Gynecologic, Obstetric, and Scrotal Emergencies
Robert D. Harris
Roberta diFlorio Alexander
John H. Harris Jr.
Gynecologic, obstetric, and scrotal emergencies are among the most common urgent situations involving children or young adults: They frequently present with acute pain in otherwise healthy, young patients; they may be extremely anxiety producing to both the patient and clinician (because of the uncertainty of the diagnosis and the acuteness/severity of the medical condition); and they are often diagnosed with imaging, usually ultrasound (US). This is especially relevant due to recent concerns over the public health problem of medically related excessive radiation exposure that is occurring largely due to the increase in body and head computed tomography (CT) performed in emergency departments, placing the public at increased risk for developing cancer in 20 to 30 years in the future.
GENERAL CONSIDERATIONS
Gynecologic and obstetrical emergencies are two of the most common problems often encountered in teenage or premenopausal women presenting to the emergency ward or radiology department. In general terms, gynecologic emergencies usually present as a manifestation of pelvic pain and obstetrical emergencies, as vaginal bleeding in pregnancy.
The most frequently used imaging modality for obstetrical and gynecologic emergencies is pelvic US for four reasons: (1) it is widely available; (2) it is the most efficacious technique for visualizing the ovaries, uterus, fetus, and placenta; (3) it does so without adding to the burden of harmful ionizing radiation that accrues due to other imaging techniques; and (4) it can be obtained in real time in a short acquisition period. Conventional radiographs and CT, both of which use ionizing radiation to produce an image, have a more limited role, as the soft tissues of the pelvis are poorly delineated by the former technique, and limited contrast and spatial resolution of pelvic organs is a disadvantage in the latter modality. Magnetic resonance imaging (MRI) offers improved global anatomic visualization and contrast resolution compared with US, employs nonionizing radiation and is a problem-solving technique in some obstetrical and gynecologic emergencies. However, its cost, claustrophobic-associated limitations, longer duration of scanning, and limited availability preclude universal acceptance.
Conventional abdominal radiography is frequently the first-line imaging examination in the nonpregnant female patient with abdominal or pelvic pain. It may show dilated bowel loops or air-fluid levels in a patient with small bowel obstruction from pelvic adhesions, an appendicolith in acute appendicitis, or a radiopaque ureteral calculus in a patient with flank and pelvic discomfort. Other common causes for radiodensities or metallic foci are uterine/ovarian calcifications, pelvic phleboliths (calcified veins), fallopian tube clips from prior sterilization, and surgical clips from endoscopic surgery or herniorrhaphy. If additional diagnostic imaging is necessary, most patients will proceed to US (or, in some cases, CT) for further
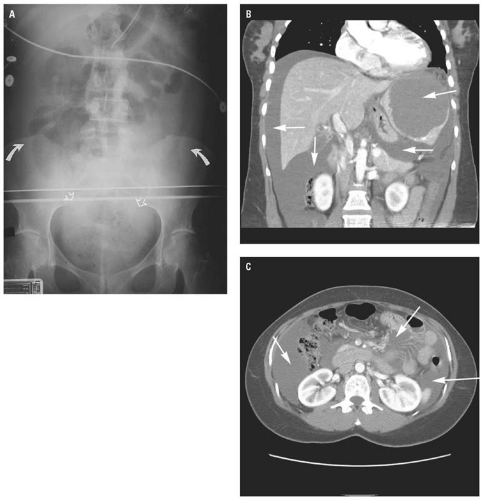
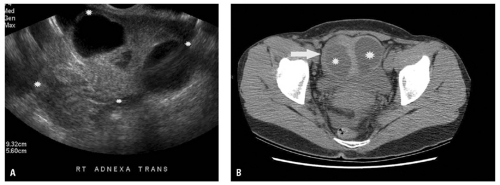
diagnosis. Conventional radiographs or CT may reveal hemoperitoneum in patients with a ruptured ectopic pregnancy or hemorrhagic ovarian cyst (Fig. 16.1).
diagnosis. Conventional radiographs or CT may reveal hemoperitoneum in patients with a ruptured ectopic pregnancy or hemorrhagic ovarian cyst (Fig. 16.1).
The indications for conventional radiography in a pregnant patient are much more restrictive due to the risks of exposing the fetus to ionizing radiation. Suspected renal colic (flank pain, hematuria, fever) or suspected bowel obstruction are the primary indications for a conventional radiograph, using shielding of nonimaged body parts and as low-dose radiation exposure as possible, in a gravid patient. First trimester radiography is to be avoided, if at all possible, due to the extreme sensitivity of the early fetus or embryo.
The conventional teaching in radiology is that most urinary stones are radiopaque, but the actual figure varies and depends on the size of the stone and the radiographic technique as well. Obstetrical patients present special challenges. A third trimester fetus with a well-ossified skeleton may mask detection of upper tract calculi; also, there is the more common problem of differentiating pelvic phleboliths from distal ureteral calculi. Noncontrast helical CT, which has all but replaced intravenous urography in most medical
centers, has not been used widely in obstetrical patients due to the significant radiation exposure concerns.
centers, has not been used widely in obstetrical patients due to the significant radiation exposure concerns.
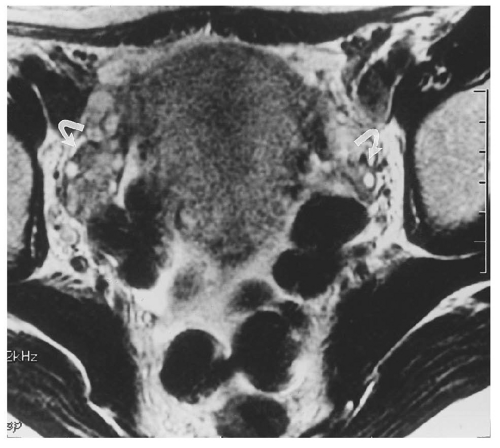
CT is generally not performed in obstetrical patients, unless there is an indication for pelvimetry. This pelvimetry technique has been well established without the use of any contrast material and requires only two or three images—low-dose images plus the scout localizer—similar to the frontal view of a routine radiograph. MRI has also been suggested as the modality for assessing cephalopelvic disproportion. Gynecologic patients may require CT for assessing complicated or extensive tuboovarian abscesses (TOAs) (Fig. 16.2). The imaging of cysts or ovarian masses too large to be completely visualized by US is usually by pelvic MRI with its excellent spatial and chemically based information. Most pelvic CT is obtained with oral contrast material (with the exception of the limited CT for appendicitis), but the need for intravenous contrast CT is less well established for true gynecologic and obstetrical emergencies. It is regarded as safe for the fetus; the only issue is maternal allergic reactions and renal function, as it is a well-documented nephrotoxic agent.
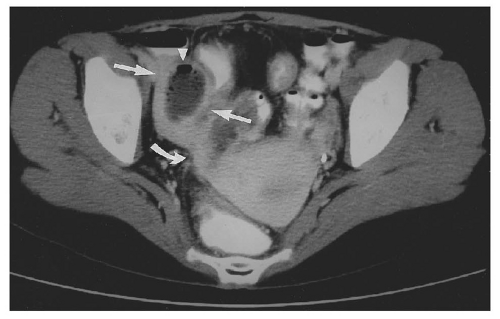
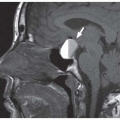
MRI has shown promise as an adjunctive imaging test in cases where US is equivocal or suboptimal, and there are extensive data supporting its use in fetal abnormalities, placenta previa or accreta, and evaluating ovarian cysts and masses. MRI has also been helpful in the diagnosis of uterine incarceration, rare but potentially grave situation, with trapping of a retroverted uterus between pubis and sacrum. This condition—frequently associated with severe maternal pain, premature labor, and uterine rupture—is often missed with prenatal US and may be subsequently diagnosed with MRI (Fig. 16.3). However, US remains the preeminent imaging modality for most obstetrical and gynecologic emergencies.
GYNECOLOGIC IMAGING: MODALITIES
Ultrasound
US is the diagnostic “workhorse” for problems of the female pelvis. Radiographs may demonstrate a ureteral calculus or an appendicolith (calcificied stool in the appendix), and CT is useful to image a pelvic abscess from pelvic inflammatory disease (PID), but US is the modality of choice in most situations.
