The “head and neck” encompasses extracranial structures from the skull base to the thoracic inlet including the orbits, nasal cavity, paranasal sinuses (PNSs), face, jaws, temporal bones and soft tissues of the neck, oral cavity, and upper aerodigestive tract. In this chapter we describe approaches to imaging, highlighting typical and atypical imaging features and the differential diagnosis for a variety of processes that involve the pediatric head and neck.
Imaging Technques and Modalities
The choice of imaging modality depends on the clinical indication, region of interest, patient age, need for sedation or anesthesia, and parental concerns regarding the use of ionizing radiation.
Conventional Radiography
Plain films (PF) or digital radiography is requested for evaluation of osseous structures in trauma, to evaluate the sinuses for suspected sinusitis, and the soft tissues of the neck for airway narrowing caused by adenoidal hypertrophy, laryngotracheobronchitis, or occasionally epiglottitis. Intraoperative or postoperative temporal bone PFs are useful for assessment of the position of cochlear implant arrays. Radiopaque foreign bodies are also well demonstrated by PF or digital radiography. This is of particular importance in assessing patients undergoing magnetic resonance imaging (MRI) where the presence of a ferromagnetic foreign body could contraindicate the examination.
Fluoroscopy
Video fluoroscopy (VF) may be used to assess airway and palatal motion during speech. VF and a barium pharyngogram or esophagogram demonstrate causes of extrinsic airway compression (eg, vascular slings/rings) and intrinsic or mural abnormalities affecting the pharynx or esophagus. A barium pharyngogram can also be used to evaluate for an underlying pyriform sinus tract in a child with recurrent infrahyoid neck infections. This examination should be performed after resolution of infection/inflammation to avoid a false-negative examination from edematous effacement of the tract. Conventional sialography is seldom performed in children but can be used to demonstrate salivary ductal anatomy in sialectasis.
Ultrasonography
Real-time ultrasonography is often the initial mode of evaluation for pediatric neck masses and thyroid and ocular lesions. Ultrasonography helps distinguish between solid versus cystic masses and nodal versus nonnodal neck masses. Cystic masses range from anechoic with increased through transmission to mildly or moderately echoic depending on the presence of hemorrhagic, proteinaceous, or purulent material. Oscillating compression of the mass with the transducer helps demonstrate the swirling nature of echogenic contents as seen in viscous or solid-appearing cystic masses such as abscess or lymphatic malformation (LM). Doppler ultrasonography provides important information regarding vascularity, direction of flow, and pulsatility. For example, Doppler ultrasonography is used to distinguish venous from arterial flow and helps characterize masses as markedly vascular (eg, proliferating infantile hemangioma [IH]), moderately vascular, or avascular.
Computed Tomography
High-resolution multidetector computed tomography (CT) provides information that is complementary to that provided by ultrasonography and MRI, and is particularly helpful in osseous assessment. CT is also useful for demonstrating calcifications such as phleboliths, tumoral calcification, and sialoliths. Images should be acquired using the lowest dose that provides diagnostic quality images. Axial images are generally acquired or reformatted parallel to the hard palate, with coronal reformatted images perpendicular to the plane of the hard palate. For indications that require contrast, images are obtained only with contrast. CT angiography (CTA) and CT venography (CTV) require the acquisition of images during the administration of a bolus of intravenous contrast, timed to demonstrate the arterial or venous anatomy, respectively.
Neck CT is primarily used for evaluating acute infection, and sometimes characterization of congenital or acquired neck masses. Images are acquired with intravenous (IV) contrast using the “split-dose” technique. After acquiring the scout images, half of the IV contrast dose is administered as a bolus, followed by a 3-minute pause. Helical 3-mm images are then acquired during the rapid administration of the second half of the contrast bolus. This technique allows the contrast to percolate through enhancing lesions while still providing excellent information about neck vasculature. Multiplanar reconstructions (MPRs) are created in soft tissue and bone algorithms.
CT of the orbits, sinuses, nasal cavity, and facial bones is obtained without contrast for evaluating congenital lesions (eg, choanal atresia), trauma, chronic sinus disease, and osseous lesions. Acute complicated sinus and orbital infection, suspected invasive fungal sinusitis, and soft tissue tumors or developmental masses are evaluated with contrast-enhanced CT (CECT). Three-dimensional (3D) images can be created for assessment and follow-up of craniofacial malformations.
Temporal bone CT without contrast is used for evaluation of congenital malformations, chronic infection, cholesteatoma, trauma, and conductive, mixed, or sensorineural hearing loss (SNHL). Depending on the need for sedation, MRI is sometimes preferred for SNHL evaluation. CECT is required for the evaluation of suspected coalescent mastoiditis (CoM) and temporal bone region masses. Temporal bone CT is also useful for the evaluation of local vascular variants.
Radionuclide Imaging
[ 18 F]fluorodeoxyglucose ([ 18 F]-FDG) positron emission tomography (PET)-CT is an extremely useful modality for the diagnosis, staging, and follow-up of malignant head and neck tumors. Radionuclide imaging is helpful in evaluating the pediatric thyroid gland. Iodine 123 ( 123 I) and technetium 99m ( 99m Tc) pertechnetate are primarily used. Indications for thyroid radionuclide imaging include identification of ectopic thyroid tissue, assessment of congenital hypothyroidism, and evaluation of a solitary thyroid nodule. Metaiodobenzylguanidine labeled with radioactive iodine is used for the assessment, staging, and follow-up of neuroblastoma.
Magnetic Resonance Imaging
MRI provides superior soft tissue characterization that is complementary to that provided by ultrasonography and CT. MRI is indicated for the initial evaluation and follow-up of congenital and acquired masses and for the assessment of complicated sinus, orbital, and temporal bone infections. Pulse sequences typically include multiplanar, high-resolution, fat-suppressed (FS) T2-weighted (T2W) or T2 short tau inversion recovery images, axial diffusion-weighted images (DWI), axial T1-weighted (T1W) images, and gadolinium (Gd)-enhanced FS T1W images. The field of view and slice thickness vary depending on the size of the patient and lesion. Vascular pulsation in the neck produces phase artifact, which should be taken into consideration when selecting the direction of the phase and frequency-encoding steps, to minimize phase artifact through the region of interest. Non-echo-planar DWI images are sometimes acquired to mitigate the geometric distortion caused by susceptibility effects at the skull base. Susceptibility sequences are sometimes required for confirmation of hemorrhage or mineralization. A flow-sensitive gradient echo sequence or 3D time-of-flight MR angiogram (MRA) is useful for evaluating vascular malformations, vascular tumors, and arterial morphology of the neck. Time-of-flight MR venography (MRV) is used for assessment of venous thrombosis or venous anatomy. Gd-enhanced gradient echo images are of use for the depiction of nonocclusive venous thrombi and are a useful adjunct to MRV.
MR of the temporal bones is useful for evaluating SNHL and cranial nerve (CN) palsies. Imaging at 3T with heavily T2W sequences such as axial and oblique sagittal T2 3D Sampling Perfection with Application optimized Contrast using different flip angle Evolutions (SPACE) or Constructive Interference in Steady State (CISS) provide excellent detail of the fluid-containing inner ear structures. These sequences also provide exquisite detail of the globes. Gd-enhanced, thin-section, high-resolution FS T1W images are indicated for acquired SNHL, tumors/masses, and inflammatory conditions involving the temporal bones, PNSs, and orbits. Images can be obtained immediately after the administration of contrast, but delayed (eg, 5 minutes) images may be of use to detect subtle enhancement, for example, if autoimmune labyrinthitis is suspected.
Angiography
Conventional angiography is reserved for detailed assessment of neck vasculature and for endovascular treatment of arteriovenous malformation (AVM) and fistulae (AVFs) and certain vascular tumors (eg, juvenile angiofibroma [JA]).
Congenital and Developmental Abnormalities
Orbit and Globe
Normal Development and Anatomy
The eye and orbit develop from neuroectoderm, cutaneous ectoderm, mesoderm, and neural crest cells. The optic primordium gives rise to the optic vesicle and stalk, which become the globe and the optic nerve (ON). A transitory vascular system, the hyaloid artery and its branches, forms the primary vitreous and then involutes. The hyaloid artery and vein ultimately become the central artery and vein of the retina. The globe is located within the orbital fat. The outer layer of the globe is the opaque sclera and translucent cornea; the middle vascular layer is the uvea, which includes the choroid, ciliary body, and iris. The inner layer is the retina, which is continuous posteriorly with the ON. The anterior segment structures lie anterior to the lens. The iris and ciliary body divide the anterior segment into anterior and posterior chambers, both of which contain aqueous humor. The posterior segment structures are posterior to the lens and include the vitreous humor. The lacrimal gland lies in the superolateral orbit; tears drain via the superior and inferior lacrimal canaliculi into the inferomedially located lacrimal sac before coursing into the nasolacrimal duct, which drains into the inferior meatus of the nasal cavity.
The orbit contains orbital fascia, fat, extraocular muscles (EOMs), the globe, lacrimal system, vessels, and nerves. The optic foramen lies at the orbital apex and transmits the ON and ophthalmic artery. The superior orbital fissure lies inferolateral to the optic foramen and transmits CN III and IV, the ophthalmic division of CN V, CN VI, sympathetic nerves, and the superior ophthalmic vein (SOV). The inferior orbital fissure separates the lateral orbital wall and orbital floor and connects posteromedially with the pterygopalatine fossa and posterolaterally with the retromaxillary fissure and infratemporal fossa. Most of the EOMs originate at the orbital apex and insert on the globe, forming a cone about the globe and ON. The EOMs consist of the levator palpebrae superioris the superior, middle, lateral, and inferior rectus muscles and the superior and inferior oblique muscles. The orbital fascia forms the periosteum of the orbit, and its anterior reflection about the globe is termed the orbital septum. This septum separates the anterior preseptal space from the posterior postseptal space. The postseptal space is further subdivided by the muscular cone into intraconal and extraconal components. Growth of the orbital cavity is contingent upon normal growth of the globe. The globe is 75% of adult size at birth and is fully grown by age 7 years.
Congenital and Developmental Abnormalities of the Globe
Anophthalmos and Microphthalmos.
Anophthalmos or anophthalmia refers to complete absence of the globe, and microphthalmos or microphthalmia refers to ocular hypoplasia [ Fig. 10.1 ]. These conditions, which are an important cause of blindness, can be unilateral or bilateral, symmetric or asymmetric in appearance, and syndromic (eg, the holoprosencephaly [HPE] disorders, trisomy 13) or nonsyndromic in nature. Congenital anophthalmos is rare and usually results from a genetic mutation or an insult early during gestation. Anophthalmos can also result from degeneration of the optic vesicle. Imaging of anophthalmos reveals a small orbit and absent globe. Microphthalmos is characterized by a small globe. It is usually associated with a small orbit unless there is an associated large orbital cyst. Microphthalmos can also be seen in association with other ocular abnormalities such as anterior (eg, cataract) or posterior (eg, coloboma) segment dysgenesis.

Macrophthalmos.
A large globe is frequently caused by severe myopia that is sporadic or syndromic in nature (eg, Stickler syndrome). Buphthalmos is enlargement of the globe due to increased intraocular pressure, as seen in glaucoma, which may be caused by various factors such as neurofibromatosis type 1 (NF-1). Imaging is helpful in excluding an intraorbital mass and reveals enlargement of the globe [ Fig. 10.1 ]. The differential diagnosis includes congenital cystic eye in which a cystic orbital mass is present without identifiable ocular structures.
Staphyloma.
Staphyloma is an ocular outpouching caused by stretching and thinning of the sclera and uvea without an actual focal defect in the layers. Causative factors include prior infection or inflammation, severe axial myopia, glaucoma, trauma, and surgery. On imaging, staphyloma appears as a bulge typically involving the posterior contour of the globe [ Fig. 10.2 ].

Coloboma.
Coloboma is a congenital ocular defect that results from faulty closure of the embryonic optic fissure producing a notch or gap in the affected part of the iris, retina, choroid, or optic disc. Coloboma can be unilateral or bilateral and may be associated with a normally sized globe, microphthalmos, or glaucoma. Coloboma is often familial and occurs in several syndromes including Treacher-Collins syndrome (TCS), CHARGE, and trisomies 13 and 18. On ultrasonography, CT, or MR, coloboma appears as a protrusion of vitreous into a chorioretinal gap or into the optic disc [ Fig. 10.2 ]. The differential diagnosis for chorioretinal coloboma is staphyloma (acquired bulge lined by retina and choroid). The differential diagnosis for ON head coloboma is the morning glory disc anomaly (MGDA; see later).
Morning Glory Disc Anomaly.
MGDA is an uncommon optic disc malformation that resembles a morning glory flower. MGDA is usually unilateral and sporadic but is sometimes associated with cephaloceles, moyamoya disease, and PHACES association ( p osterior fossa malformations, h emangiomas, a rterial anomalies, c oarctation of the aorta and cardiac defects, e ye abnormalities, s ternal clefting and s upraumbilical abdominal raphe). On funduscopy, there is optic disc excavation with an annulus of chorioretinal pigmentary changes, straightening of retinal vessels, and central glial tissue. On MR, there is a funnel-shaped optic disc defect with elevation of adjacent retinal margins and lack of normal ON head enhancement. There is abnormal tissue within the distal ON with effacement of the adjacent subarachnoid space [ Fig. 10.2 ] and sometimes ON atrophy. The funnel-shaped morphology and heaped up margins distinguish MGDA from coloboma.
Malformations of the Orbit
Hypertelorism and Hypotelorism.
Hypertelorism, referring to an increased distance between the medial orbital walls, is a feature of numerous syndromes and developmental disorders including syndromic craniosynostosis, cephalocele, agenesis of the corpus callosum (ACC), and frontonasal dysplasia [ Fig. 10.3 ]. Imaging of hypertelorism demonstrates widely spaced orbits. Dystopia canthorum refers to telecanthus in which there is an increased distance between the inner canthi of the eyes with lateral displacement of the lacrimal puncta, as seen in some types of Waardenburg syndrome.

Hypotelorism refers to a decreased distance between the medial orbital walls, as seen in a variety of syndromic and developmental disorders including the HPEs, arrhinencephaly, and premature fusion of the metopic and sagittal sutures. Other manifestations of HPE include cyclophthalmos or cyclopia (single median eye), synophthalmos (partial fusion of the eyes), ethmocephaly (hypotelorism with median proboscis), and cebocephaly (hypotelorism with rudimentary nose/single nostril). Imaging reveals closely set eyes with normal-sized globes, microphthalmos, or anophthalmos, and sometimes other craniofacial anomalies [ Fig. 10.3 ].
Abnormalities of Orbital Size.
Orbital enlargement results from bony defects as seen with NF-1-associated sphenoid dysplasia or orbital cephalocele, or arises because of a congenital or acquired intraorbital mass such as an ocular cyst, vascular anomaly, or tumor. A small orbit is a feature of anophthalmos or microphthalmos resulting from malformation or an early insult (eg, infection, ocular enucleation, or orbital irradiation) [ Fig. 10.1 ]. Exorbitism referring to shallow orbits with ventral protrusion of the globes as seen in syndromic craniosynostosis (eg, Apert and Crouzon syndromes) [ Fig. 10.3 ] should not be mistaken for proptosis in which ocular protrusion occurs from orbital mass effect caused by tumor, inflammation, or thyroid ophthalmopathy. Enlargement of the optic canal occurs because of ON tumor and/or dural ectasia, as seen in NF-1. A small optic canal accompanies ON hypoplasia and disorders such as osteopetrosis and fibrous dysplasia.
Optic Nerve Hypoplasia.
ON hypoplasia is a developmentally small ON. This anomaly can be unilateral or bilateral and isolated or syndromic. Numerous syndromes, many with well-characterized underlying genetic mutations, are associated with ON hypoplasia, perhaps the best known being septooptic dysplasia (absent septum pellucidum, midline forebrain anomalies, and pituitary hypoplasia). On MR, the affected ONs, chiasm, and tract(s) appear diminutive [ Fig. 10.1 ]. The differential diagnosis is ON atrophy.
Persistent Hyperplastic Primary Vitreous.
Persistent hyperplastic primary vitreous (PHPV) results from failure of the normal process of embryonic hyaloid vasculature regression, with persistence of hyperplastic primary vitreous and the capillary vascular network overlying the lens. PHPV is usually unilateral and associated with microphthalmos, cataract, and leukocoria. Bilateral PHPV is seen in various syndromic disorders such as trisomy 13 and Walker-Warburg disease. PHPV is characterized by a triangular morphology of the lens, which “points” toward a linear density (on CT) or hypointensity (T2W MR) representing retrolental fibrovascular tissue and the persistent hyaloid remnant of Cloquet canal [ Fig. 10.4 ]. Abnormal vitreous density or signal intensity reflects hemorrhage and layering debris. Complications include glaucoma and progressive retinal hemorrhage leading over time to phthisis bulbi. The differential diagnosis includes Coats disease, retinopathy of prematurity (ROP), retinal detachment, and retinoblastoma (RB).

Coats Disease.
Coats disease results from defective retinal vascular development, leading to retinal telangiectasias with leaky vessels, subretinal exudates, and retinal detachment. Coats disease is usually unilateral and presents with leukocoria and strabismus. On CT, Coats disease appears as a hyperdense exudate, usually without calcification [ Fig. 10.4 ]. On MR, the subretinal exudate appears hyperintense on T1W and T2W images. The differential diagnosis includes RB, but RB presents as a mineralized mass with or without retinal detachment.
Retinopathy of Prematurity.
ROP or retrolental fibroplasia is attributed to excessive oxygen therapy in premature, low-birth-weight infants, but is now relatively uncommon. ROP manifests as fibrovascular organization of the vitreous sometimes resulting in retinal detachment, microphthalmos, and blindness. On CT the globes appear small and hyperdense, sometimes with dystrophic mineralization. The differential diagnosis includes prior infection (eg, cytomegalovirus [CMV]) and RB (calcified mass, normal-sized globe). MR shows abnormal signal intensity caused by subretinal hemorrhages [ Fig. 10.4 ].
Ocular and Orbital Abnormalities Associated With Craniofacial and Central Nervous System Malformations
Ocular and orbital anomalies are seen in numerous craniofacial disorders. Cephaloceles and nasal dermoids are variably associated with widening of the nasal bridge, hypertelorism, and sometimes intracranial anomalies (eg, ACC, polymicrogyria). The syndromic craniosynostoses are associated with hypertelorism, exorbitism, midfacial hypoplasia, and occasionally cleft lip and palate (CLCP). Hypertelorism is a feature of frontonasal dysplasia with broadening of the nasal bridge and a bifid nose [ Fig. 10.3 ]. HPE disorders are associated with hypotelorism, microphthalmia, nasal anomalies (eg, pyriform aperture stenosis or more severe manifestations), and sometimes central megaincisor. Septooptic dysplasia is associated with optic hypoplasia.
NF-1 is characterized by sphenoid bone deficiency with pulsatile proptosis and orbital deformity [ Fig. 10.5 ], buphthalmos, ON glioma, nerve sheath tumors, and rarely rhabdomyosarcoma (RMS). Orbital manifestations of Sturge-Weber syndrome include buphthalmos, glaucoma, venous dysplasia, and venous hypertension. Retinal neuroglial hamartomas appearing as small, hypointense retinal nodules on T2W MR are a feature of tuberous sclerosis [ Fig. 10.5 ]. Enhancing retinal hemangioblastomas occur in von Hippel-Lindau disease.

Joubert syndrome is characterized by absent cerebellar vermis, abnormal eye movements, and sometimes retinal abnormalities with chorioretinal coloboma. Walker-Warburg syndrome and the congenital muscular dystrophies feature ocular abnormalities such as cataracts and other anterior segment anomalies, microphthalmos, PHPV, retinal detachment, vitreous hemorrhage, coloboma, and ON hypoplasia. Aicardi syndrome (X-linked, affects females) is characterized by ACC, polymicrogyria, choroid plexus tumors, and chorioretinal lacunae. Ocular manifestations include microphthalmos, retinal detachment, coloboma, staphyloma, and cataract.
The congenital cranial dysinnervation disorders are characterized by abnormal development of cranial motor nuclei and absence or hypoplasia of affected CNs, leading to fibrosis of the affected EOMs (previously known as congenital fibrosis of the EOMs). Clinical signs depend on the affected CNs and include strabismus, gaze limitation or ophthalmoplegia, ptosis, and poorly reactive pupils. On high-resolution MR there is absence or hypoplasia of the affected CNs, and the affected EOMs appear small [ Fig. 10.5 ].
Developmental Masses and Anomalies
Malformation or maldevelopment of orbital tissues can create a variety of masses. The more frequently encountered lesions are described in the following subsections. Vascular malformations and lipoma are considered in a later section.
Dermoid and Epidermoid.
Dermoids are common congenital masses thought to arise from epithelial rests sequestered in bony sutures. A dermoid usually presents as a small, firm nodule, often along the lateral orbital rim. Dermoids (and less common epidermoids) are composed of cysts lined by keratinized, stratified squamous epithelium. Dermoids also sometimes contain hair and sebaceous glands. On CECT, dermoid/epidermoid appears as a well-defined, low-density mass with minimal, if any, peripheral enhancement. Bone remodeling or erosion is sharply defined and well corticated. Thick, irregular peripheral enhancement and irregular osseous destruction suggests inflammation/infection. Sometimes fatty density is seen within the cyst. On MR, dermoid/epidermoid appears rounded and sharply circumscribed, usually with high signal intensity on T2W images, decreased diffusivity, low signal intensity on T1W images, and minimal, if any, peripheral Gd enhancement. Fat content produces high signal intensity on T1W imaging that suppresses with FS techniques [ Fig. 10.6 ]. Imaging does not reliably distinguish between dermoid and epidermoid.

Nasolacrimal Duct Cyst.
Congenital nasolacrimal duct cyst (NLDC) or mucocele is a common anomaly thought to arise due to failure of canalization of the distal NLD at the valve of Hasner beneath the inferior turbinate on one or both sides. Clinical signs and symptoms include a cystic medial canthal swelling and/or neonatal nasal obstruction and respiratory distress. On imaging, NLDC appears as a cystic structure that is tubular on coronal images [ Fig. 10.7 ]. It extends inferiorly from the medial canthus and protrudes inferior to the inferior turbinate, sometimes with lacrimal sac enlargement. The differential diagnosis includes meningocele and cystic neuroglial heterotopia (NGH); unlike NLDC, these entities project superior to the inferior turbinate.

Lacrimal Gland Anomalies.
Lacrimal gland anomalies are uncommon and include ectopic or absent lacrimal tissue. Neoplastic transformation of ectopic lacrimal tissue is rare, especially in children.
Nasal Cavity, Paranasal Sinuses, Face, and Mandible
Normal Development and Anatomy
The facial structures develop from mesenchymal primordia surrounding the stomodeum (primitive mouth). The nasomedial processes create the philtrum of the lip, the premaxillary portion of the upper jaw, and the primary palate. The forehead, nose, and nasal septum derive from the frontonasal prominence. Portions of the upper lip, maxilla, and secondary palate derive from the maxillary processes. The nasolacrimal groove is located between the maxillary process and the nasal primordium and gives rise to the NLD and lacrimal sac. The mandible, lower lip, chin, and lower cheek arise from paired mandibular prominences. The muscles of mastication (first arch derivatives, innervated by CN V) and the muscles of facial expression (second arch derivatives, innervated by CN VII) are derived from mesodermal cells of the pharyngeal arches. The nasal cavities communicate with the nasopharynx and oral cavity after rupture of the oronasal membrane at the choanae. PNSs form as diverticula of the nasal cavity walls, and subsequently pneumatize with progressive development through childhood. Specialized olfactory epithelium develops along the roof of each nasal cavity and connects with the olfactory bulbs. The nasal cavity and PNSs are lined with respiratory epithelium.
At birth, the face is relatively small compared with the head, and this craniofacial proportion alters as the face enlarges during childhood. The neonate is an obligate nose breather. The nasal airway consists of the pyriform apertures anteriorly, the nasal cavities divided by the cartilaginous and bony nasal septum, and the posterior nasal choanae. The paired inferior, middle, superior, and sometimes supreme turbinates are located along the lateral nasal cavity. The cribriform plate and fovea ethmoidalis form the roof of the nasal cavity and ethmoid air cells, respectively, on each side. The U-shaped hard palate forms the nasal cavity floor. The developing teeth are closely related to the alveolar recesses of the maxillary antra. The pterygoid plates arise from the sphenoid bone and lie posterior to the maxillary antra. The pterygopalatine fossae, located between the maxillary antra and the pterygoid plates, communicate with the masticator spaces and inferior orbital fissures. The thin lamina papyracea separates the ethmoid air cells from the orbit and the orbital floor is formed by the roof of the maxillary antrum.
The maxillary sinuses and ethmoid air cells are present at birth and attain adult size by about 10 to 12 years. The sphenoid sinuses develop at about 2 years of age, converting from hematopoietic to fatty marrow before pneumatization. The sphenoid sinus attains adult size by about 14 years of age. The frontal sinuses develop toward the end of the first decade of life. Each frontal sinus drains through an ostium into the frontal recess and ultimately into the middle meatus. The anterior ethmoid air cells drain into the hiatus semilunaris and middle meatus. The maxillary sinus also drains into the middle meatus via the maxillary ostium and infundibulum. The ostiomeatal unit consists of the infundibulum, uncinate process, hiatus semilunaris, ethmoid bulla, and middle meatus. The posterior ethmoid air cells and sphenoid sinus drain into the sphenoethmoidal recess and superior meatus. The sphenoid sinuses are close to the ONs, pituitary gland, cavernous sinuses, and internal carotid arteries (ICAs).
Developmental Sinonasal Variants
The turbinates are convex toward the nasal cavity. Turbinates with paradoxical curvature are concave toward the nasal cavity. Concha bullosa or middle turbinate pneumatization is a common anatomic variant that can cause nasal septal deviation [ Fig. 10.8 ] if unilateral or asymmetric. Nasal septal deviation with or without a septal spur can be developmental (eg, in association with unilateral cleft palate) or acquired (eg, post trauma). Underpneumatization or hyperpneumatization of the PNS can occur [ Fig. 10.8 ]. The maxillary sinuses often contain septations and frequently have accessory ostia. Ethmoid air cell variations include infraorbital extension (Haller cells), extension ventral to the NLD (agger nasi cells), supraorbital air cells, and sphenoethmoidal air cells (Onodi cells). Sometimes the ethmoid bulla is quite large. It is not unusual to see thinning or even apparent dehiscence of the lamina papyracea. Not infrequently, developmental variants occur in the sphenoid bone that may be mistaken for a dermoid or tumor; however, the hallmark of the developmental lesion is a corticated lucency on CT [ Fig. 10.8 ], facilitated diffusion with fluid or fatty signal intensity on MR, and no Gd enhancement.

Congenital Nasal Malformation
Nasal agenesis with complete absence of the nose and nasal cavity is uncommon and is usually a manifestation of a craniofacial syndrome. Midnasal cavity stenosis and midface hypoplasia is seen in a variety of craniofacial disorders, especially the syndromic craniosynostoses.
Pyriform aperture stenosis is an uncommon congenital narrowing of the anterior nasal apertures that presents as neonatal airway obstruction. On CT or MR, there is narrowing of the anterior nasal apertures associated with a triangular hard palate morphology [ Fig. 10.9 ]. Pyriform aperture stenosis is sometimes associated with a solitary central megaincisor (SCMI) [ Fig. 10.9 ]. Pyriform aperture stenosis and SCMI sometimes occur with HPE. Therefore an infant with pyriform aperture stenosis and SCMI should undergo brain MRI to assess for HPE. Other facial features of HPE include a small/absent nose, hypotelorism, and midline cleft palate.

Choanal atresia is congenital posterior choanal obstruction. Bilateral choanal atresia causes neonatal airway obstruction. Unilateral atresia is more common and presents later with unilateral nasal stuffiness. CT or MRI shows thickening of the posterior vomer and medial deviation of the lateral wall(s) of the nasal cavity and pterygoid plates [ Fig. 10.9 ]. The anomaly is either bony (lateral wall meets thickened vomer) or part bony and part membranous, with pooling of nasal secretions. Bilateral choanal atresia is typically associated with CHARGE syndrome ( c oloboma, h eart defect, a tresia choanae, r etarded growth and development, g enital hypoplasia, and e ar anomalies). Other imaging features of CHARGE include CLCP, skull base anomalies (constricted clivus), olfactory bulb hypoplasia/aplasia, pituitary and pontine hypoplasia, and hypoplasia of the vestibules with absent/hypoplastic semicircular canals (SCCs).
Congenital Nasal Masses
Congenital nasal masses include NLDC (discussed earlier), disorders resulting from defective neural tube closure, vascular malformations (discussed later), and congenital tumors (eg, teratoma, hemangioma, and juvenile xanthogranuloma; see later). Disorders resulting from defective neural tube closure include cephalocele, neuroglial heterotopia (NGH), dermoid, and dermal sinus tract (DST). Development of the nasofrontal region results in transient nasofrontal structures termed the fonticulus frontalis (separating the nasal and frontal bones) and prenasal space (between the nasal bones and the underlying nasal capsule) that involute in early gestation. Usually the only remnant is the foramen cecum, ventral to the crista galli, containing fibrous tissue and sometimes a small emissary vein. Persistence of these primitive structures may be associated with a dural diverticulum and protrusion of intracranial contents as a nasofrontal or nasoethmoidal cephalocele. Partial or complete obliteration of the intracranial connection results in sequestered NGH (“nasal glioma”). NGH can be extranasal (faulty fonticulus frontalis closure) or intranasal (faulty prenasal space closure). With dural diverticulum regression, incorporation of surface ectoderm may form a DST and/or dermoid along the nasal dorsum, sometimes extending from the nasal bridge through the nasofrontal suture into the anterior cranial fossa, or extending along the nasal septum and sometimes through the foramen cecum to the anterior cranial fossa. Nasal dermoid can occur alone or with a DST.
The clinical presentation of children with congenital nasal masses includes respiratory distress caused by nasal obstruction or a visible mass. The presence of a nasal pit, hairy tuft, or small midline nasal nodule suggests a diagnosis of nasal dermoid. A bluish mass suggests venous malformation (VM); a strawberry-red mass is characteristic of IH, or occasionally NGH. Yellowish discoloration suggests juvenile xanthogranuloma. On CECT a dermoid appears rounded and hypodense with minimal, if any, peripheral enhancement. DST appears similar with a tubular morphology. Bone erosion is smoothly marginated and corticated, sometimes appearing as a “gap” at the nasofrontal suture or as scalloping of the affected bone. Enlargement of the foramen cecum greater than 2 mm suggests intracranial extension; however, the foramen cecum is not fully ossified at younger than 2 years of age. For this reason it is helpful to obtain CECT to delineate the enhancing cartilaginous anterior skull base. NGH may appear isodense with brain, or cerebrospinal fluid (CSF), or may have a combination of two densities, and typically appears as a teardrop-shaped mass within the anterior nasal cavity extending from an intact anterior cranial fossa into the nasal cavity, superior to the inferior turbinate. Cephaloceles (meningocele, encephalocele) appear similar to NGH but communicate with intracranial CSF (meningocele) or contain herniated dysplastic brain and CSF (encephalocele).
More frequently, MRI alone is performed to avoid ionizing radiation, with CT reserved for osseous assessment if indicated. Dermoid and DST usually appear hyperintense on thin-section high-resolution FS T2W MRI. DWI characteristically reveals decreased diffusivity; non-echo-planar imaging technique with imaging in the coronal plane is preferred because of decreased susceptibility effects at the skull base compared with the echo planar imaging technique or imaging in the axial plane, thereby improving diagnostic sensitivity. The signal intensity of dermoid on T1W images is variable depending on lipid content, which can render a lesion inconspicuous on all FS sequences [ Fig. 10.10 ]. There is usually minimal, if any, peripheral Gd enhancement on FS T1W images. NGH appears isointense with CSF or brain, or there may be a combination of two signal intensities [ Fig. 10.10 ]. Although usually nonenhancing, mild enhancement is occasionally observed. Sometimes a small fibrous tag extending toward foramen cecum renders distinction from a cephalocele challenging. Cephaloceles contain CSF and sometimes dysplastic brain with intracranial communication through a nasofrontal or nasoethmoidal bone defect [ Fig. 10.10 ].

Fissural Cysts
Fissural cysts arise along lines of embryologic fusion and include nasolabial (along the base of nasal ala and anterior nasal fold), nasopalatine (incisive canal), and median palatal (midline hard palate) cysts. On CT, these cysts appear lucent with smooth bone remodeling.
Facial and Mandibular Anomalies
Cleft Lip and Palate.
Clefts arise from abnormal fusion or maldevelopment of facial structures. CLCP are unilateral or bilateral, and complete (separated margins) or incomplete (partially opposed margins). The most common CLCP is off midline, resulting from failure of fusion of nasomedial and maxillary processes. Syndromic association is highest with bilateral CLCP, is next highest with unilateral CLCP, and seen least often with unilateral cleft lip. CLCP is well seen on fetal ultrasonography/MRI particularly when complete. Bilateral CLCP results in a protruding premaxillary segment [ Fig. 10.11 ]. Determining the extent of hard palate involvement can be challenging. True midline/median CLCP is rare; associated hypertelorism should prompt a search for cephalocele and ACC. Hypotelorism with midline CLCP suggests HPE.

Isolated secondary cleft palate may result as follows: micrognathia → glossoptosis (tongue pushed up and back) → failure of apposition of secondary palatal shelves → U-shaped cleft palate [ Fig. 10.11 ]. The triad of micrognathia, glossoptosis, and postnatal feeding difficulty is termed Pierre Robin sequence. This descriptive term encompasses many syndromes (eg, 22q11del, Stickler, and TCS). Micrognathia should prompt a search for isolated cleft secondary palate which appears on sagittal fetal ultrasonography/MRI as a shortened hard palate with glossoptosis. Oblique (medial canthus to nose) and transverse facial clefts (laterally from mouth) are rare. Facial clefting can also result from amniotic bands.
Preoperative imaging of cleft palate with cone beam CT may be obtained to assess the bone over the roots of teeth along the cleft margins to determine the feasibility of successful bone grafting. Complications of CLCP include dental crowding, abnormal dental eruption, oronasal/oroantral fistulae, maxillary retrusion, midface hypoplasia, and nasal septal deviation, with disruption of speech, feeding, and Eustachian tube function.
Craniofacial Syndromes.
The syndromic craniosynostoses are characterized by premature fusion of coronal and other sutures. Many of these disorders (eg, Crouzon and Apert syndromes) also have hypertelorism, exorbitism, midface hypoplasia, and maxillary retrusion. Midface underdevelopment causes upper airway narrowing that is compounded by adenotonsillar hypertrophy. Fusion of multiple sutures produces a cloverleaf or “kleeblattschädel” skull deformity [ Fig. 10.12 ]. The hallmark of Apert syndrome is bicoronal craniosynostosis with wide patency of metopic and sagittal sutures, polysyndactyly, and malformed horizontal SCC.

Micrognathia is a small mandible and retrognathia is posterior mandibular positioning. Micrognathia (with retrognathia) can be sporadic or inherited, isolated or syndromic, and results in airway narrowing and sometimes obstruction. Numerous syndromes are associated with micrognathia. Images should be assessed for symmetry and facial malformation to determine the most likely causative factor. Unilateral micrognathia is the hallmark of hemifacial microsomia (HFM), a heterogeneous group of conditions of uncertain cause that involve the first and second brachial apparatus and neural crest derivatives [ Fig. 10.12 ]. There are also ipsilateral congenital external and middle ear anomalies, facial hypoplasia, hypoplasia of muscles of mastication and parotid gland, zygomatic arch hypoplasia, and sometimes transverse facial clefts. The Goldenhar HFM phenotype is characterized by epibulbar lipodermoids and vertebral and renal anomalies. Bilateral asymmetric micrognathia is seen in branchio-oto-renal syndrome (BOR). BOR is also associated with branchial cleft anomalies (eg, cysts or sinus tracts), characteristic temporal bone anomalies, and renal findings (eg, cysts). Bilateral symmetric micrognathia is a feature of TCS and Nager syndrome. TCS features marked micrognathia, sometimes with absent mandibular condyles, deficient zygomatic arches, posterior malar slanting, downward slanting palpebral fissures, coloboma, and severe bilateral temporal bone anomalies [ Fig. 10.12 ]. As mentioned earlier, Pierre Robin sequence refers to the clinical triad of micrognathia, glossoptosis (leading to U-shaped cleft palate), and feeding difficulty, featured in a variety of syndromes. Preoperative imaging of craniofacial disorders, before reconstructive surgery, requires low-dose CT with creation of MPRs and 3D images.
Ear and Temporal Bone
Normal Development and Anatomy
The external and middle ear are derived from branchial apparatus, and the internal ear is derived from neurectoderm. The first branchial cleft gives rise to the external auditory canal (EAC); the first branchial pouch forms the Eustachian tube and middle ear cavity (MEC). The auricles develop from the first and second branchial arches. The ossicles grow and ossify during fetal life. The malleus and incus are derived from the first and second branchial arches. The stapes suprastructure and tympanic segment of CN VII derive from the second branchial arch; the stapes footplate partly arises from otic capsule. MEC and mastoid antrum pneumatization commences in the fetus; aeration occurs after birth. Mastoid air cell pneumatization continues during childhood. The inner ear structures develop in the fetus; the cochlea and endolymphatic sac and duct are the last to differentiate.
The temporal bone comprises the squamosal, mastoid, tympanic, and petrous portions and the styloid process. The EAC is part cartilaginous and part bony (tympanic plate), bounded medially by the tympanic membrane (TM), which is attached to the tympanic plate, and scutum. The MEC is bounded laterally by the TM and medially by the cochlear promontory. On coronal CT images, the MEC is divided into the hypotympanum (below TM level), mesotympanum (at TM level), and epitympanum or attic (above TM). The tegmen tympani forms the MEC roof and continues laterally as the mastoid tegmen. Prussak space is located between the scutum, the TM pars flaccida, the lateral malleal ligament, and the malleus neck. The oval window is located over the vestibule, above the cochlear promontory. The carotid canal (CC) lies inferior to the cochlea. The internal jugular vein (IJV) lies inferior to the vestibule.
On axial images the anterior wall of the MEC includes the CC, Eustachian tube, and the semicanal for the tensor tympani tendon which attaches to the malleus. The posterior wall of the MEC has two recesses and an intervening bony protrusion, forming a W-shape in the axial plane. This consists of the sinus tympani (medially) separated by the pyramidal eminence from the facial recess (laterally). The stapedius tendon arises from the pyramidal eminence and attaches to the stapes. The round window niche overlies the cochlear basal turn. The MEC contains the ossicles: malleus, incus, and stapes. The malleus attaches to the TM and articulates with the incus in the attic, resembling an ice cream cone. The incus then curves downward and medially (long and lenticular processes) to articulate with the stapes. The stapes has two crura and a footplate attached to the oval window.
The inner ear is located in the petrous portion of the temporal bone (often simply referred to as the petrous bone) and consists of the cochlea, vestibular aqueduct (which contains the endolymphatic sac and duct), vestibule, SCC (superior, posterior, and lateral), cochlear aqueduct, facial nerve canal (FNC), and internal auditory canal (IAC), mostly enclosed within dense otic capsule bone. The cochlea consists of ![]() to
to ![]() turns, separated by the shelflike interscalar septum and a central conical bony projection (modiolus), and containing a wafer-thin osseous spiral lamina. The IAC transmits CNs VII and VIII; the medial IAC opening is the porus acusticus; the fundus is lateral. The crista falciformis (a horizontal bony plate) and Bill’s bar (a vertical crest) divide the IAC into quadrants: CN VII is located in the anterosuperior quadrant; CN VIII trifurcates into the anteroinferiorly located cochlear nerve and posteriorly located superior and inferior vestibular nerves. The cochlear nerve travels through the cochlear aperture into the modiolus. CN VII enters the labyrinthine FNC, forms an anterior genu where the geniculate ganglion is located, then travels posteriorly along the medial MEC in the tympanic FNC, passing beneath the lateral SCC and above the oval window. Next, CN VII forms the posterior genu, then courses inferiorly in the mastoid FNC. CN VII exits the stylomastoid foramen before entering the parotid gland. The chorda tympani branches off the mastoid segment of CN VII and courses toward the MEC. The exiting CN VII is prone to birth injury before mastoid process development.
turns, separated by the shelflike interscalar septum and a central conical bony projection (modiolus), and containing a wafer-thin osseous spiral lamina. The IAC transmits CNs VII and VIII; the medial IAC opening is the porus acusticus; the fundus is lateral. The crista falciformis (a horizontal bony plate) and Bill’s bar (a vertical crest) divide the IAC into quadrants: CN VII is located in the anterosuperior quadrant; CN VIII trifurcates into the anteroinferiorly located cochlear nerve and posteriorly located superior and inferior vestibular nerves. The cochlear nerve travels through the cochlear aperture into the modiolus. CN VII enters the labyrinthine FNC, forms an anterior genu where the geniculate ganglion is located, then travels posteriorly along the medial MEC in the tympanic FNC, passing beneath the lateral SCC and above the oval window. Next, CN VII forms the posterior genu, then courses inferiorly in the mastoid FNC. CN VII exits the stylomastoid foramen before entering the parotid gland. The chorda tympani branches off the mastoid segment of CN VII and courses toward the MEC. The exiting CN VII is prone to birth injury before mastoid process development.
Developmental Variants
On CT images obtained in the first few years of life, it is normal to see a thin pericochlear lucency ( cochlear cartilaginous cleft ); this ossifies over time and should not be mistaken for cochlear otospongiosis [ Fig. 10.13 ]. Under age 2 years the posterior petrous bone is not fully ossified, with a small depression adjacent to the vestibular aqueduct and thin bone over the SCC. It is important to bear these developmental variants in mind in order not to misdiagnose large vestibular aqueduct (LVA) or SCC dehiscence, respectively. In infancy there is also transient prominence of the subarcuate canal that travels between the superior SCC limbs; this should not be mistaken for bone erosion caused by an underlying mass [ Fig. 10.13 ].

Congenital External and Middle Ear Malformations
Because the external and middle ear structures are both derived from branchial apparatus, congenital external ear malformations are invariably associated with malformed middle ear structures. Clinical presentation includes microtia (small auricle), anotia (absent auricle), abnormally shaped or low-set ears, EAC atresia or stenosis, periauricular tags, pits or masses, craniofacial malformation, and conductive hearing loss (CHL) or mixed hearing loss. EAC malformations may be unilateral or bilateral (symmetric or asymmetric) and isolated or syndromic. Pointers to a syndromic cause or teratogenic insult include micrognathia, bilateral congenital external and middle ear malformation (CEMEM), and associated inner ear malformation. Micrognathia is associated with a low-set auricle; normal fetal mandibular growth is required for the auricle to ascend to its normal location.
EAC atresia is characterized by absence of the EAC and tympanic plate. Coronal CT images show a thick or thin bony and sometimes partly membranous plate at the expected location of the TM [ Fig. 10.14 ]. EAC stenosis is a narrowed EAC with a hypoplastic tympanic plate [ Fig. 10.14 ]. A stenotic EAC tends to trap debris that can, over time, lead to paradoxical EAC widening because of scalloping or erosion from keratosis obturans or EAC cholesteatoma, respectively. EAC atresia and stenosis are associated with deficiency of the manubrium of the malleus, the malleus being fused laterally to the atresia plate in EAC atresia. There is also variable malformation of the incus and stapes, sometimes with additional sites of ossicular fixation. The MEC ranges from near normal to severely hypoplastic. Congenital MEC cholesteatoma may occur in association, and results in a clinically occult erosive MEC opacity. It is also important to look for oval window stenosis or atresia, associated with stapedial malformation and an abnormal course of the FNC tympanic segment, coursing between the stapedial crura over the atretic oval window, over the promontory, or over the MEC floor. The mastoid FNC also descends more ventrally, sometimes over the atresia plate or into the temporomandibular joint (TMJ). Additional malformations include mastoid bone hypoplasia/decreased pneumatization, micrognathia/absent mandibular condyle, and hypoplastic zygomatic arches (eg, TCS, HFM).

Temporal bone findings in TCS (see micrognathia) include bilateral EAC atresia/stenosis, severe MEC hypoplasia/aplasia, rudimentary ossicles, oval window atresia, and poor/absent mastoid pneumatization. Variable inner ear malformations include flattened cochlear turns and malformed vestibules/SCCs. CEMEM occurs in a variety of other syndromes; CEMEM is unilateral in HFM, and bilateral and asymmetric in BOR (with anomalous dilated, Eustachian tubes).
Minor MEC and ossicular anomalies without EAC malformation occur less frequently. Isolated ossicular anomalies include alteration in size, shape, orientation, fusion, and/or fixation. A monopod stapes has a single strut in place of two crura. Congenital fusion of the malleus to the attic is termed a malleus bar. Isolated oval window stenosis or atresia is associated with stapedial and FNC anomalies as mentioned earlier. FNC dehiscence permits CN VII to protrude into the MEC. CN VII aplasia/hypoplasia is associated with various syndromes (eg, Moebius, CHARGE, and HFM). Congenital MEC cholesteatoma appears as a rounded white mass behind an intact TM. CT reveals a rounded mass ventral to or surrounding the malleus and abutting the promontory [ Fig. 10.14 ]. Bone erosion and growth into surrounding structures characterizes advanced disease. Congenital EAC cholesteatoma appears as a rounded erosive mass lateral to the TM.
Inner Ear Malformations
Inner ear anomalies present with SNHL, mixed hearing loss, disturbed balance, or with syndromic features affecting other organs. Genetic disorders are a significant cause of SNHL, as are CMV infection and prematurity (multifactorial). Imaging is sometimes helpful in suggesting a genetic or syndromic etiology and provides information that is useful for surgical planning and counseling. Following is a descriptive classification of inner ear malformations.
Vestibular Aqueduct Malformation
- 1.
LVA; large endolymphatic sac anomaly (LESA): usually with cochlear incomplete partition type II (IP-II) or modiolar deficiency
Cochlear Malformations
- 1.
Complete labyrinthine aplasia (Michel anomaly): absent inner ear structures
- 2.
Cochlear aplasia: absent cochlea, normal or malformed vestibule and SCC
- 3.
Cochlear hypoplasia: a small cochlea, usually less than turns, ± internal structure
- 4.
Common cavity malformation: cystic cavity (cochlea + vestibule + SCC)
- 5.
Cystic cochleovestibular malformation: globular cochlea, no internal architecture—IP-I; cochlea, vestibule, and lateral SCC form a bilobed cyst
- 6.
Cochlear IP-I: no internal cochlear architecture; normal or malformed vestibule and SCC
- 7.
Cochlear IP-II (Mondini anomaly): normal cochlear basal turn, deficient septation between plump middle and apical turns, deficient modiolus, LVA
- 8.
Cochlear modiolar deficiency: deficient cochlear modiolus, ± LVA
- 9.
Cochlear nerve and cochlear nerve aperture aplasia or hypoplasia: cochlear nerve canal < 0.7 mm wide or atretic; variable modiolar thickening; cochlear nerve hypoplasia/aplasia
Vestibular and Semicircular Canal Malformations
- 1.
Complete labyrinthine aplasia (Michel deformity): as described earlier
- 2.
Common cavity malformation: as described earlier
- 3.
Cystic cochleovestibular malformation: as described earlier
- 4.
Vestibular hypoplasia with SCC aplasia/hypoplasia: small vestibule; small/absent SCC
- 5.
Vestibule-SCC globular anomaly: dilated vestibule and lateral SCC form a single space
- 6.
SCC small bone island: small bone island between lateral SCC and vestibule
Internal Auditory Canal Malformations
- 1.
IAC aplasia: absent IAC; absent CNs VII and VIII
- 2.
IAC stenosis: narrowed IAC; variable CNs VII and VIII hypoplasia or aplasia
- 3.
IAC enlargement: large IAC; CNs VII and VIII usually normal
- 4.
IAC duplication: variable CNs VII and VIII hypoplasia or aplasia
Perilymph Fistula
- 1.
Communication between inner ear and middle ear cavity at the round or oval window
Genetic or Syndromic Inner Ear Anomalies.
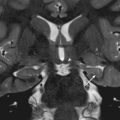
LVA is the most common inner ear malformation. Clinical presentation is fluctuating, progressive SNHL sometimes following relatively mild head trauma. Children with LVA are advised to avoid contact sports. CT reveals the flared LVA with a midpoint width of ≥1 mm and an opercular width ≥2 mm [ Fig. 10.15 ]. On reformats parallel to the plane of the superior SCC long axis, the LVA measures ≥1 mm in width. On thin-section, heavily T2W MR images, there is enlargement of the endolymphatic sac and duct lateral to the dura [ Fig. 10.15 ]. There is usually associated cochlear modiolar deficiency or IP-II (the cochlea resembles a baseball cap ) with variable enlargement of the vestibule and lateral SCC [ Fig. 10.15 ]. LVA is associated with a heritable genetic mutation that encodes for the pendrin protein, sometimes resulting in Pendred syndrome (LVA with thyroid organification defect leading to hypothyroidism and sometimes goiter).

BOR has a characteristic cochlear anomaly; the basal turn is tapered and the middle and apical turns are hypoplastic and offset anteriorly ( unwound appearance) [ Fig. 10.16 ]. There is also a funnel-shaped LVA, posterior SCC malformation, large/anomalous Eustachian tubes, and CEMEM. CHARGE syndrome (see choanal atresia) is characterized by hypoplasia of the vestibule and SCC hypoplasia/aplasia [ Fig. 10.16 ]. Other temporal bone findings include oval window atresia, ossicular malformation, absence/flattening of the apical/middle cochlear turns, atresia/stenosis of the cochlear nerve aperture, and funnel-shaped LVA. MRI shows variable deficiency of CNs VII and VIII. X-linked mixed hearing loss with stapes gusher affects boys and is associated with an increased risk for CSF gusher during attempted stapedectomy or cochleostomy. Imaging reveals a malformed, corkscrew-shaped cochlea without internal structure, with enlargement of the lateral IAC, and sometimes the vestibule and SCC [ Fig. 10.16 ]. SCC malformations most frequently involve the lateral SCC, may be isolated or syndromic, and are common in trisomy 21 and Apert syndrome, in which there is a small bone island and globular lateral SCC, or a lateral SCC-vestibule common cavity. Posterior SCC anomalies are seen in a subtype of Waardenburg syndrome and in Alagille syndrome.

Vascular Variants
The IJVs are often asymmetric in size, with the right side larger than the left. A high-riding jugular bulb is diagnosed on coronal CT images when its superior aspect protrudes above the IAC floor and is visible on axial images at the level of the cochlear basal turn [ Fig. 10.17 ]. A dehiscent jugular bulb can produce pulsatile tinnitus and appears as a bluish retrotympanic mass. On CT the jugular bulb protrudes through a bone defect into the posteroinferior MEC [ Fig. 10.17 ]. Jugular venous stenosis/atresia is associated with some craniofacial disorders such as syndromic craniosynostosis and achondroplasia. In these syndromes, regional emissary veins enlarge and provide collateral venous drainage. An aberrant ICA occurs because of segmental aplasia of the extracranial ICA, which is reconstituted by the external carotid artery (ECA) branches before rejoining the horizontal petrous ICA. Clinical presentation is pulsatile tinnitus with a red retrotympanic mass. The aberrant ICA courses lateral to the IJV and lies exposed within the MEC. A persistent stapedial artery arises from the petrous ICA, courses in proximity to the stapes, and enters the FNC before reconstituting the middle meningeal artery. The foramen spinosum is absent.

Neck and Oral Cavity
Normal Development and Anatomy
Head and neck structures arise from the branchial apparatus, consisting of paired branchial arches, branchial (or pharyngeal) pouches, branchial clefts (grooves), and branchial membranes. The branchial arches form along the lateral primitive pharynx. Each arch consists of a mesenchymal core (containing neural crest cells and arterial, neural, cartilaginous, ligamentous, and muscular elements). The arches are covered externally by ectoderm and internally by endoderm, and are separated from each other by the branchial clefts externally and the branchial pouches internally. The primitive mouth (stomodeum) arises from surface ectoderm in contact with the amniotic cavity externally. The oral tongue arises primarily from paired lingual mesenchymal proliferations derived from the first branchial arches. The foramen cecum is located in the midline along the posterior third of the tongue. The salivary glands begin as solid proliferations from epithelial buds.
The thyroid primordium is a focal endodermal thickening that arises between the first and second branchial pouches at the site that will become the foramen cecum. The primordium elongates caudally along a diverticulum that continues to develop into a long tract, termed the thyroglossal duct (TGD), and the caudally migrating primordial cells eventually divide into what will become the thyroid lobes and isthmus, with cells contributed from surrounding endoderm. The TGD (and thus path of migration of thyroid primordia) originates in the midline posterior tongue at a point termed the foramen cecum, continues caudally ventral to the hyoid bone, and then transiently loops just posterior to the body of the hyoid before continuing further inferiorly to the thyroid bed. The TGD normally involutes; however, the distal half of the TGD may persist, with the primordial thyroid cells in that location eventually becoming the pyramidal lobe. The thymus and inferior parathyroid glands originate from the third branchial pouch. The superior parathyroid glands arise from the fourth branchial pouch. The laryngotracheal groove and tracheoesophageal folds become the ventral laryngotracheal lumen and dorsal esophagus.
The neck is divided by the hyoid bone into suprahyoid and infrahyoid compartments. Two layers of fascia encompass the neck: the superficial and deep cervical fasciae. The deep cervical fascia in turn consists of superficial, middle, and deep layers. The fascial layers divide the suprahyoid neck into eight compartments (parapharyngeal, pharyngeal mucosal, masticator, parotid, carotid, retropharyngeal (RP), danger, and perivertebral spaces). The sternocleidomastoid muscle (SCM) divides the infrahyoid neck into anterior and posterior triangles. The layers of the deep cervical fascia further subdivide the infrahyoid neck into five major spaces that are continuous with corresponding spaces in the suprahyoid neck (carotid, visceral, posterior cervical, RP, and perivertebral spaces).
The lymphatic system of the neck consists of lymph nodes (LNs) and lymphoid tissue in the Waldeyer ring (the nasopharyngeal adenoid, paired palatine tonsils, and lingual tonsillar tissue). The adenoid becomes prominent within the nasopharynx by 2 to 3 years of age, then regresses during adolescence. If no adenoidal tissue is seen in a young child without prior adenoidectomy, the possibility of immunodeficiency should be considered. The cervical LNs occur in contiguous groups and are classified according to various systems. Parotid, RP, facial, and occipital LNs are named according to location. Level IA is submental LNs; level IB is submandibular LNs. Level II, III, and IV nodes are jugular chain LNs (cranial to caudal). Level V nodes are posterior triangle spinal accessory LNs; level VI nodes are infrahyoid LNs medial to the carotid arteries. Normal LNs are homogeneous, have a fatty hilum, and are oval.
The major head and neck vessels include the common carotid arteries (CCAs), each of which bifurcates into the external carotid artery (ECA) and ICA, and the external, anterior, and IJVs. The IJVs are often asymmetric, right larger than left, sometimes with ectasia in the supine position. The pterygoid venous plexus is sometimes prominent and larger on one side. Medialization of one or both ICAs may occur as an isolated or syndromic finding (eg, 22q11 deletion or velocardiofacial syndrome). This finding is important if pharyngeal or neck surgery is planned. The major nerves traversing the neck include CNs IX through XII, the sympathetic chain, and CN VII and branches of CN V.
The oral cavity contains the tongue, teeth, portions of the mandible, and the floor of the mouth inferiorly, which is bounded by the paired mylohyoid muscles. The mylohyoid muscles form a sling when viewed in the coronal place. Resting within the sling are the left and right sublingual spaces (within the floor of mouth); lateral and external to the sling are the left and right submandibular spaces (outside of the floor of mouth). Thus each sublingual space and the ipsilateral submandibular space are separated by the mylohyoid muscle. The major salivary glands consist of paired parotid, submandibular, and sublingual glands. Minor salivary glands also exist in many locations in the head and neck, including on the oral mucosa, in the floor of mouth, along the palate, and even in the sinonasal cavity. Most muscles of the suprahyoid neck attach to the mandible. The maxilla contains the maxillary sinuses.
Tornwaldt Cyst
Tornwaldt cyst is a developmental nasopharyngeal cyst that is usually an incidental finding. On imaging, it is sharply circumscribed, thin-walled, and located in the midline along the posterior nasopharynx. It is typically hyperintense on T2W MR, variable in signal on T1W MR, and does not enhance [ Fig. 10.18 ].

Branchial Apparatus Anomalies
Branchial anomalies are thought to arise due to remnants or incomplete obliteration of the branchial apparatus, or due to trapped epithelial rests. Branchial apparatus anomalies include cysts, sinus tracts (ectodermal or endodermal opening), fistulae (both openings) and aberrant tissue, and are classified according to the arch, cleft, or pouch of origin. Fistulae and sinuses, usually identified at birth because of drainage, are best imaged by CT, sometimes with a contrast-enhanced fistulogram. Branchial apparatus cysts (BAC) are more frequently diagnosed in older children and adults. Ultrasonography reveals an anechoic or hypoechoic thin-walled cyst. CT and MRI show an oval or round cyst with minimal, if any, peripheral enhancement. Wall thickening, enhancement, and surrounding edema suggest superimposed inflammation.
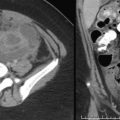
First BAC locations include the parotid region, periauricular soft tissues, EAC, MEC, or nasopharynx. A Work type I BAC is periauricular and Work type II is periparotid [ Fig. 10.19 ]. The differential diagnosis of first BAC includes dermoid cyst, LM, and necrotic adenopathy (eg, nontuberculous mycobacterial infection). The second BAC is the most common branchial anomaly. The usual location is at the mandibular angle, posterior to the submandibular gland, lateral to the ICA/IJV, and anterior to SCM (type II second BAC) [ Fig. 10.19 ]. Type I second BAC is deep to platysma, lateral to SCM. Type III second BAC protrudes between the ICA and ECA, and may extend to the lateral pharyngeal wall or skull base. Type IV (second pouch anomaly) is adjacent to the lateral pharyngeal wall. The differential diagnosis includes dermoid, LM, necrotic adenopathy, and laryngocele. The third BAC is in the upper posterior cervical space or lower anterior neck. Recurrent infrahyoid neck abscess or suppurative thyroiditis, particularly if it contains air, should raise the possibility of an underlying pyriform sinus tract [ Fig. 10.20 ]. This anomaly is thought to arise from the embryonal thymopharyngeal duct of the third branchial pouch. After resolution of inflammation, a contrast swallowing study may demonstrate the sinus tract. Other branchial anomalies include thymic [ Fig. 10.21 ] and parathyroid anomalies such as aberrant cervical thymus, thymic cysts, parathyroid cysts, aberrant parathyroid tissue, and thyroid anomalies (see later).