < 1 mm thickness do not stop a simple cyst from being regarded as simple. Thicker septations, particularly those with nodular thickening, are suspicious for malignancy and require further investigation (Fig. 8.3). Rarely, a cyst may change over time to become more septated and show malignant features.6Computed tomography (CT) imaging is advocated for any cyst that deviates from being simple.7 Some authors advocate the use of Doppler studies or micro-bubble contrast-enhanced Doppler studies of septated lesions. It has been shown that flow in the septa, particularly high-velocity, pulsatile flow is a marker for malignancy.8,9 Internal echoes within a cyst are usually the result of either infection or hemorrhage (Fig. 8.4). The rate of hemorrhage into simple cysts is usually quoted as 6%, though the relevant studies were performed 30 years ago, predating sophisticated ultrasound. Cysts of polycystic kidney disease suffer a greater rate of hemorrhagic complication, in part due to the large size of the kidneys and their vulnerability to trauma. The appearance of a hemorrhage will vary with time. A fresh hemorrhage is anechoic, gaining echoes over time. Eventually, clot retraction, nodule and septum formation, calcification, and thickening of the cyst wall will occur. Hemorrhagic cysts are associated with malignancy;10 they may themselves mimic features of malignancy that lead to unnecessary surgery.11 Aspiration cytology is unhelpful because of the frequency of false negative results. If CT or magnetic resonance (MR) imaging do not show any overt features of malignancy, then follow-up of hemorrhagic cysts with serial ultra-sound imaging is prudent. Infection of a cyst can occur via hematogenous spread or via iatrogenic cyst puncture. An infected cyst may be indistinguishable from a simple cyst but is likely to show a complex echo pattern. The contents may be highly reflective (Fig. 8.4), there may be fluid–fluid levels with dependant debris and there may be contained gas. The wall of the cyst becomes thicker and may appear nodular due to adherent inflammatory tissue and an infected cyst will have clinical features of an abscess. Both are characterized by fever and flank pain resistant to antibiotic therapy. Aspiration and drainage are required for diagnosis and treatment.12 Fig. 8.2 Five simple cysts of similar size in the kidney of a 60-year-old. All demonstrate the typical features of a simple cyst Fig. 8.3 Septated cyst. The septations in this cyst are thicker than 1 mm, and therefore the lesion requires further investigation Hydatid (echinococcosis) cysts of the kidney represent a rare form of renal infection. Renal involvement occurs in only 4% of confirmed hydatid disease.13 The ultrasound appearances are nonspecific, but daughter cysts within the main cyst and fine wall calcification may aid in the diagnosis. There is eggshell-like mural calcification in about 3% of simple cysts (Fig. 8.5). The majority represent calcification that has occurred as a result of bleeding or inflammation and is seen as a thin, bright margin to the cyst.14 Fig. 8.4 a A fluid–debris level (arrow) within a cyst following recent intracystic hemorrhage. b Pyonephrosis in a longstanding hydronephrosis. Note that there is little or no remaining renal cortex. The fine echoes within the fluid indicate the presence of pus, blood, or other debris. The clinical picture is needed to aid in the differentiation of these entities Fig. 8.5 Calcified wall of a hemorrhagic cyst (arrow) at the upper aspect of the left kidney. (Courtesy of Dr. G.M. Baxter) Bright foci in the cyst walls or septa that show ring-down artifact are often seen but do not correlate with calcification on CT images.15 There is an association of renal cyst calcification with malignancy, but this is much less important in the diagnosis than the presence of soft-tissue nodules.16 Milk of calcium cysts contain a colloidal suspension of calcium crystals; these often show a dependant layer of high-reflective material on ultrasound, enough to cause shadowing.17 Milk of calcium cysts may masquerade as renal calculi but represent a calyceal diverticulum that has lost its communication with the collecting system.18 A milk of calcium cyst is usually asymptomatic. Fluid-containing lesions that communicate with the renal collecting system can be indistinguishable from simple cysts on ultrasound alone. Contrast-enhanced CT or urography is required to show the communication. Diagnostic confusion can arise in both directions; peri-pelvic cysts may mimic hydronephrosis and obstructed calyces may mimic a cyst.19,20 Likewise, the obstructed upper moiety of a duplex kidney may simulate an upper-pole renal cyst, especially if the surrounding cortex has become atrophic and nonfunctioning (Fig. 8.6). Conventionally, intravenous urography (IVU) is needed to establish the diagnosis. Nicolau et al. have claimed that measuring the size of the cystic structure on ultra-sound before and after a 1.5 L fluid load will reliably distinguish between a cyst and renal obstruction; an increase in size of the lesion indicates renal obstruction.21 Most authors prefer the greater certainty afforded by urography or contrast-enhanced CT imaging. Cysts in the renal sinus are produced in two forms: Parapelvic and peripelvic.22 Parapelvic cysts are parenchymal in origin and are usually solitary and are seen in about 1.5% of autopsies. Peripelvic cysts are thought to arise by lymphatic ectasia and are usually multiple and septated. Peripelvic lymphangiectasia is rare and is associated with perirenal lymphatic cysts, as well as perivascular cysts (probably dilated lymph vessels).23,24 The perirenal cysts appear to arise in a capsular location rather than a cortical location. Fig. 8.6 a Obstructed upper moiety of a duplex kidney. Atrophy of the renal cortex around the upper moiety has occurred. The fluid within the dilated collecting system contains echoes indicating pus, blood, or other debris. In this case, the upper moiety was infected. b IVU in the same patient, demonstrating the typical “drooping flower head” sign of a normal lower moiety being displaced by the nonfunctioning upper moiety A recent hematoma may be indistinguishable from a cyst. The diagnosis should be suspected in the light of a history of trauma and serial ultrasound will show the development of echoes within the lesion as the hematoma matures. Arteriovenous malformations and aneurysms may appear identical to a simple cyst on gray-scale ultrasound but will present no diagnostic difficulty if Doppler ultra-sound imaging is used.25 Occasionally CT will misinterpret a venous varix as an enhancing mass.26 This is a rare lesion that appears as a discrete, space-occupying mass with a thick capsule and consisting of several noncommunicating cysts of varying size separated by fibrous septa (Fig. 8.7).27,28 If the cysts are small, the lesion may appear as a more solid mass. Multilocular cystic nephromas are predominantly found in young males or older females. There is pathological disagreement on their origin and this has led to a confusing array of synonyms: Benign cystic nephroma, cystic hamartoma, multilocular cystadenoma, cystic Wilms tumor, benign cystic differentiated nephroblastoma, and segmental polycystic kidney, to name a few. Whatever the name given, it is not possible for ultra-sound or CT to distinguish the lesion from a cystic renal cell carcinoma (RCC). Fig. 8.7 Example of a multilocular cystic nephroma. The cysts are contained within the one lesion The seminal paper by Bosniak on the classification of renal cysts and the likelihood of malignancy was based on CT imaging, but the findings can be extrapolated to ultrasound.29 The initial premise was to identify reliably lesions that did not require surgery. Cysts are graded from I to IV depending on their internal complexity, with Grade I being a simple cyst and Grade IV being complex with solid areas. Approximately 60% of Grade III lesions and almost 100% of Grade IV lesions are malignant. Grades I and II can be left alone, whereas Grades III and IV require surgery. This approach has been shown to succeed,30 though some modifications to the classification have evolved. Biopsy of Grade III lesions is advocated to prevent unnecessary surgery31 and follow-up of moderately complex lesions (Grade IIF) is advised, as the absence of change supports benign disease.32
Introduction
Renal Cysts
Simple Cysts
Multiple Simple Cysts
Complicated Cysts
Septations
Hemorrhage
Infection
Calcification
Differential Diagnosis of Renal Simple Cysts
Calyceal and Renal Pelvic Diverticula
Hydronephrosis Duplex System
Lymphatic Cysts
Hematoma
Arteriovenous Malformations and Aneurysms
Multilocular Cystic Nephroma
Cystic Malignancy (Table 8.1.)
Category 1 | Cystic masses with well-defined margins, homogeneous, of water density, with no contrastenhancement |
Category 2 | Cystic masses showing a few thin septa (< 1 mm) orthin fine calcifications, or appearing as hyperdensecysts |
Category 3 | Cystic masses showing more extensive thickenedand irregular calcifications, uniform wall thickening, and thickened and irregular or multiple septa(> 1 mm) |
Category 4 | Cystic masses having irregular thickened walls orsolid elements and possibly having enhancement ofcyst walls, septa, or solid areas |
Fig. 8.8 Thickening of the upper cyst wall (arrow) in a large cystic renal carcinoma of the midaspect of the right kidney
Most cystic renal carcinomas (50%) are unilocular and represent necrosis within the renal tumor.33 Ultra-sound shows a thick, uneven wall with the cystic component containing echoes. Next most common (30%), the mass has several cystic spaces with thick nodular intervening masses containing adenocarcinoma. In 20%, there is a solid mass within the wall of a cyst (Fig. 8.8); this feature is usually caused by asymmetric necrosis. Rarely, the lesion is a unilocular cystadenocarcinoma with a thin layer of clear cells in the walls. Multilocular cystadenocarcinoma represents only 3% of renal cell tumors but follows a relatively benign clinical course.34
Congenital Cystic Renal Disease
Polycystic Kidney Disease
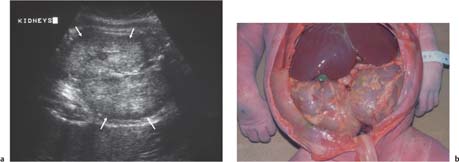
Autosomal recessive polycystic kidney disease (ARPKD) may present in utero or in childhood. The kidneys are symmetrically enlarged, smooth, and are of increased reflectivity due to the multiple tiny cysts being too small to individually resolve, but providing numerous reflective interfaces. However, a few small discrete cysts may be seen and a low-reflective rim may develop around the kidneys. Generally, ARKPD patients diagnosed in utero have a poor prognosis and may succumb from underdeveloped lungs caused by lack of amniotic fluid (Fig. 8.9). ARKPD patients diagnosed at an older age generally have better renal function but suffer from portal hypertension as a consequence of hepatic cysts and periportal fibrosis. Those ARKPD patients that survive the perinatal period have a better prognosis than is generally perceived.35
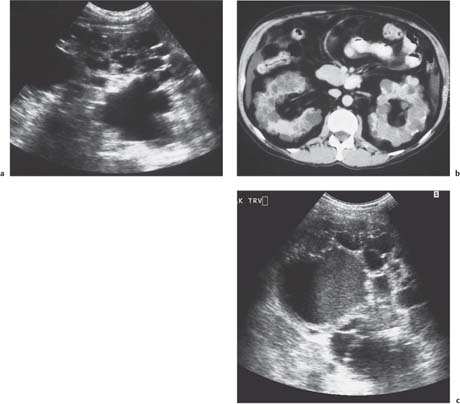
Autosomal dominant polycystic kidney disease (ADPKD) usually presents in the fourth or fifth decade of life with renal impairment, hypertension, hematuria, and abdominal pain. ADPKD may also be detected serendipitously during ultrasound imaging for other reasons. Screening of offspring of affected ADKPD adults is normally performed with ultrasound. Renal cysts are rare below age 30; finding two or more renal cysts in this age group with a family history of ADPKD indicates that the patient is also affected.36 Once the condition is established, innumerable cysts of varying sizes disrupt the normal architecture of the kidneys and both kidneys become considerably enlarged (Fig. 8.10). The size of the kidneys is related to renal function and hyper-tension; an increase in cyst volume correlates with decline in renal function.37 Liver cysts occur in up to 67% and increase in size and number with age. Women suffer more severe polycystic liver disease than men.38
Seminal vesicle cysts occur in 40% of men, and rarely cysts may occur in the pancreas, spleen, and ovary.39
Fig. 8.9 a Autosomal recessive polycystic kidneys diagnosed in utero. Both kidneys are symmetrically enlarged with smooth surfaces and a bright texture. A hypoechoic rim (arrows) has developed around each kidney. The lack of amniotic fluid shows the kidneys are not functioning. b Autopsy of the newborn child. The baby died at birth due to lack of lung development as a consequence of the lack of amniotic fluid. The kidneys are shown to fill the abdomen and to have a smooth outline with no macroscopic cysts
Fig. 8.10 a Longitudinal image through the right kidney in a patient with ADPKD. b CT image of ADPKD, demonstrating numerous cysts throughout both kidneys with disruption of the normal renal architecture. c One of the cysts in this autosomal dominant polycystic kidney shows a fluid–debris level. The clinical history and outcome were of hemorrhage into the cyst rather than infection
Fig. 8.11 Autopsy specimen from a fetus affected with bilateral multicystic dysplastic kidneys. There are cysts of different sizes distorting the renal outline. Note how this differs from the image of autosomal recessive polycystic kidneys shown in Fig. 8.9b
Fig. 8.12 Patient with tuberous sclerosis where the kidneys are affected by innumerable angiomyolipomata
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree