Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
Abstract
Functional lesions of the ovary are by far the most common abnormalities encountered in the pathology of the ovary.
7.1 Introduction
Functional lesions of the ovary are by far the most common abnormalities encountered in the pathology of the ovary.
These lesions mainly involve the follicle (essentially during the reproductive age), less frequently the stroma cells (essentially after menopause), both as in the PCOD (in young women), or more rarely the Leydig cells (reproductive age group or menopause). During pregnancy, while the corpus luteum cyst is the most common functional lesion, very uncommon multifollicular ovaries (hyperreactio luteinalis) or solid nodules likely arising from stromal cells (pregnancy luteoma) can develop.
In clinical practice, these abnormalities can in many situations mimic tumoral lesions, mainly benign. Misinterpretation of their diagnosis can lead to unnecessary surgery and even more to inappropriate resections particularly in young women, which compromise the fertility, may be complicated with adhesions, or can lead to early menopause.
7.2 Functional Lesions in Nonpregnant Women During the Reproductive Age Group
There are a wide range of functional lesions in this age group. They vary from the single simple cyst to the more complex polycystic ovarian syndrome. For practical purposes, we divided this section in macrofollicular lesions (≥10 mm) and microfollicular lesions (<10 mm). Uncommon lesions involve the stroma.
Macrofollicular Lesions
These lesions result from excessive growth of one or several follicles with or without transformation in corpus luteum.
The most common and well defined is the unique follicle which can be non-luteinized (follicle cyst) or luteinized (corpus luteum cyst). The latter usually appears after rupture of the follicle but also has been described in some rare examples of luteinized unruptured follicle syndrome (LUF syndrome). These cysts may be complicated by hemorrhage.
Besides the common unilocular form, more complex patterns may be encountered in ultrasound representing bilocular or adjacent cysts.
Further more, multiple cysts superior to 10 mm in one or both ovaries led to the definition of the macrofollicular ovaries that could be divided in several sub-entities.
Microfollicular Lesions
They are dominated by the polycystic ovarian syndrome (PCOS) but can be encountered in women with no clinical or hormonal disturbance.
7.2.1 Follicle and Corpus Luteum Solitary Cysts
Definition
Follicle and corpus luteum are, respectively, termed follicle cyst and corpus luteum cyst when >3 cm [1].
Microscopically, follicle cysts are lined by an inner layer of granulosa cells and an outer layer of theca interna cells. The cells in either layer may be luteinized. Vascularization is weak and limited to the theca layer.
Corpus luteum cysts exhibit a convoluted lining composed of large luteinized granulosa cells and smaller luteinized theca interna cells with prominent outermost layer of connective tissue. Its wall is thicker. Vascularization is prominent at the periphery, essentially in the theca layer [1].
Content of follicle cysts and corpus luteum cysts varies from a serous or serosanguineous fluid to clotted blood, their hemorrhagic forms [1].
7.2.1.1 Non-Hemorrhagic Follicle Cysts
Common macroscopic and radiologic findings are summarized in Table 7.1 [1].
Table 7.1
Common macroscopic and radiologic findings of non-hemorrhagic follicle cysts
Size: between 3 and 8 cm |
Round |
Unilateral |
Thin wall |
Serous content |
Unique |
Unilocular |
Absence of papillary projection |
Ultrasound
The Cyst
Typically these cysts are unilocular, anechoic with a thin or non-visualized wall and without any papillary projection (Fig. 7.1). They usually measure from 3 to 8 cm in diameter. Larger cysts may occur rarely [1].
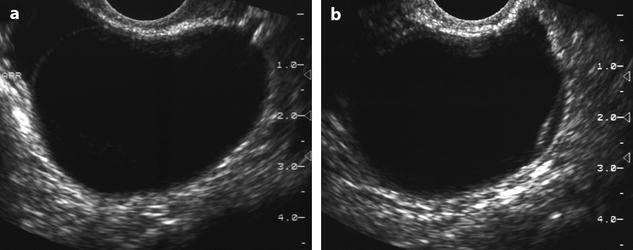
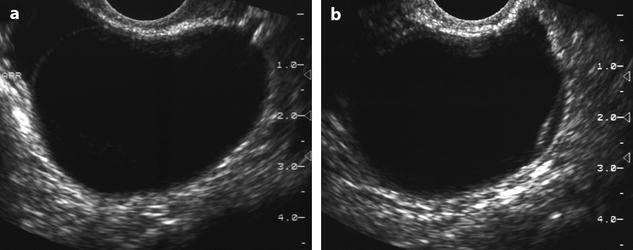
Fig. 7.1
Functional cyst with clear fluid. A 43-year-old women with left pelvic pain. (a) Endovaginal US displays a right unilocular anechoic cyst measuring 4.5 cm with a thin regular wall. An adjacent follicle is seen at the periphery. (b) Another view depicts an echogenic line near the inner wall of the cyst very likely related to a detachment of the granulosa. Coelioscopy with cystectomy was performed. Pathology revealed a functional follicular cyst
By definition a follicle cyst is >3 cm; otherwise, it is called follicle [1]. However, a follicle less than 3 cm that persists over one or more cycles can be assimilated to a small follicle cyst, but the denomination of persistent macrofollicle is more appropriate.
Its intraovarian location can be definitely diagnosed when the mass is encased in the ovarian parenchyma and/or surrounded by follicles which are pushed toward the periphery of the cyst.
In corpus luteum cyst, the wall is thicker. In color Doppler, vascularization in the wall is usually demonstrated.
Differential Diagnosis on US
The solitary follicle cyst should be distinguished from other purely ovarian and extraovarian cystic masses (Table 7.2).
Table 7.2
Differential diagnosis of purely unilocular ovarian cystic masses on US, MR, and/or CT
Epithelial ovarian tumors |
1. Serous cystadenoma |
2. Mucinous cystadenoma (occasional) |
Extraovarian unilocular cystic masses |
1. Hydrosalpinx |
2. Paraovarian cyst |
3. Peritoneal pseudocyst |
4. Uncommon: meningocele, bladder diverticulum |
Ovarian non-epithelial unilocular cystic masses |
Exceptional |
1. Mature cystic teratoma (pediatric age) |
2. Granulosa cell tumor (juvenile and adult type) |
When the ovarian origin is definite, the cyst cannot be differentiated from other purely cystic ovarian masses (Table 7.2) (Figs. 7.1, 7.2, 7.3, and 7.4). Follow-up is necessary to make the differential diagnosis.

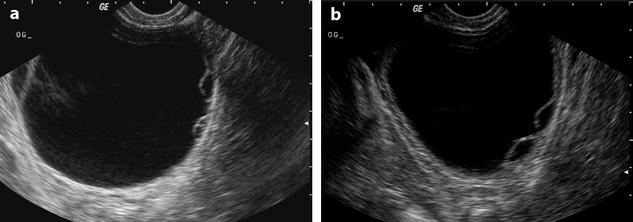
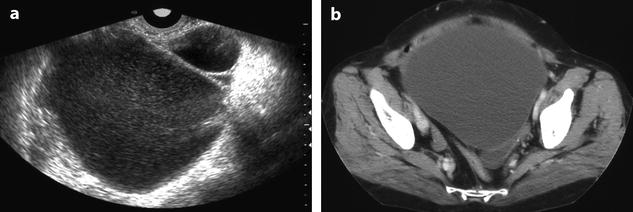

Fig. 7.2
Unilocular serous cystadenoma without papillary projection. Ultrasound shows an anechoic cyst without any papillary projection indistinguishable from a functional cyst. Only persistence on follow-up allowed suspicion of a neoplastic lesion. Histology confirmed the diagnosis of a serous cystadenoma
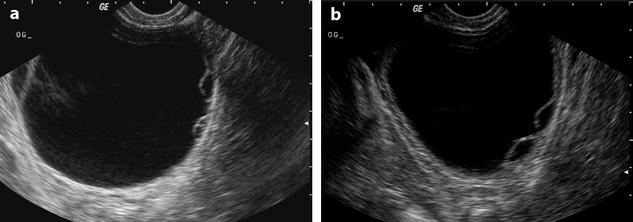
Fig. 7.3
Mucinous cystadenoma in a 40-year-old woman. (a) Transvaginal ultrasound shows a 7.4-cm cyst with anechoic fluid and thin wall. On the left, there is a loculation or an adjacent follicle. On the right, small loculations can be misinterpreted as granulosa detachments (compare to Fig. 7.1). (b) Another view of the left loculations. Follow-up showed persistence of the cyst. Coelioscopy and cystectomy were performed. Pathology: mucinous cystadenoma
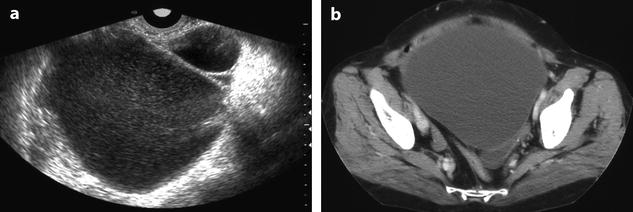
Fig. 7.4
Unilocular mucinous cystadenoma. (a) Ultrasound discloses a hypoechoic cyst adjacent to a smaller follicle. Differentiation from a functional hemorrhagic cyst or an endometrioma is not possible. (b) CT better demonstrates the large size of the cyst and absence of septa or papillary projections. Surgery confirmed the diagnosis of mucinous cystadenoma
When the ovarian origin is not sure, extraovarian unilocular cystic masses must be discussed:
1.
Hydrosalpinx is the most common differential diagnosis. In the typical form of hydrosalpinx, tubular shape, plicae, mucosal folds when present allow to make the differential (Fig. 7.5). However, in some cases, only the ampullary portion of the salpinx may be dilated and simulates a unilocular cyst.
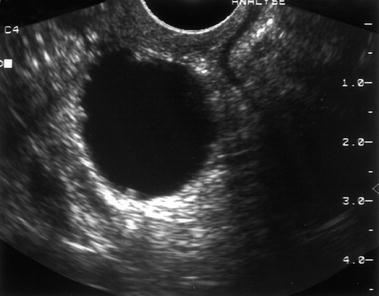
Fig. 7.5
Small hydrosalpinx with mucosal folds. Transvaginal sonography displays a small unilocular 2.5-cm cystic lesion with small intraluminal projections very suggestive of mucosal folds in a hydrosalpinx. Coelioscopy and pathology confirmed the diagnosis of hydrosalpinx
2.
A paraovarian cyst can only be distinguished when it is clearly separated from the ipsilateral normal ovary (Fig. 7.6).
Fig. 7.6
Large paraovarian cyst laminating a normal left ovary. Axial T2W MR image discloses a large paraovarian cyst coming in close contact with the left ovary and laminating it. Distinction from an ovarian cyst is not possible, although one should expect the ovary to be more laminated with such a large cyst. Functional cyst can be as large as this one, although this is infrequent. Coelioscopy and pathology confirmed a left paraovarian simple cyst
3.
Peritoneal pseudocyst is rarely unilocular. Previous surgery or PID is usually suggestive.
4.
When the location is posterior in the pelvis, a meningocele must always be kept in mind.
Whatever the type of mass, purely cystic masses on US are almost always benign. Most cases of follicle cyst and corpus luteum cysts regress spontaneously within 2 months, and this process can be accelerated by administration of a combined estrogen-progestogen preparation.
MR and CT
Occasionally follicle cyst can be visualized on MR or CT.
On MR, performed without contrast, their signal is close to urine on T1- and T2-weighted images (Fig. 7.7). The wall is usually not visible on T1 where its signal is usually isointense relative to ovarian stroma, but usually visible on T2 where its signal is hypointense relative to ovarian stroma; after contrast, the wall shows in most cases greater enhancement than ovarian stroma [2].
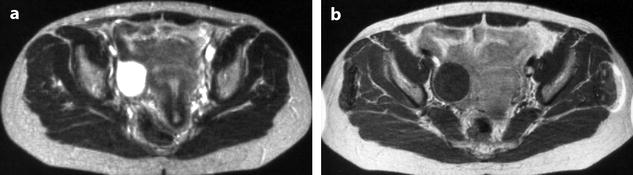
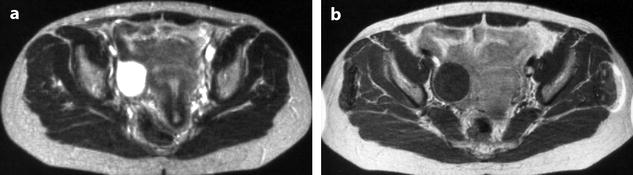
Fig. 7.7
Functional cyst with clear fluid. (a) MR, axial view, T2-weighted image. The content of the cyst has signal intensity close to urine. (b) MR, axial view, T1-weighted image with contrast injection. Regular cyst with a low signal intensity close to urine is displayed in the right ovary laminating the normal parenchyma
On CT, their density is close to water density. After contrast injection, enhancement of the laminated normal ovarian parenchyma can be seen.
7.2.1.2 Follicle Hemorrhagic Cysts (FHC)
Macroscopic and Radiologic Findings
They are summarized in Table 7.3.
Table 7.3
Macroscopic and radiologic findings of hemorrhagic follicle cysts
Common |
Size: 5–6 cm |
Unilocular |
Round |
Unilateral |
Unique |
Thick wall |
Uncommon |
Bilateral |
Multiple in the same ovary |
Ultrasound
Cystic Content
Blood is known to have a variable sonographic appearance mostly related to the temporal sequence of clot formation and lysis. Classically fresh blood is anechoic, progressing subacutely to a mixed echogenicity and finally becoming anechoic. Therefore, it is not surprising that FHC have such variable features (Fig. 7.8).
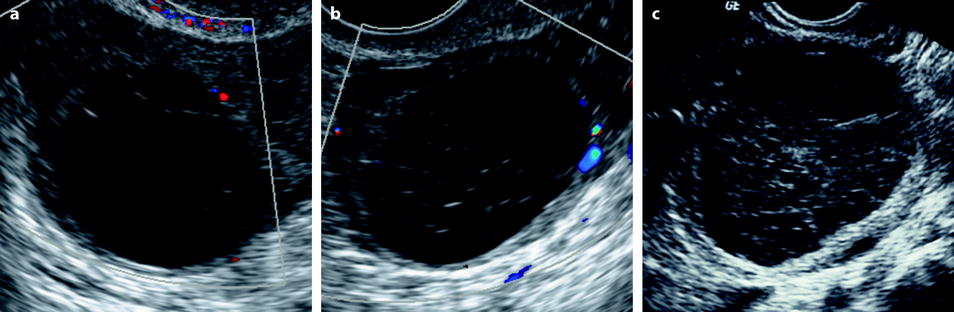
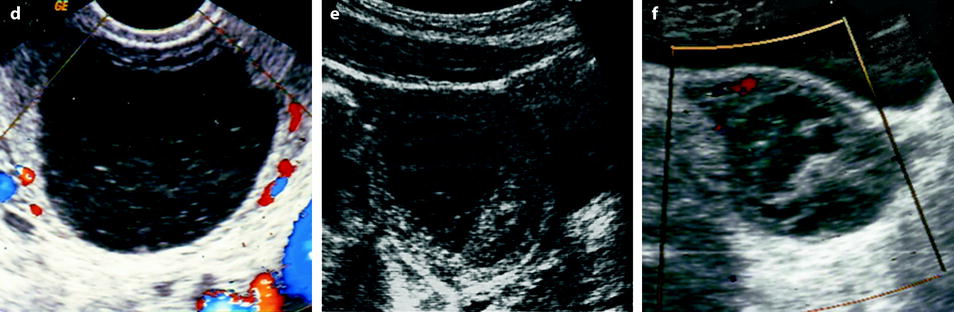
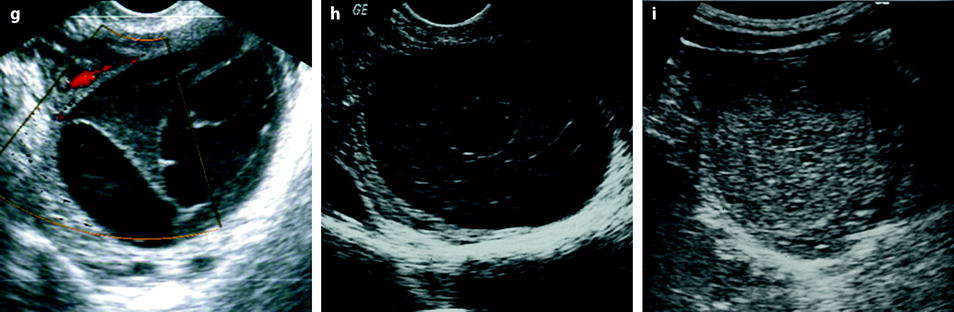
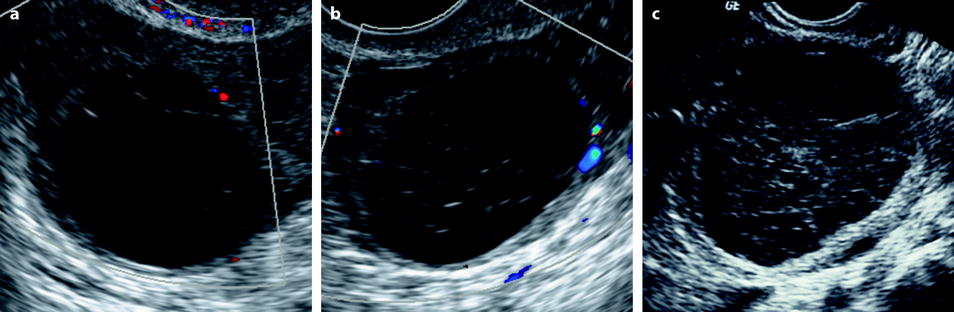
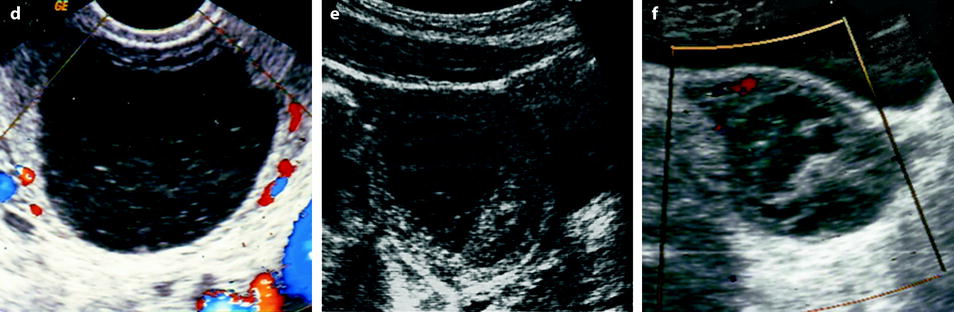
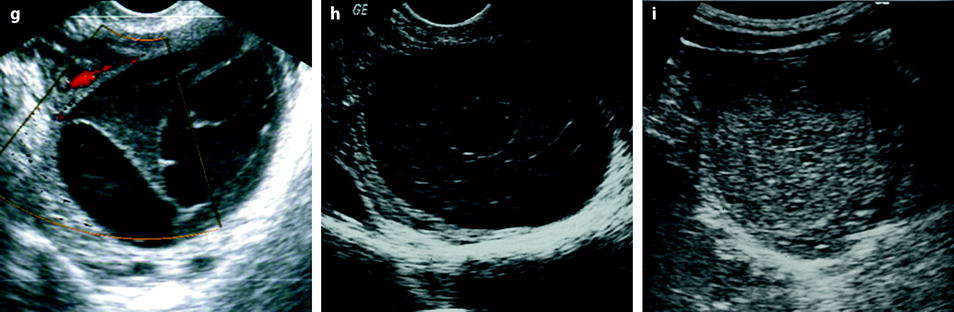
Fig. 7.8
Some but not all patterns of FHC: (a) scarce fibrin strands at the limit of visibility, (b) classical fine fishnet appearance, (c) coarse fishnet appearance looking like a sponge, (d) ill-defined fluid-debris level, (e) eccentric clot with associated slightly perceptible fishnet or reticular pattern, (f) irregular retractile clot, (g) stellate well-demarcated clot, (h) anechoic area inside diffuse echogenic content, (i) hyperechoic relatively homogeneous pattern. Although not always shown here, color or power Doppler was always performed to exclude vascularization inside the echoic content of the cysts. In all cases, follow-up or surgery confirmed the diagnosis
Some typical patterns are very suggestive of FHC [3–6]:
1.
Diffuse echogenic pattern which seems to consist of a blood clot and often includes a small echo-free area (Figs. 7.8h and 7.9).
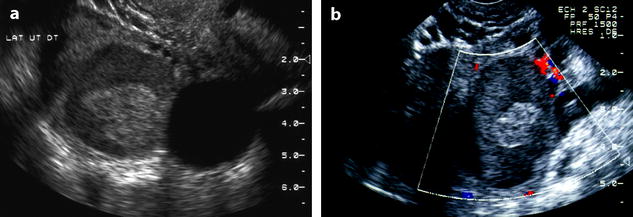
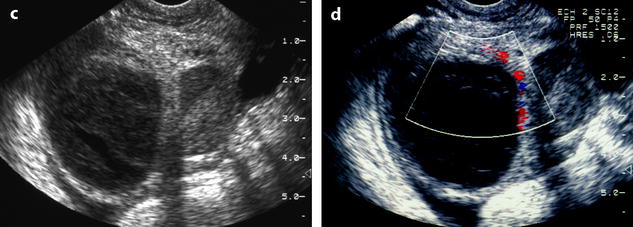
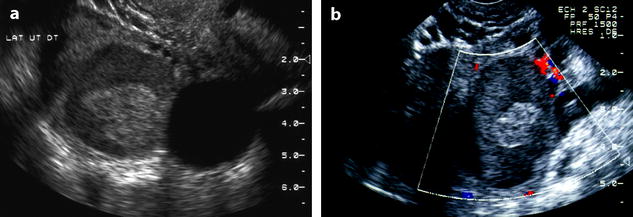
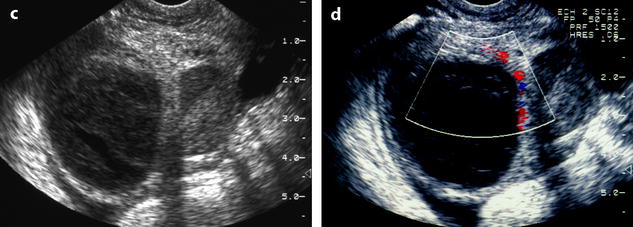
Fig. 7.9
Functional hemorrhagic cysts. Twenty-three-year-old woman with pelvic pain. (a) Endovaginal US shows in the right ovary a 3.5-cm echogenic mass with a central, more echogenic portion and an adjacent 2.8-cm anechoic follicle. (b) Endovaginal US with color Doppler demonstrates absence of vessel in the echogenic mass, making the diagnosis of an echogenic cyst. (c, d) Endovaginal US performed 10 days later. The echogenicity of the larger mass has significantly changed. An echo-free area is visualized in an otherwise relatively homogeneous echogenic mass. Modification of the echogenicity in a short interval and the new pattern of the mass are both characteristic of FHC. On the other hand, an echogenic material probably related to hemorrhage is now present in the previously anechoic follicle
2.
Whirled pattern of clotted blood or a mixed pattern with a clearly demarcated echogenic part (Fig. 7.10).
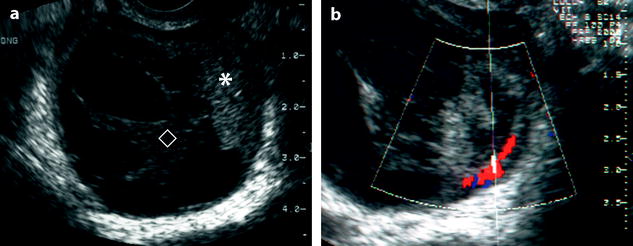
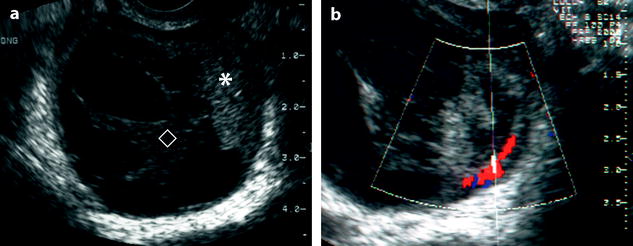
Fig. 7.10
FHC with different intracystic patterns. (a) FHC with eccentric hyperechoic clot (asterisk), echoic central clot (lozenge) with digitations surrounding slightly echoic areas. (b) Doppler showed flow only in the wall. Follow-up confirmed disappearance of the cyst
3.
Multiple fine interdigitating “septations” giving a fishnet appearance (Fig. 7.11). These echogenic lines correspond to fibrin or other products of blood.
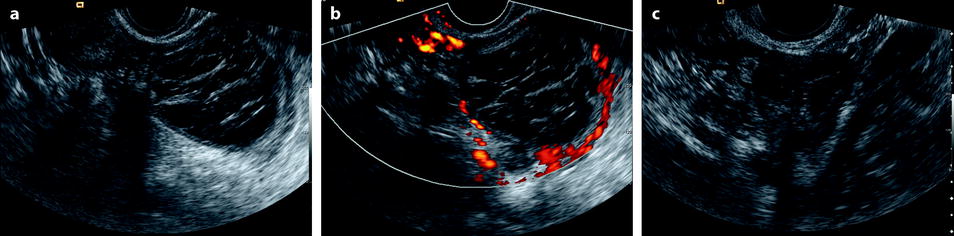
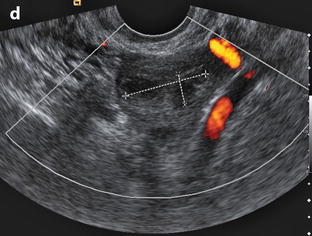
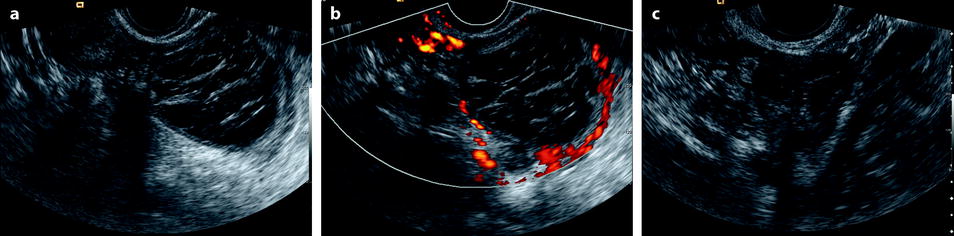
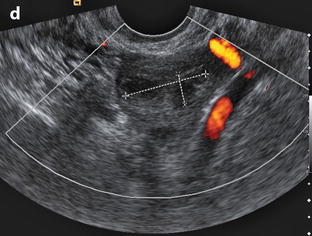
Fig. 7.11
FHC with a coarse fishnet appearance and follow-up. (a, b) endovaginal ultrasound in a 39-year-old woman with left pelvic pain in the second part of her menstrual cycle demonstrated a 5-cm left ovarian cyst with a coarse fishnet appearance and peripheral marked venous and arterial vasculature suggesting an hemorrhagic corpus luteum cyst. (c, d) follow-up endovaginal ultrasound, 15 days later, at day 8 of her menstrual cycle, shows marked shrinking of the cyst that measures only 25 × 10 mm still containing echoic structures with no color Doppler. A third ultrasound 3 months later showed complete disappearance of the cyst
4.
In other cases, some echogenic patterns are more heterogeneous, but containing in at least an area of the cyst one of the patterns described above (Fig. 7.12).
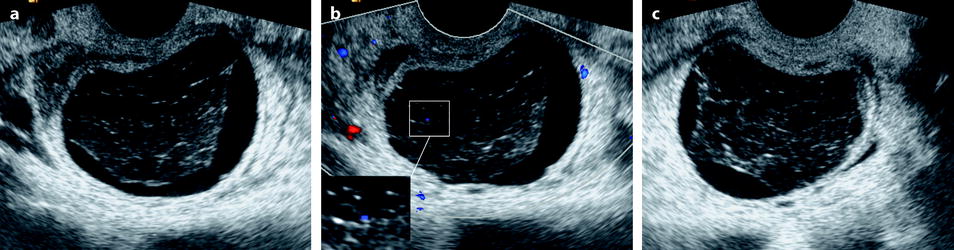
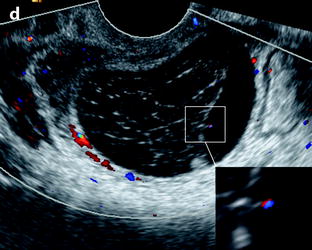
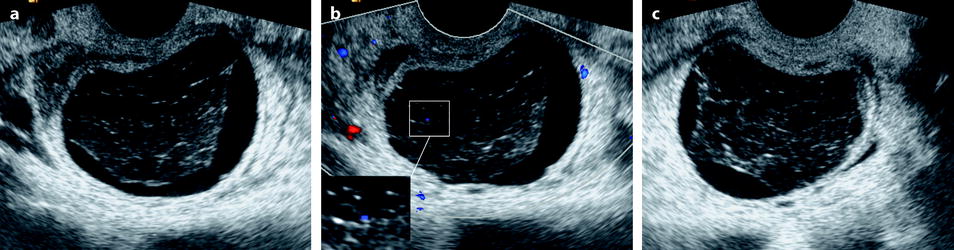
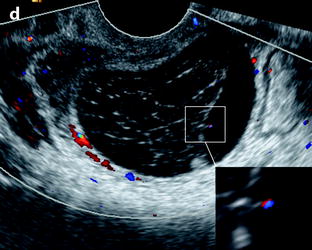
Fig. 7.12
FHC with central clot, reticular pattern, and Doppler artifacts. Transvaginal US in a 46-year-old woman discloses a cyst with a large central clot surrounded by slightly echoic liquid (a–c). On some views (c), the clot seems anchored to the inner wall of the cyst like a spider web. A reticular pattern is also present (d). Doppler artifacts (inset in b and d) must not be mistaken with true vascular flow. Follow-up confirmed complete disappearance of the cyst
Some other patterns are not as characteristic:
1.
Layering is uncommon. It is not specific [7, 8] (Fig. 7.13); this level can be seen in endometrioma and in dermoid cyst.
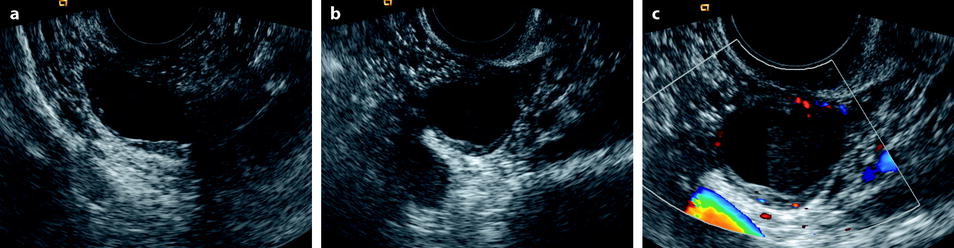
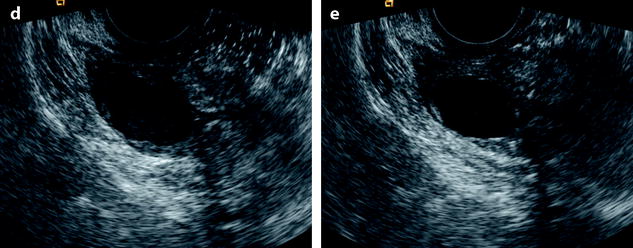
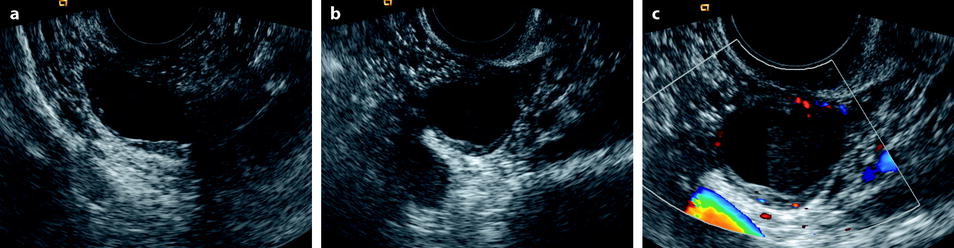
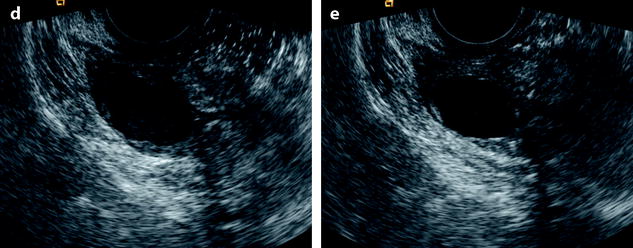
Fig. 7.13
Corpus luteum with hemorrhagic cystic content and fluid level. (a) Oblique transvaginal US view in a woman in the second part of her cycle discloses a right ovarian 2.5 × 1.5-cm cystic structure with mixed echoic and anechoic content. (b) Strict sagittal view demonstrates the presence of a sharp fluid level. (c) Color Doppler shows vascular peripheral rim highly suggesting a cystic hemorrhagic corpus luteum. (d) Coronal view through the dependent part shows only echoic content. (e) Coronal view through the nondependent part shows only anechoic content. Follow-up confirmed disappearance of the cyst
2.
The pattern can be diffusely echogenic and heterogeneous (Fig. 7.14).

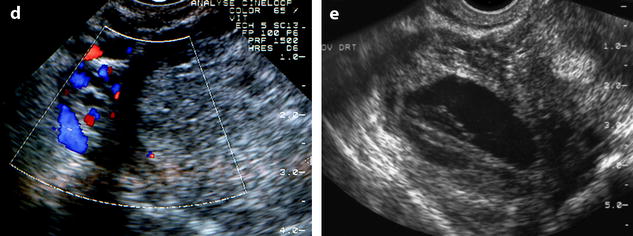

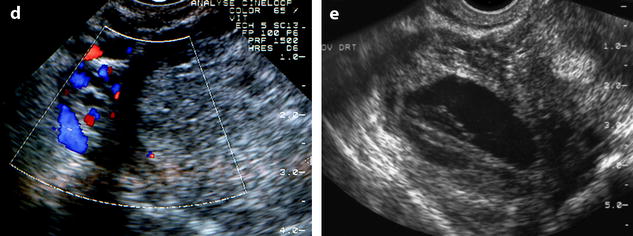
Fig. 7.14
FHC with atypical intracystic patterns. (a) FHC with heterogeneous intracystic pattern that can simulate a dermoid cyst. Note the linear echoic strands mimicking hair in dermoid cyst (arrow). (b) Homogeneously diffuse echoic pattern with slight more echoic eccentric area (black arrow), a combination that can simulate endometrioma. (c, d) Diffuse slightly hyperechoic and slightly heterogeneous avascular pattern that can suggest either endometrioma or dermoid cyst. (e) Fibrin digitations that can be confused with true septae in a multilocular cyst but avascular on Doppler
3.
The cyst can be completely anechoic (with hemorrhage in the wall).
Wall
A thickened wall of 2–3 mm is usually present.
Acoustic enhancement is common.
Normal Ovarian Parenchyma
A normal ovarian parenchyma pushed toward the periphery is frequently observed.
Doppler
The main interest of color Doppler particularly when the form is not characteristic is to demonstrate the absence of vessel in the mass, which highly suggests its cystic nature [9]. Regular vessels can be visualized in the wall of the cyst.
Bilaterality and Multiplicity
Bilaterality and multiplicity in the same ovary are very uncommon.
Ultrasound findings of FHC are summarized in Table 7.4, and as endometrioma can have a close presentation, findings of endometriomas are reported in the same table.
Table 7.4
Ultrasound findings of endometriomas and functional hemorrhagic cysts
Endometrioma | Functional hemorrhagic cyst | |
|---|---|---|
Size | <8 cm | <8 cm |
Shape | Not round with protrusion | Round |
Bilateral | 1/2 to 1/3 of cases | Exceptional |
Multiple cysts in the same ovary | Possible | Exceptional |
Location | Ovarian fossa | Ovarian fossa |
Displaced inward and backward | ||
Internal echo pattern | Ground glass pattern | Fishnet pattern |
Whirled pattern | ||
Heterogenous pattern | ||
Clots | Echogenic foci | Large hyperechoic central portion |
Peripheral | ||
Round or curvilinear | ||
Wall | Thick | Thick |
Layering | Possible | Possible |
Acoustic enhancement | Very common | Very common |
Follow-up ultrasound | No modification in size and echo pattern | Modification in size and echo pattern |
Normal parenchyma pushed toward the periphery | Common finding | Common finding |
Adhesions | Possible | Absence |
Differential
The main differential diagnoses are listed in Table 7.5.
Table 7.5
Differential diagnosis of FHC
(a) Endometriosis |
(b) Other cystic echogenic masses |
Mature cystic teratoma |
Tubo-ovarian abscess |
Cystic epithelial tumor complicated with hemorrhage |
(c) Tissular echogenic masses |
Echogenic epithelial tumor with endocystic vegetation |
Ovarian fibroma |
2.
Cystic mature teratoma typically has different morphological characteristics. However, in some cases, the echogenic pattern does not allow to make the differential so that MR or CT is necessary to make a specific diagnosis (Fig. 7.14).
3.
More uncommonly, solid echogenic masses must be differentiated. Indeed, in some cases, vascularization can be difficult or impossible to demonstrate in a tissular mass as an ovarian fibroma or in a small vegetation resembling a clot in a cystic epithelial tumor (Fig. 7.15).
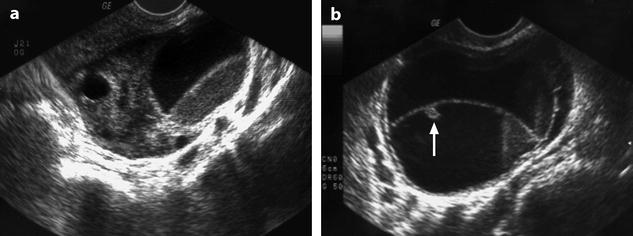
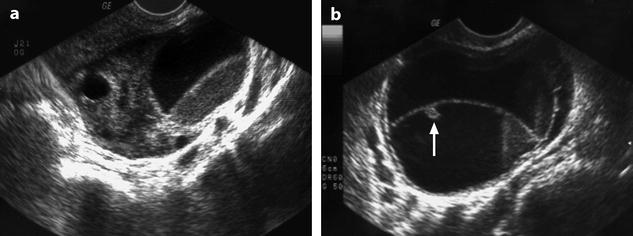
Fig. 7.15
Pseudovegetation in an FHC. Multiple hemorrhagic functional cysts in a 33-year-old woman under Clomid for ovarian stimulation: (a) Endovaginal oblique view shows a partly anechoic and partly echoic cyst. (b) Strict endovaginal sagittal view is necessary to well disclose the levels in the cysts. The small echoic structure against the wall of one of the cysts (arrow) is not vegetation but a small clot. All lesions disappeared on follow-up ultrasound
Resolution on follow-up ultrasound is a key finding for the diagnosis.
In all cases and particularly when the pattern of the cyst is not characteristic, two findings displayed on follow-up are characteristic for FHC [5] (Figs. 7.9 and 7.14):
Decrease in size or even complete disappearance of the cyst usually after the next period
Changing of the ultrasound pattern is depicted within 10 days
Association: FHC can be associated in the same ovary with one or more endometriomas.
Rupture (see Chap. 32)
MR [29]
Most commonly, the content of the cyst in FHC is hypointense on T1 (without and with fat suppression) contrary to endometrioma (Fig. 7.16). On T2 it is homogeneous or often heterogenous (Fig. 7.17).
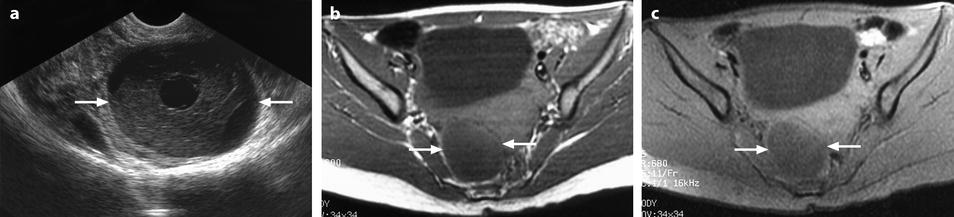
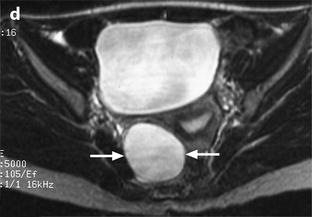
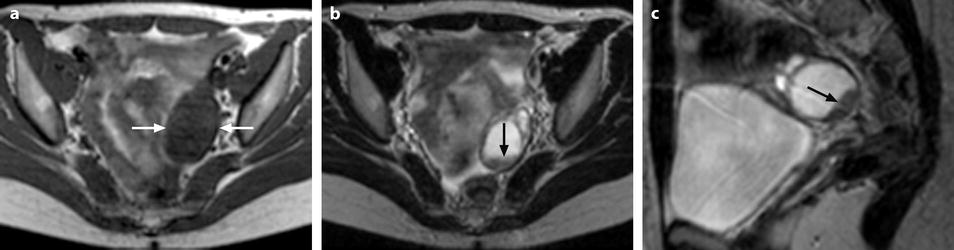
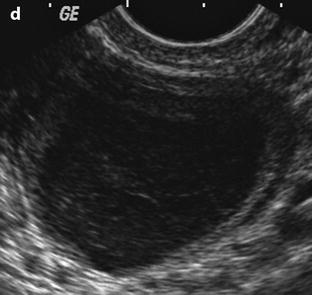
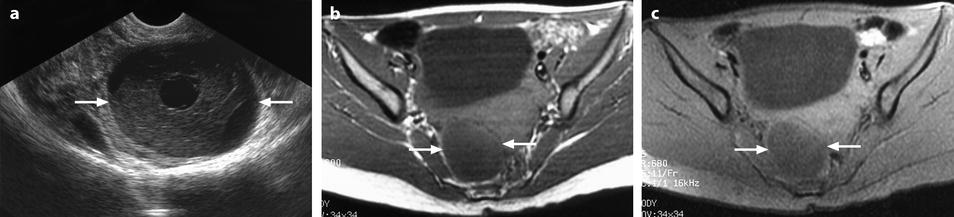
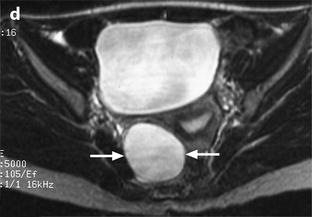
Fig. 7.16
FHC with a typical pattern on US and comparable to a simple cyst on MR. (a) Transvaginal US in a 26-year-old woman with pelvic pain in the second part of her menstrual cycle shows a 5.5-cm right ovarian cyst (arrows) with a typical pattern of FHC. (b–d) MR examination performed after 1.5 h demonstrates a homogeneous cyst (arrows), hypointense (i.e., with a signal intensity less than or equal to that of muscle) on T1-weighted images without (b) and with fat suppression (c); on T2-weighted images (d), the overall signal of the cyst was hyperintense, i.e., comparable to that of urine. A follow-up US examination after 12 days showed the disappearance of the cyst (Figures from Author’s personal publication: Kanso et al. [29])
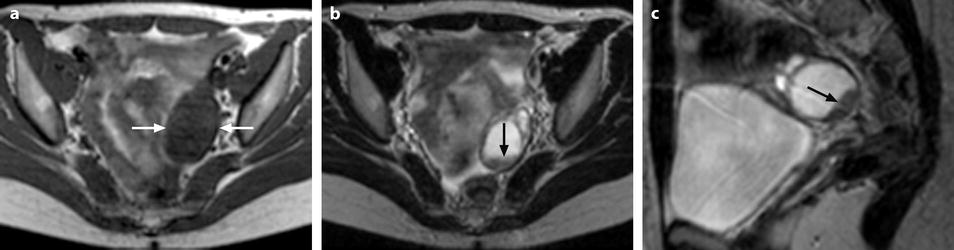
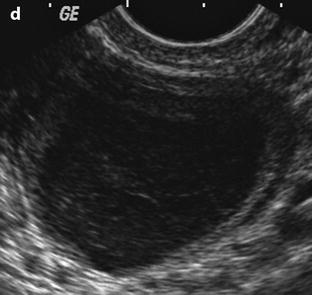
Fig. 7.17
FHC hypointense on T1 and heterogeneous on T2. A 25-year-old woman with a 3.4-cm left ovarian FHC and a 3.5-cm dermoid cyst of the right ovary (not shown on these images). (a) Axial T1-weighted image shows a homogeneous hypointense left adnexal cyst (arrows) that was also hypointense after fat suppression (not shown). (b, c) T2-weighted images show a heterogeneous cyst with a pseudo-horizontal level in the axial plane (arrow in b), but in the sagittal plane, this interface appears oblique (arrow in c). (d) Ultrasound performed the same day before MRI showed the left ovarian cyst to have a typical fishnet appearance. Laparoscopy confirmed the presence of a right dermoid cyst and left FHC (Figures from Author’s personal publication: Kanso et al. [29])
Uncommonly, the cyst can have intermediate signal intensity on T1 that increases after fat suppression with heterogeneous signal on T2 (Fig. 7.18).
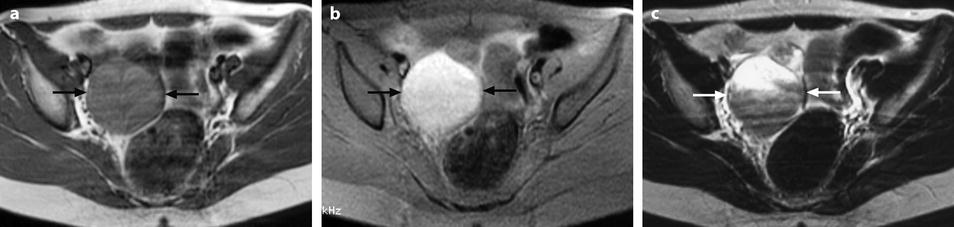

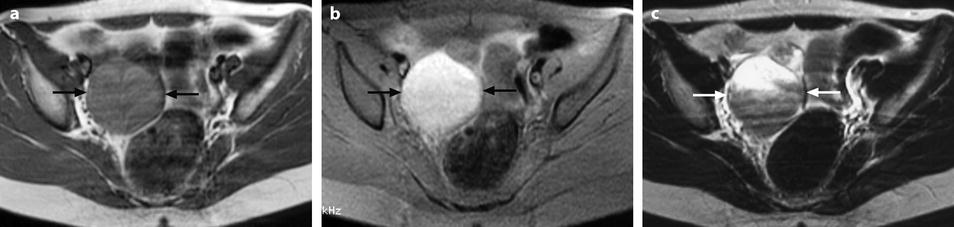

Fig. 7.18
FHC with intermediate signal intensity on T1 and high signal intensity on T1-weighted images with fat suppression. Axial MR images of a 6-cm surgically proven right FHC in a 16-year-old patient. (a) T1-weighted image shows a cyst (arrows) of intermediate signal intensity, slightly higher than that of muscle. (b) On T1-weighted image with fat suppression, the cyst (arrows) is relatively homogeneous and appears hyperintense. (c) T2-weighted image shows a heterogeneous cyst (arrows) with hyperintense and hypointense areas. (d) Ultrasound performed within 24 h shows an echoic pattern with some anechoic small areas (Figures from Author’s personal publication: Kanso et al. [29])
Partial hyperintensity can be seen on T1 fat suppression (Fig. 7.19).


Fig. 7.19
FHC partially hyperintense on T1-weighted images. A 51-year-old patient with a 5.3-cm left FHC discovered incidentally on a pelvic MR performed for uterine adenomyosis. (a, b) T1-weighted image (a) shows a cyst (arrows) that is mainly hypointense, with small peripheral hyperintense components more evident after fat suppression (b). (c) On T2-weighted image, the cyst (arrows) appears very heterogeneous. The cyst disappeared spontaneously on follow-up examination (Figures from Author’s personal publication: Kanso et al. [29])
Exceptionally it can looks like an endometrioma (Fig. 7.20).
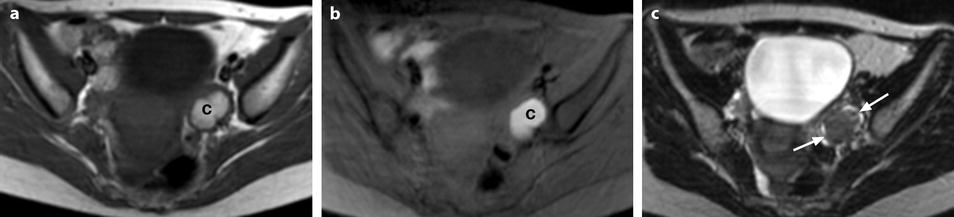

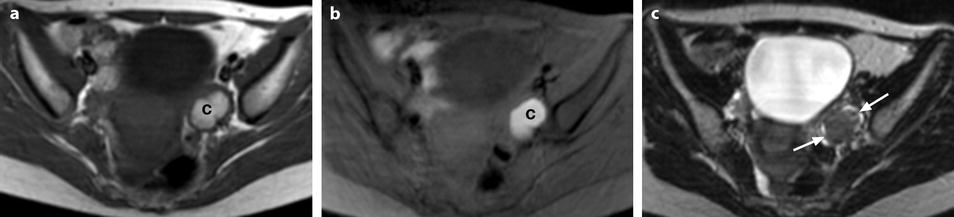

Fig. 7.20
FHC mimicking endometrioma. Axial MR images in a 26-year-old patient with a known left ovarian cyst persistent since 6 months. (a, b) T1-weighted images without (a) and with fat suppression (b) show an almost entirely hyperintense 3.2-cm left ovarian cyst (letter c) with internal notches. (c) On T2-weighted image, the cyst (arrows) exhibits low signal intensity. (d) Concomitant US shows a cyst (arrows) with echoic and hyperechoic content suggesting endometriosis. The MR and US imaging diagnosis was, incorrectly, an endometrial cyst. The patient, having refused any surgical or medical treatment, had an US examination 6 months later showing a decrease of the cyst size to 8 mm and its complete disappearance after another 6 months, hence confirming its functional nature (Figures from Author’s personal publication: Kanso et al. [29])
MR findings are summarized in Table 7.6.
Table 7.6
Signal intensity of FHC and endometriomas on MR
T1 | T1-FS | T2 | FHC | Endometrioma |
|---|---|---|---|---|
Low | Low | High (homogenous or heterogenous) | Most common | – |
Low | – | Rare | ||
Intermediate | High | High (homogenous or heterogenous) | Uncommon | Uncommon |
Low | – | Uncommon | ||
High | High | <Adipose tissue (homogenous or heterogenous) | Exceptional | Most common |