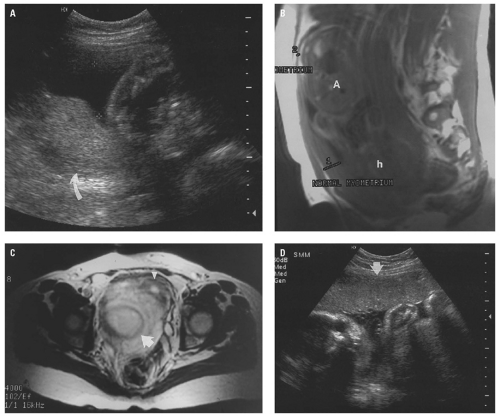
There are instances where conventional radiography may suggest the diagnosis, but in general, it only shows nonspecific signs. There may be a mass effect related to the bowel from a pelvic abscess in a patient with PID, but this may be difficult to differentiate from a distended bladder, abscess from other causes, or other soft tissue abnormality (i.e., tumor). Intrauterine contraceptive devices (IUDs) are generally radiopaque and well demonstrated with abdominal radiographs or CT. However, the usual clinical question of the exact location of the IUD (intrauterine vs. extrauterine) is difficult, if not impossible, to ascertain with conventional radiography (Fig. 16.4A) but is easily determined with CT or US. Rarely, IUDs may not be radiopaque, which presents difficulty in localization with conventional radiography. Mirena IUDs are not very radiopaque and can even be difficult to see on transvaginal (TV) pelvic US if they are not lined up precisely at the right geometry to the transducer (Fig. 16.4B,C).
Transabdominal US has been the traditional method to image the female pelvis and is still a useful first step in sonography. However, TVUS is state of the art in all centers because of better spatial and contrast resolution, and it is almost universally available on a 24-hour basis. Virtually, all emergent
pelvic sonograms require TV scanning. Translabial US, although occasionally useful when TV is contraindicated, is rarely used also. It may be useful in certain instances such as assessing placenta previa or if the patient is unable to tolerate a TV approach.
pelvic sonograms require TV scanning. Translabial US, although occasionally useful when TV is contraindicated, is rarely used also. It may be useful in certain instances such as assessing placenta previa or if the patient is unable to tolerate a TV approach.
At most medical centers, TV scanning is the technique of choice. This obviates the need for a full bladder, and the image resolution is much improved compared to transabdominal or translabial US. Of course, if a more global view of the pelvis is needed, then one can perform transabdominal (i.e., transvesical) US if there is significant urine in the bladder to serve as an acoustic window.
Transabdominal US can be performed with a general purpose 2 to 6 MHz transducer and can provide a field of view as large as 18 to 20 cm. A 5 to 8 MHz transducer will provide better spatial resolution but will not penetrate much beyond 8 to 12 cm. Transabdominal US allows for better global visualization of the pelvis and may better image some large adnexal masses or high-riding ovaries, which may not be completely visualized with TV technique.
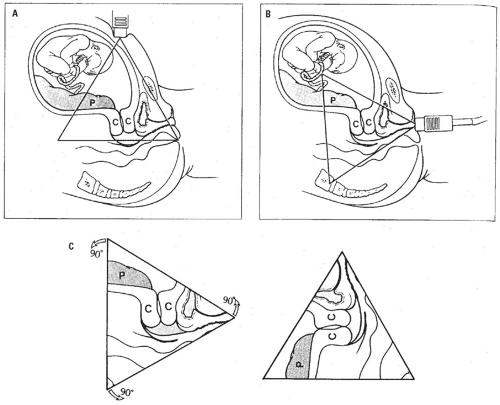
TV sonography is the preferred method of pelvic US and doesn’t require full bladder, which optimizes transabdominal examination. Details of the TV technique will not be discussed in depth here; any basic US textbook will have this information. Placement of the TV probe is similar to a speculum exam, and the technique of introduction can be mastered relatively simply by an experienced physician or sonographer. (However, finding some pelvic structures can be quite challenging and will be addressed further on). The transducer, covered with sterile condom and gel, is placed into the vagina and oriented in the longitudinal plane, such that the bladder is visualized in the upper left of the image and posterior structures (rectum) are on the bottom right of the image. The conventional anteflexed uterus presents with the fundus oriented toward the left of the image just beneath the bladder (Fig. 16.5A,B). If the uterus is retroflexed, the fundus will be directed to the right inferior corner of the image. Rotating the transducer 90 degrees produces a more oblique coronal view traditionally labeled as transverse, referring to the plane of the transducer (Fig. 16.5C). By anteroposterior angulation of the probe, the uterus can be imaged in its entirety. Imaging of the adnexa is performed
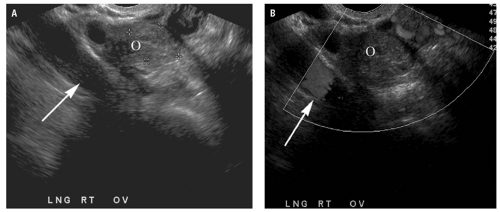
by angling the probe to the patient’s left or right. On occasion, the ovaries may be difficult to locate, particularly in postmenopausal women, and a useful landmark is the internal iliac vessels, which often reside just posterior and lateral to the ovary (Fig. 16.6). During real-time scanning, bowel loops will usually undergo peristalsis and so may be excluded as nonovarian tissue.
by angling the probe to the patient’s left or right. On occasion, the ovaries may be difficult to locate, particularly in postmenopausal women, and a useful landmark is the internal iliac vessels, which often reside just posterior and lateral to the ovary (Fig. 16.6). During real-time scanning, bowel loops will usually undergo peristalsis and so may be excluded as nonovarian tissue.
The transducer requirements for TVUS are unique and deserve mention. A higher frequency is used with TV than transabdominal sonography because the transducer is close to the cervix, uterus, and ovaries, so the overall depth coverage of the beam is not as important. The transducer is positioned in the vaginal fornices, and most state-of-the-art probes have almost 180 degrees of coverage and so can obtain a large field of view given the high frequency (6 to 10 cm). The method of emergent pelvic US performed in our radiology or emergency department is as follows: If the patient comes with a full bladder or a catheter in place, we commence with a transabdominal study
(through the full bladder) and progress (if necessary) to a TV study. In some cases of fetal demise or placental abruption, the transabdominal study suffices. We then have the patient void or empty the bladder through a catheter and proceed to TV technique. In most cases of gynecologic or obstetrical emergencies, the study is incomplete without TV scanning. If the patient arrives with an empty or partially distended bladder, she is asked to void and we proceed directly to TV scanning.
(through the full bladder) and progress (if necessary) to a TV study. In some cases of fetal demise or placental abruption, the transabdominal study suffices. We then have the patient void or empty the bladder through a catheter and proceed to TV technique. In most cases of gynecologic or obstetrical emergencies, the study is incomplete without TV scanning. If the patient arrives with an empty or partially distended bladder, she is asked to void and we proceed directly to TV scanning.
Computed Tomography and Magnetic Resonance Imaging
CT and MRI are usually secondary imaging tests in patients with a gynecologic or obstetrical emergency. CT is best performed 1 to 2 hours after administration of oral contrast material (300 to 600 mL) to opacify the bowel, taking contiguous 5-mm thick images to cover the entire pelvis. Helical scanning allows the entire pelvis to be scanned in 5 to 15 seconds and is generally acquired with a pitch of 1 to 2 (pitch = table speed ÷ slice collimation). Intravenous contrast is occasionally indicated and can be helpful in suspected pelvic abscesses or acute appendicitis or even to delineate the blood vessels from nonvascular structures. MRI usually includes T1-gradient echo and fast T2-weighted sequences in multiple imaging planes. Occasionally, short T1 inversion recovery (STIR) or specialized gradientecho pulse sequences may be helpful. Gadolinium is the generic intravenous contrast agent used in MRI, but its use is rarely indicated in emergent pelvic imaging and is relatively contraindicated in obstetrical imaging. The role of fetal MRI, a recently developed technique with very selective indications (fetal central nervous system [CNS] anomalies, placenta accreta), will not be discussed here due to space limitations and the fact that it is rarely an emergent study.
Normal Imaging Anatomy
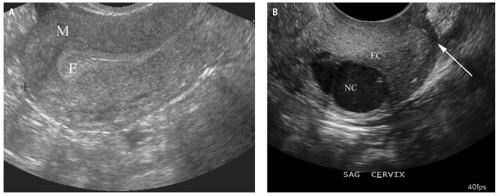
The uterus, on US, appears as an oval or elliptical organ that resides posterior to the bladder and anterior to the rectum. Its size is dependent on the age and childbearing status of the patient. In premenarche, the uterus is small, ranging from 3 to 4 cm in maximum length. For the menstrual years in nulliparous women, it reaches 6 to 8 cm, and in multiparous women, it may enlarge from 8 to 10 cm. Postmenopausal women have a smaller uterus that measures 4 to 6 cm.9 The uterus is composed of an echogenic endometrial stripe (Fig. 16.7A) that varies in thickness relative to the point in the menstrual cycle, reflecting the hormonal status, and
is generally 3 to 15 mm thick in premenopausal women—thicker in the secretory phase (latter half of menstrual cycle). The myometrium consists of the inner zone or junctional zone, which is slightly hypoechoic compared with the outer myometrium, which is of a medium-level homogeneous echo texture. However, this distinction is not often visible on US imaging and is better seen on pelvic MRI. The cervix is a smooth muscular structure that resembles a small “barrel” and can best be imaged in the longitudinal plane (Fig. 16.7B).
is generally 3 to 15 mm thick in premenopausal women—thicker in the secretory phase (latter half of menstrual cycle). The myometrium consists of the inner zone or junctional zone, which is slightly hypoechoic compared with the outer myometrium, which is of a medium-level homogeneous echo texture. However, this distinction is not often visible on US imaging and is better seen on pelvic MRI. The cervix is a smooth muscular structure that resembles a small “barrel” and can best be imaged in the longitudinal plane (Fig. 16.7B).
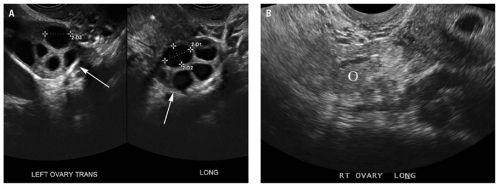
Ovarian size also depends on patient age and menstrual status, with premenarchal ovaries measuring 2 to 6 mL (volume = length × width × height × 0.52); those of menstruating women, 8 to 18 mL (often with small follicles); and those of postmenopausal women, less than 6 to 8 mL.8 Ovaries may be difficult to recognize in prepubertal and postmenopausal patients because of the lack of follicles, which are usually apparent in the menstruating years (Fig. 16.8). The sonographic appearance of ovarian stroma is homogeneous and similar in echogenicity to the myometrium. The fallopian tubes are thin, elongated (7 to 12 cm), paired structures coursing from the uterine cornua (or horn) to lie next to the ovary, but they are not generally visualized on US unless they are distended with fluid, blood, or an ectopic pregnancy (Fig. 16.9). Most of the paraovarian structures visualized by US are bowel loops, which can be seen to undergo peristalsis during real-time scanning—one of the reasons that physicians should be physically present for the US examination in the emergent setting.
US is extremely operator dependent, and virtually, any two-dimensional plane of scanning is possible with experience and knowledge of pelvic anatomy. The operator must have the flexibility to go beyond the standard transverse and sagittal planes, as much patient anatomy does not adhere to the traditional anatomy textbooks. Traditionally, transabdominal images are obtained in the transverse and longitudinal planes, with oblique images added as necessary. The uterus typically sits in the midline or just off midline in the true pelvis, with paired ovaries laterally adjacent to the fundus, but these are notorious for lying outside of the classic ovarian fossa. Occasionally, ovaries may reside on a long mesosalpinx, and they may rest behind the uterus (in the cul-de-sac) or out toward the pelvic sidewall or even up in the false pelvis.
TV technique (as described earlier) is more difficult to learn than transabdominal scanning, as the few customary anatomic landmarks are limited, and hands-on scanning experience is essential to become familiar with the variations in pelvic anatomy and the subtle probe mechanics for obtaining an excellent TV image. The longitudinal view is relatively straightforward anatomically, but the transverse view is semiaxial or semicoronal in the anatomic planes. All permutations in between are possible,
and oblique imaging is quite helpful for demonstrating the uterus and ovaries, which are rarely midline (or in the same anatomic plane) structures as in the anatomy textbooks. It is essential to become familiar with the TV probe used because the angle of the beam is variable, and side-, end-, and oblique-fire transducer options are all possibilities.
and oblique imaging is quite helpful for demonstrating the uterus and ovaries, which are rarely midline (or in the same anatomic plane) structures as in the anatomy textbooks. It is essential to become familiar with the TV probe used because the angle of the beam is variable, and side-, end-, and oblique-fire transducer options are all possibilities.
The location and appearance of the uterus and ovary are variable on CT (and anatomically) and are not particularly well defined due to their soft tissue density being similar to that of bowel. If bowel is not opacified with contrast material, it may be difficult to distinguish from the uterus and adnexal structures. In general, CT is not indicated in the acute gynecologic emergency, and US is the primary imaging modality. On occasion, MRI may be indicated because of its larger, more global visualization of the female pelvis. The pelvic organs have a characteristic appearance on T2-weighted images (T2WIs). The uterus is depicted as a high-signal endometrium, an inner myometrium (or junctional zone) of lower signal, and an outer myometrium of intermediate signal (Fig. 16.10). The ovaries are characterized by the high T2 signal follicles that are present in the menstruating years that help to identify the ovaries; the ovarian stroma is of low-to-medium signal intensity on T2WIs (Fig. 16.11).
GYNECOLOGIC EMERGENCIES
The problem of acute pelvic pain (defined as <48 hours duration) in young to middle-aged women is a common clinical dilemma. The most
frequent causes are ovarian cyst (enlargement or rupture) or torsion, PID, ectopic pregnancy, endometriosis, or less likely in the acute emergency setting, an ovarian or uterine neoplasm. A negative US is useful in excluding significant pathology in most cases. All patients of childbearing age should ideally have a pregnancy test, preferably a serum human chorionic gonadotropin (B-hCG), before being evaluated with US or other imaging, as the quantitative levels of the pregnancy test largely influences the interpretation of the sonographic findings. Briefly stated, if the B-hCG is more than 2,000 mIU and the patient has a normal pregnancy, then a gestational sac should be identified in the endometrial cavity. If not present, then there is a concern for a nonviable pregnancy, either an ectopic or a spontaneous miscarriage.
frequent causes are ovarian cyst (enlargement or rupture) or torsion, PID, ectopic pregnancy, endometriosis, or less likely in the acute emergency setting, an ovarian or uterine neoplasm. A negative US is useful in excluding significant pathology in most cases. All patients of childbearing age should ideally have a pregnancy test, preferably a serum human chorionic gonadotropin (B-hCG), before being evaluated with US or other imaging, as the quantitative levels of the pregnancy test largely influences the interpretation of the sonographic findings. Briefly stated, if the B-hCG is more than 2,000 mIU and the patient has a normal pregnancy, then a gestational sac should be identified in the endometrial cavity. If not present, then there is a concern for a nonviable pregnancy, either an ectopic or a spontaneous miscarriage.
Ovarian Cysts and Neoplasms
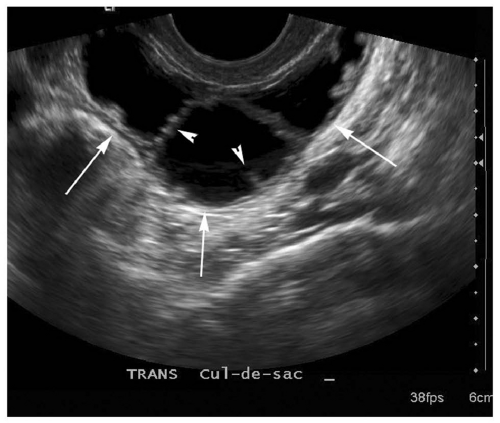
The functioning (premenopausal) ovary frequently contains follicles (arbitrarily defined as smaller than 2.5 cm), functional or small physiologic cysts (defined as larger than 2.5 cm), or corpus luteum cysts. Theca lutein cysts (associated with high hCG levels, i.e., from a molar pregnancy) are much less frequent but are often quite large (10 to 20 cm) and typically bilateral (40% to 60%). A simple cyst is defined by four sonographic criteria: It is anechoic; has a smooth, well defined, thin wall; has enhanced through transmission; and is unilocular. Bleeding into a cyst causes homogeneous, low-level echoes,
and the characteristic “snowstorm” or “spider’s web” appearance (Fig. 16.12). It must be noted, however, that endometriomas may also frequently present with this sonographic appearance or may be more homogeneous in echo texture (Fig. 16.13). Hemorrhagic cysts can also have these thicker septations or loculations.
and the characteristic “snowstorm” or “spider’s web” appearance (Fig. 16.12). It must be noted, however, that endometriomas may also frequently present with this sonographic appearance or may be more homogeneous in echo texture (Fig. 16.13). Hemorrhagic cysts can also have these thicker septations or loculations.
If a cyst contains mural nodules or papillary projections, thick walls, or solid echogenic foci, a neoplasm must be considered a strong possibility. Coarse calcifications or multiple strongly echogenic foci in an ovarian mass suggest a dermoid, as do echogenic, irregular foci superimposed on a low-level, homogeneously echogenic background. However, these calcifications should not be confused with the more common finding of multiple peripheral, tiny echogenic foci present in the ovaries (up to 37%), which most likely represent the echogenic walls of superficial epithelial inclusion cysts, which are too small to resolve at US (Fig. 16.14).
Most ovarian tumors are not acutely symptomatic until they enlarge enough to compress or displace adjacent structures (bladder, rectum, intestines), allow for ovarian torsion, or metastasize. Much interest has developed in attempting to differentiate benign from malignant ovarian masses with US, and most sonographic experts feel that differentiation is possible in 80% to 90% of cases. Specific sonographic morphology, and not spectral or color Doppler blood flow analysis, is the predominant means for discrimination: More simple-appearing cysts tend to be benign, and the more complex or solid masses have a higher chance of malignancy. Of course, the presence of ascites should always heighten suspicion of ovarian malignancy, given the absence of a pelvic infection or ovarian torsion.
Ovarian Torsion
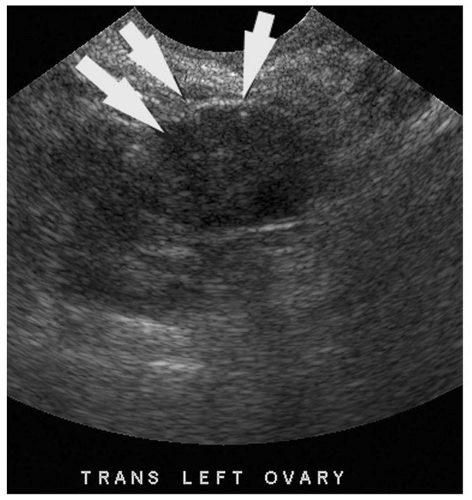
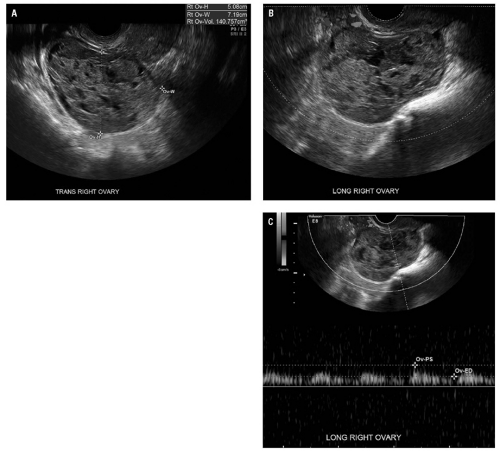
Ovarian torsion occurs most commonly in patients with a benign adnexal cyst or mass, which predisposes to twisting of the ovarian pedicle along its long axis. The usual clinical presentation is pelvic pain, nausea, vomiting, and/or fever. However, the diagnosis is often difficult, as the presentation is often atypical, both clinically and sonographically, and US remains the workhorse imaging modality. It often allows for differentiation of the other entities in the differential, from acute appendicitis, ovarian cyst or rupture, to PID. Most often, ovarian torsion at sonography is depicted as a large cystic or complex cystic mass, often midline, with diminished blood
flow (Fig. 16.15). The differential diagnosis for torsion includes causes of complex cystic adnexal masses: Ectopic pregnancy, TOA, endometrioma, or teratoma (Fig. 16.16). In theory, torsion should result in decreased blood flow to the ovary, but because the ovary has a dual blood supply, the results on color flow Doppler sonography are variable. The chronicity and completeness of the torsion are also factors in the sonographic appearance, with some cases of intermittent torsion-detorsion (ITD) being very problematic to diagnose, depending on which part of the ITD cycle the patient is in when examined with US. According to Vijayaraghan and Fleischer, a positive whirlpool sign in the twisted vascular pedicle of the ovary is the most definitive sign of ovarian torsion. Absence of blood flow in the twisted pedicle
and visualization of the flow in the artery alone are predictive of nonviability of the ovary.
flow (Fig. 16.15). The differential diagnosis for torsion includes causes of complex cystic adnexal masses: Ectopic pregnancy, TOA, endometrioma, or teratoma (Fig. 16.16). In theory, torsion should result in decreased blood flow to the ovary, but because the ovary has a dual blood supply, the results on color flow Doppler sonography are variable. The chronicity and completeness of the torsion are also factors in the sonographic appearance, with some cases of intermittent torsion-detorsion (ITD) being very problematic to diagnose, depending on which part of the ITD cycle the patient is in when examined with US. According to Vijayaraghan and Fleischer, a positive whirlpool sign in the twisted vascular pedicle of the ovary is the most definitive sign of ovarian torsion. Absence of blood flow in the twisted pedicle
and visualization of the flow in the artery alone are predictive of nonviability of the ovary.
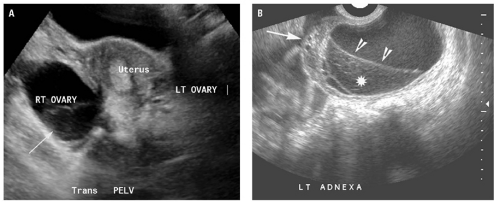
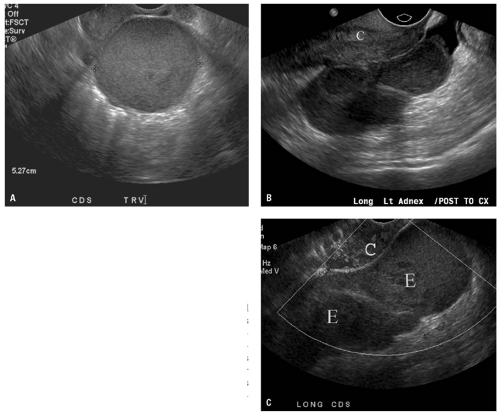 Figure 16.13. Endometrioma. A: Transverse transvaginal image of homogeneously low-level echogenic cystic mass (electronic calipers) in the cul-de-sac, proven to be endometriosis at surgery in a 36-year-old woman. B: Transvaginal sagittal image of the cul-de-sac in same patient shows tubular endometrioma behind the cervix (C). C: Color Doppler image in same orientation as Figure 16.13B shows the endometrioma (arrows) to be avascular in nature, consistent with old hemorrhage. E, endometrium; C, cervix. |
One study evaluated 20 patients with surgically proven ovarian torsion. Sonographic findings varied with age: Prepubertal girls usually demonstrated large, extrapelvic cystic, or complex cystic masses, whereas pubertal females most often had a solid adnexal mass. Color Doppler flow was variable and did not correlate with morphology or age of patient. Other authors report that if torsion is complete, venous blood flow will be absent with preservation of abnormal arterial flow (high-resistive index or low-peak systolic flow) (Fig. 16.17). In another study, Fleischer et al. showed that specific signs on color Doppler US were predictive of ovarian viability: Lack of central venous ovarian flow represented infarction of the ovary, and the presence of venous flow indicated an ovary that was salvageable. However, a more recent study of 10 surgically proven cases of ovarian torsion with color Doppler analysis reported that color flow was normal in 60%. They showed that when color Doppler blood flow is abnormal, the time to diagnosis is less and the hospital stay significantly shortened. In ovulation induction (OI) patients, however, the sensitivity fell to 25% for abnormal color Doppler flow. In this population, it seems, abnormal color Doppler US is even less accurate and caution is undertaken when evaluating this subset of patients in the emergent setting.
Pelvic Inflammatory Disease
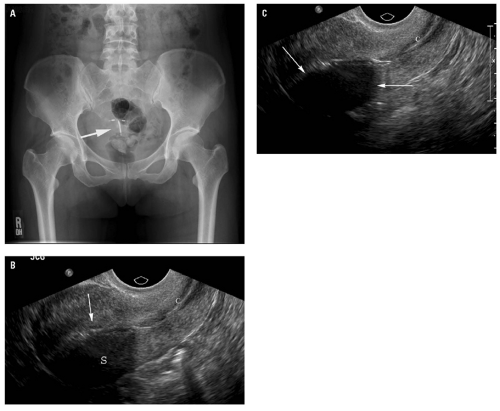
PID is diagnosed clinically and with positive cultures in most patients without requiring imaging. US or, less often, CT is important in medically refractory or complicated cases. PID is a disease predominantly seen in the young, sexually active female who is infected with common sexually transmitted pathogens (Chlamydia and gonococcus most commonly), initially infecting the cervix and uterus and then propagating proximally to fallopian tubes and ovaries. Clinically, the patients may have few or no symptoms, yet the sonographic findings may be striking or vice versa. Patients with TOA often have fewer signs of acute illness than those without TOA.16 On US, the characteristic finding of PID is a dilated, thick-walled tubular structure with incomplete septa (characteristic mucosal folds) containing internal echoes in the adnexa (pyosalpinx), or a thickened, echogenic tubular structure in the adnexal region (Fig. 16.18). In the subacute or chronic stage of disease, one may
encounter a hydrosalpinx (a thin-walled tubular structure without internal echoes) or a “string of beads” sign. A thicker wall correlates well with more acute disease.17 Bilateral adnexal involvement is common with PID. If left untreated, the infection often extends to ovaries and paraovarian tissues as a large cystic or complex cystic mass— the TOA (Fig. 16.19



encounter a hydrosalpinx (a thin-walled tubular structure without internal echoes) or a “string of beads” sign. A thicker wall correlates well with more acute disease.17 Bilateral adnexal involvement is common with PID. If left untreated, the infection often extends to ovaries and paraovarian tissues as a large cystic or complex cystic mass— the TOA (Fig. 16.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree