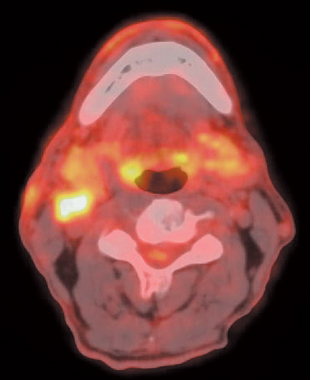
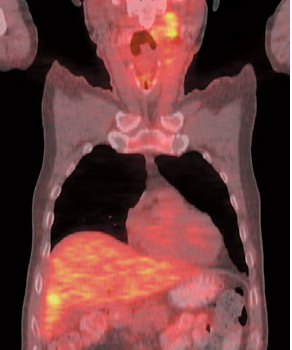
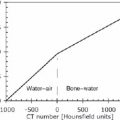
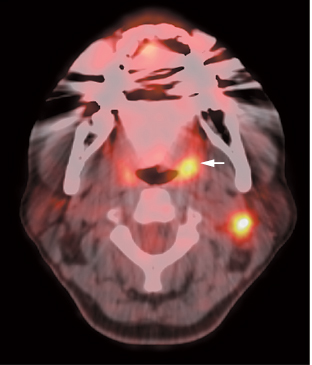
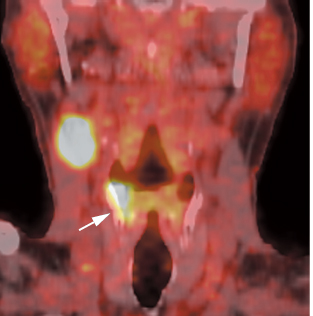
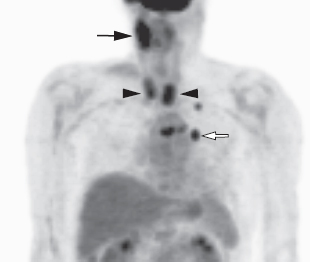
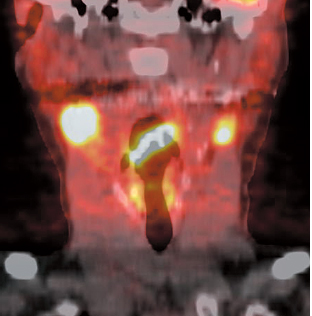
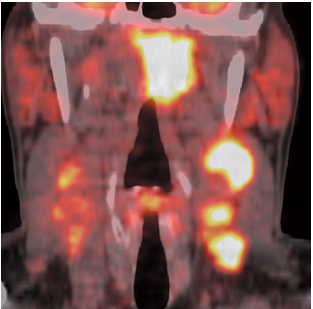
13 Fig. 13.2 Primary tumor localization: tonsil. Axial positron emission tomography/computed tomography scan in a patient with a malignant left neck node demonstrates uptake in the primary tumor in the left tonsil (arrow). Fig. 13.3 Primary tumor localization: pyriform sinus. Coronal positron emission tomography computed tomography scan in a patient with a malignant right neck node demonstrates uptake in the primary tumor in the right pyriform sinus (arrow). A PET scan, which includes the thorax, will detect lung lesions not seen on chest x-ray. However, in general, CT is more sensitive than PET for lung lesions. Fig. 13.5 Synchronrous lung cancer. Coronal positron emission tomography scan in a patient with a right parotid malignancy (arrow) demonstrates a synchronous left upper lobe lung cancer (open arrow) with mediastinal metastases and another nodule in the left apex. Uptake in the thyroid (arrowheads) is nonspecific but related to thyroiditis in this patient. Fig. 13.6 Synchronous colon cancer. Coronal positron emission tomography scan in a patient with head and neck cancer with metastatic cervical nodes also demonstrates a synchronous sigmoid carcinoma (arrow). Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; PET, positron emission tomography. Fig. 13.7 Metastastic supraglottic cancer. Coronal positron emission tomography/computed tomography scan demonstrates a supraglottic cancer with metastases to bilateral neck nodes. Supraglottic cancers have a propensity for bilateral nodal metastases. Fig. 13.8 Metastatic nasopharyngeal cancer. Coronal positron emission tomography/computed tomography scan demonstrates a large left nasopharyngeal cancer with metastases to bilateral neck nodes. Nasopharyngeal cancers have a propensity for bilateral nodal metastases. PET is very valuable for detecting recurrent disease, as CT and MRI are limited in the postoperative/posttherapy neck.
Head and Neck Cancer
Eugene C. Lin and Abass Alavi
 Cervical Metastasis, Unknown Primary
Cervical Metastasis, Unknown Primary
Clinical Indication: B
Accuracy/Comparison to Other Modalities
Pearls/Pitfalls
 Staging
Staging
Clinical Indication: B

Accuracy/Comparison with Other Modalities
Pearls/Pitfalls
Sensitivity %
Specificity %
PET
87–90
80–93
CT/MRI
61–97
21–100
 Recurrence
Recurrence
Clinical Indication: A
| Sensitivity % | Specificity % | |
| PET | 100 | 96 |
| Tc-99m sestamibi | 73 | 96 |
| Tc-99m tetrofosmin | 64 | 96 |
Abbreviations: PET, positron emission tomography; Tc, technetium.
Accuracy
- Overall. Sensitivity 84 to 100%, specificity 61 to 93%21
- By region22
- Local. Sensitivity 97%, specificity 79%
- Regional. Sensitivity 92%, specificity 95%
- Distant. Sensitivity 94%, specificity 96%22
- Local. Sensitivity 97%, specificity 79%
- PET is sensitive and specific for disease at regional and distant sites. specificity is lower in the head and neck region due to false-positive results from inflammation related to infection or other processes.22 The primary value of PET is its high negative predictive value.23
- If PET is negative, no biopsy is needed.
- If PET is positive and biopsy is negative, a follow-up scan should be performed. Decreased activity on the follow-up scan indicates that the initial result was likely false-positive due to an inflammatory process.24
Comparison with Other Modalities25
- Other radionuclides. PET is more sensitive than sestamibi, tetrofosmin, or thallium; specificity is comparable. However, sestamibi or tetrofosmin combined with CT is comparable to PET (Table 13.2).25,26
- MRI.27 See Table 13.3.
Pearls
- SUV. SUV cutoffs of 3.0 to 3.2 have been used to detect recurrence.22,28 However, an increasing SUV on dual time point PET imaging is of greater value than a single SUV measurement.
- Radiation has minimal effect on FDG uptake in normal structures. There is mildly increased uptake, mostly in muscle, in the early postradiation period, which is related to inflammation.
Pitfalls
- Tumor stunning. A delay in PET imaging for at least 4 months after radiation can be helpful in avoiding false-negative results from presumed tumor “stunning.”29
- Laryngeal uptake. Laryngeal uptake of FDG can be noted normally, particularly in the posterior portion (see Chapter 6).
- It is better to use asymmetry of uptake rather than absolute uptake in the larynx as a criterion of abnormality.
- Anterior uptake is more suggestive of a malignant process than uptake in posterior structures.
- However, laryngeal uptake may be asymmetric due to postoperative changes or vocal cord paralysis.
- It is better to use asymmetry of uptake rather than absolute uptake in the larynx as a criterion of abnormality.
- Postoperative. False-positive results are particularly unavoidable when evaluating for recurrence. Besides the typical physiologic areas of uptake, abnormal patterns of uptake can be seen from postoperative distortion of normal anatomy or as a result of postsurgical or therapeutic inflammation. How ever, reconstruction hardware typically does not interfere with interpretability. Osteotomy sites do have slightly greater (25% on average) uptake, but less than that seen in tumor.30 PET/CT can be used in free flap cases with acceptable levels of accuracy.
| Sensitivity % | Specificity % | |
| PET | 100 | 93 |
| MRI | 62 | 43 |
 Therapy Response/Prognosis31
Therapy Response/Prognosis31
Clinical Indication: B
Potential applications of PET in therapy response are
- Evaluation of residual disease following radiotherapy or chemoradiotherapy. PET is useful in evaluating therapy response in preoperative induction chemoradiotherapy, chemoradiotherapy protocols that are aimed at organ preservation, and definitive radiotherapy.11,12
- Postchemoradiotherapy. In patients with head and neck squamous cell cancer, chemoradiotherapy regimens that attempt to preserve organ function (e.g., larynx and tongue) often achieve regional control at the primary site. However, residual tumor is more likely if cervical nodal disease (particularly N2 or N3) is present, even if there is a clinical complete response. In patients with advanced nodal disease, posttreatment neck dissection can often reduce regional recurrence. The role of PET in predicting the need for posttreatment neck dissection is controversial. PET/CT does appear to be superior to contrast-enhanced CT for predicting persistent disease in the neck.32 Some data suggest that PET is a reliable predictor of the absence of residual tumor after chemoradiotherapy in the N positive neck,33 but this is not supported by some studies.34
- Postradiotherapy. There is controversy over the role of neck dissection after definitive radiation therapy for advanced neck disease. One study suggests that PET/CT is more accurate than CT in assessing therapy response in this setting.35 Limited data suggest that if there is no residual lymphadenopathy and a negative PET, neck dissection can be withheld.36 However, if there is substantial residual lymphadenopathy (> 2 cm) and a negative PET, further studies are required before withholding neck dissection.37
- Postchemoradiotherapy. In patients with head and neck squamous cell cancer, chemoradiotherapy regimens that attempt to preserve organ function (e.g., larynx and tongue) often achieve regional control at the primary site. However, residual tumor is more likely if cervical nodal disease (particularly N2 or N3) is present, even if there is a clinical complete response. In patients with advanced nodal disease, posttreatment neck dissection can often reduce regional recurrence. The role of PET in predicting the need for posttreatment neck dissection is controversial. PET/CT does appear to be superior to contrast-enhanced CT for predicting persistent disease in the neck.32 Some data suggest that PET is a reliable predictor of the absence of residual tumor after chemoradiotherapy in the N positive neck,33 but this is not supported by some studies.34
- Prognosis. PET is helpful for both early and late prediction of outcome.
Table 13.4 Sensitivity and specificity of Positron Emission Tomography Compared with Other Imaging Modalities in the Evaluation of Therapy Response
Sensitivity %
Specificity %
PET/CT
77
93
CT
92
47
Abbreviations: CT, computed tomography; PET, positron emission tomography.
- Primary tumor. High SUV (> 10) in the primary tumor is correlated with poor prognosis.38
- Nodes. Nodal SUV does not predict prognosis.39
- Early prediction. Low levels of tumor metabolic activity after 1 cycle of chemotherapy or radiation predict complete remission and longer survival.
- Late prediction. High SUV after treatment predicts local recurrence and decreased survival.
- Primary tumor. High SUV (> 10) in the primary tumor is correlated with poor prognosis.38
Accuracy/Comparison with Other Modalities
Postradiotherapy.35 See Table 13.4.
Pitfalls
- PET has a limited clinical value in assessing response to postoperative adjuvant chemoradiotherapy.
- Postsurgical inflammatory reactions can cause false-positive results and therefore render subsequent response assessment inaccurate.
- Microscopic residual disease cannot be detected.
- Postsurgical inflammatory reactions can cause false-positive results and therefore render subsequent response assessment inaccurate.
- As in all settings, there should be a substantial time interval between radiotherapy and PET imaging. Typically, false-negative results are more commonly seen if imaging is performed early after radiation. Some studies suggest that a 4- or 8-week delay is adequate3536 for evaluating therapy response, but other studies suggest 12 weeks or longer.37 If postradiotherapy neck dissection is being considered, PET may be more valuable if it can be accurately performed earlier after therapy (within 12 weeks), as fibrosis can increase the technical difficulty and morbidity of delayed neck dissection.40
- Osteoradionecrosis can cause false-positive results.41
 Radiotherapy Planning
Radiotherapy Planning
Clinical Indication: B
Potential applications of PET in radiotherapy planning are42
- Coregistration of PET and treatment planning CT
- Detection of additional/distant disease by PET
- Gross tumor volume assessment: gross tumor volume assessment by PET is closer to the surgical specimen than CT or MRI, although all imaging modalities overestimate tumor extension.
 Characterization of Head and Neck Tumors
Characterization of Head and Neck Tumors
Clinical Indication: D
- Parotid lesions. PET cannot distinguish between benign and malignant parotid tumors.43 Warthin tumors and pleomorphic adenomas can have fluorodeoxyglucose (FDG) uptake. High-grade salivary gland tumors tend to have more uptake than lower grade tumors, but there is substantial overlap.44 PET and PET/CT may be superior to CT for staging patients’ known salivary gland malignancies.44–46
- Cystic neck masses. PET/CT may not be accurate in identifying malignancy in adults with cystic neck masses.47
 PET/CT
PET/CT
PET/CT is of particular value in head and neck evaluations, given the complex anatomy and relative lack of anatomical landmarks on PET.
- The use of PET/CT compared with PET alone will decrease the fraction of equivocal lesions by 53%, greatly improve lesion localization (see Fig. 8.1, p. 89), slightly improve accuracy, and change management in 18% of cases.11,12
- Particular attention must be paid to the possibility of mislocalization on PET/CT studies due to movement of the head between the CT and PET studies (see Figs. 8.6, p. 92 and 8.7, p. 93).
- If PET/CT or fusion with CT or MRI is not available, potential anatomical landmarks that can be used to aid in localization include the tonsils, palate, tongue, floor of mouth, salivary glands, mandible, and cervical spine.
References
- Miller FR, Karnad AB, Eng T, Hussey DH, Stan MH, Otto RA. Management of the unknown primary carcinoma: long-term follow-up on a negative PET scan and negative panendoscopy. Head Neck 2008;30(1):28–34
- Kole AC, Nieweg OE, Pruim J, et al. Detection of unknown occult primary tumors using positron emission tomography. Cancer 1998;82(6):1160–1166
- Greven KM, Keyes JW Jr, Williams DW III, et al. Occult primary tumors of the head and neck: lack of benefit from positron emission tomography imaging with 2-[F-18]fluoro-2-deoxy-D-glucose. Cancer 1999;86(1):114–118
- Wartski M, Le Stanc E, Gontier E, et al. In search of an unknown primary tumour presenting with cervical metastases: performance of hybrid FDG-PET-CT. Nucl Med Commun 2007;28(5):365–371
- Nabili V, Zaia B, Blackwell KE, Head CS, Grabski K, Sercarz JA. Positron emission tomography: poor sensitivity for occult tonsillar cancer. Am J Otolaryngol 2007;28(3):153–157
- Hannah A, Scott AM, Tochon-Danguy H, et al. Evaluation of 18F-fluorodeoxyglucose positron emission tomography and computed tomography with histopathologic correlation in the initial staging of head and neck cancer. Ann Surg 2002;236(2):208–217
- Ng SH, Yen TC, Chang JT, et al. Prospective study of [18F]fluorodeoxyglucose positron emission tomography and computed tomography and magnetic resonance imaging in oral cavity squamous cell carcinoma with palpably negative neck. J Clin Oncol 2006;24(27):4371–4376
- Schoder H, Carlson DL, Kraus DH, et al. 18F-FDG PET/CT for detecting nodal metastases in patients with oral cancer staged N0 by clinical examination and CT/MRI. J Nucl Med 2006;47(5):755–762
- Wensing BM, Vogel WV, Marres HA, et al. FDG-PET in the clinically negative neck in oral squamous cell carcinoma. Laryngoscope 2006;116(5):809–813
- Kovacs AF, Dobert N, Gaa J, et al. Positron emission tomography in combination with sentinel node biopsy reduces the rate of elective neck dissections in the treatment of oral and oropharyngeal cancer. J Clin Oncol 2004;22(19):3973–3980
- Schoder H, Yeung HW. Positron emission imaging of head and neck can cer, including thyroid carcinoma. Semin Nucl Med 2004;34(3):180–197
- Schoder H, Yeung HW, Gonen M, et al. Head and neck cancer: clinical usefulness and accuracy of PET/CT image fusion. Radiology 2004;231(1):65–72
- Kim SY, Roh JL, Kim MR, et al. Use of 18F-FDG PET for primary treatment strategy in patients with squamous cell carcinoma of the oropharynx. J Nucl Med 2007;48(5):752–757
- Schoder H, Yeung HW. Positron emission imaging of head and neck cancer, including thyroid carcinoma. Semin Nucl Med 2004;34(3):180–197
- Stuckensen T, Kovacs AF, Adams S, Baum RP. Staging of the neck in patients with oral cavity squamous cell carcinomas: a prospective comparison of PET, ultrasound, CT and MRI. J Craniomaxillofac Surg 2000;28(6):319–324
- Liu FY, Chang JT, Wang HM, et al. [18F]fluorodeoxyglucose positron emission tomography is more sensitive than skeletal scintigraphy for detecting bone metastasis in endemic nasopharyngeal carcinoma at initial staging. J Clin Oncol 2006;24(4):599–604
- Lowe VJ, Stack BC Jr. Esophageal cancer and head and neck cancer. Semin Roentgenol 2002;37(2):140–150
- Goerres GW, Schmid DT, Schuknecht B, Eyrich GK. Bone invasion in patients with oral cavity cancer: comparison of conventional CT with PET/CT and SPECT/CT. Radiology 2005;237(1):281–287
- Murakami R, Uozumi H, Hirai T, et al. Impact of FDG-PET/CT imaging on nodal staging for head-and-neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys 2007;68(2):377–382
- Yamamoto Y, Wong TZ, Turkington TG, Hawk TC, Coleman RE. Head and neck cancer: dedicated FDG PET/CT protocol for detection–phantom and initial clinical studies. Radiology 2007;244(1):263–272
- Kutler DI, Wong RJ, Schoder H, Kraus DH. The current status of positron-emission tomography scanning in the evaluation and follow-up of patients with head and neck cancer. Curr Opin Otolaryngol Head Neck Surg 2006;14(2):73–81
- Wong RJ, Lin DT, Schoder H, et al. Diagnostic and prognostic value of [(18)F]fluorodeoxyglucose positron emission tomography for recurrent head and neck squamous cell carcinoma. J Clin Oncol 2002;20(20):4199–4208
- Ryan WR, Fee WE Jr, Le QT, Pinto HA. Positron-emission tomography for surveillance of head and neck cancer. Laryngoscope 2005;115(4):645–650
- Terhaard CH, Bongers V, van Rijk PP, Hordijk GJ. F-18-fluoro-deoxy-glucose positron-emission tomography scanning in detection of local recurrence after radiotherapy for laryngeal/pharyngeal cancer. Head Neck 2001;23(11):933–941
- Kao CH, Shiau YC, Shen YY, Yen RF. Detection of recurrent or persistent nasopharyngeal carcinomas after radiotherapy with technetium-99m methoxyisobutylisonitrile single photon emission computed tomography and computed tomography: comparison with 18-fluoro-2-deoxyglucose positron emission tomography. Cancer 2002;94(7):1981–1986
- Kao CH, Tsai SC, Wang JJ, et al. Comparing 18-fluoro-2-deoxyglucose positron emission tomography with a combination of technetium 99m tetrofosmin single photon emission computed tomography and computed tomography to detect recurrent or persistent nasopharyngeal carcinomas after radiotherapy. Cancer 2001;92(2):434–439
- Yen RF, Hung RL, Pan MH, et al. 18-fluoro-2-deoxy-glucose positron emission tomography in detecting residual/recurrent nasopharyngeal carcinomas and comparison with magnetic resonance imaging. Cancer 2003;98(2):283–287
- Yao M, Luo P, Hoffman HT, et al. Pathology and FDG PET correlation of residual lymph nodes in head and neck cancer after radiation treatment. Am J Clin Oncol 2007;30(3):264–270
- Keyes JW Jr, Watson NE Jr, Williams DW III, et al. FDG PET in head and neck cancer. AJR Am J Roentgenol 1997;169(6):1663–1669
- Oliver C, Muthukrishnan A, Mountz J, Deeb E, Johnson J, Deleyiannis F. Interpretability of PET/CT imaging in head and neck cancer patients following composite mandibular resection and osteocutaneous free flap reconstruction. Head Neck 2008;30(2):187–193
- Kostakoglu L, Goldsmith SJ. PET in the assessment of therapy response in patients with carcinoma of the head and neck and of the esophagus. J Nucl Med 2004;45(1):56–68
- Chen AY, Vilaseca I, Hudgins PA, et al. PET-CT vs contrast-enhanced CT: what is the role for each after chemoradiation for advanced oropharyngeal cancer? Head Neck 2006;28(6):487–495
- Brkovich VS, Miller FR, Karnad AB, et al. The role of positron emission tomography scans in the management of the N-positive neck in head and neck squamous cell carcinoma after chemoradiotherapy. Laryngoscope 2006;116(6):855–858
- Gourin CG, Williams HT, Seabolt WN, et al. Utility of positron emission tomography-computed tomography in identification of residual nodal disease after chemoradiation for advanced head and neck cancer. Laryngoscope 2006;116(5):705–710
- Andrade RS, Heron DE, Degirmenci B, et al. Posttreatment assessment of response using FDG-PET/CT for patients treated with definitive radiation therapy for head and neck cancers. Int J Radiat Oncol Biol Phys 2006;65(5):1315–1322
- Kim SY, Lee SW, Nam SY, et al. The feasibility of 18F-FDG PET scans 1 month after completing radiotherapy of squamous cell carcinoma of the head and neck. J Nucl Med 2007;48(3):373–378
- Yao M, Smith RB, Graham MM, et al. The role of FDG PET in management of neck metastasis from head-and-neck cancer after definitive radiation treatment. Int J Radiat Oncol Biol Phys 2005;63(4):991–999
- Halfpenny W, Hain SF, Biassoni L, et al. FDG-PET. A possible prognostic factor in head and neck cancer. Br J Cancer 2002;86(4):512–516
- Schwartz DL, Rajendran J, Yueh B, et al. FDG-PET prediction of head and neck squamous cell cancer outcomes. Arch Otolaryngol Head Neck Surg 2004;130(12):1361–1367
- Frank SJ, Chao KS, Schwartz DL, et al. Technology insight: PET and PET/CT in head and neck tumor staging and radiation therapy planning. Nat Clin Pract Oncol 2005;2(10):526–533
- Liu SH, Chang JT, Ng SH, Chan SC, Yen TC. False positive fluorine-18 fluorodeoxy-D-glucose positron emission tomography finding caused by osteoradionecrosis in a nasopharyngeal carcinoma patient. Br J Radiol 2004;77(915):257–260
- Daisne JF, Duprez T, Weynand B, et al. Tumor volume in pharyngolaryngeal squamous cell carcinoma: comparison at CT, MR imaging, and FDG PET and validation with surgical specimen. Radiology 2004;233(1):93–100
- Rubello D, Nanni C, Castellucci P, et al. Does 18F-FDG PET/CT play a role in the differential diagnosis of parotid masses. Panminerva Med 2005;47(3):187–189
- Roh JL, Ryu CH, Choi SH, et al. Clinical utility of 18F-FDG PET for patients with salivary gland malignancies. J Nucl Med 2007;48(2):240–246
- Otsuka H, Graham MM, Kogame M, Nishitani H. The impact of FDG-PET in the management of patients with salivary gland malignancy. Ann Nucl Med 2005;19(8):691–694
- Jeong HS, Chung MK, Son YI, et al. Role of 18F-FDG PET/CT in management of high-grade salivary gland malignancies. J Nucl Med 2007;48(8):1237–1244
- Ferris RL, Branstetter BF, Nayak JV. Diagnostic utility of positron emission tomography-computed tomography for predicting malignancy in cystic neck masses in adults. Laryngoscope 2005;115(11):1979–1982
- Kole AC, Nieweg OE, Pruim J, et al. Detection of unknown occult primary tumors using positron emission tomography. Cancer 1998;82(6):1160–1166
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree